Gas Exchange and Ventilation–Perfusion Relationships in the Lung
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypothermia Brochure
Visit these websites for more water safety and hypothermia prevention in- formation. What is East Pierce Fire & Rescue Hypothermia? www.eastpiercefire.org Hypothermia means “low temperature”. Washington State Drowning When your body is exposed to cold tem- Prevention Coalition Hypothermia www.drowning-prevention.org perature, it tries to protect itself by keeping a normal body temperature of 98.6°F. It Children’s Hospital & tries to reduce heat loss by shivering and Regional Medical Center In Our Lakes moving blood from your arms and legs to www.seattlechildrens.org the core of your body—head, chest and and Rivers abdomen. Hypothermia Prevention, Recognition and Treatment www.hypothermia.org Stages of Hypothermia Boat Washington Mild Hypothermia www.boatwashington.org (Core body temperature of 98.6°— 93.2°F) Symptoms: Shivering; altered judg- ment; numbness; clumsiness; loss of Boat U.S. Foundation dexterity; pain from cold; and fast www.boatus.com breathing. Boat Safe Moderate Hypothermia www.boatsafe.com (Core body temperature of 93.2°—86°F) Symptoms: Semiconscious to uncon- scious; shivering reduced or absent; lips are blue; slurred speech; rigid n in muscles; appears drunk; slow Eve breathing; and feeling of warmth can occur. mer! Headquarters Station Sum Severe Hypothermia 18421 Old Buckley Hwy (Core body temperature below 86°F) Bonney Lake, WA 98391 Symptoms: Coma; heart stops; and clinical death. Phone: 253-863-1800 Fax: 253-863-1848 Email: [email protected] Know the water. Know your limits. Wear a life vest. By choosing to swim in colder water you Waters in Western Common Misconceptions Washington reduce your survival time. -

Job Hazard Analysis
Identifying and Evaluating Hazards in Research Laboratories Guidelines developed by the Hazards Identification and Evaluation Task Force of the American Chemical Society’s Committee on Chemical Safety Copyright 2013 American Chemical Society Table of Contents FOREWORD ................................................................................................................................................... 3 ACKNOWLEDGEMENTS ................................................................................................................................. 5 Task Force Members ..................................................................................................................................... 6 1. SCOPE AND APPLICATION ..................................................................................................................... 7 2. DEFINITIONS .......................................................................................................................................... 7 3. HAZARDS IDENTIFICATION AND EVALUATION ................................................................................... 10 4. ESTABLISHING ROLES AND RESPONSIBILITIES .................................................................................... 14 5. CHOOSING AND USING A TECHNIQUE FROM THIS GUIDE ................................................................. 17 6. CHANGE CONTROL .............................................................................................................................. 19 7. ASSESSING -

Gas Exchange
Gas exchange Gas exchange occurs as a result of respiration, when carbon dioxide is excreted and oxygen taken up, and photosynthesis, when oxygen is excreted and carbon dioxide is taken up. The rate of gas exchange is affected by: • the area available for diffusion • the distance over which diffusion occurs • the concentration gradient across the gas exchange surface • the speed with which molecules diffuse through membranes. Efficient gas exchange systems must: • have a large surface area to volume ratio • be thin • have mechanisms for maintaining steep concentration gradients across themselves • be permeable to gases. Single-celled organisms are aquatic and their cell surface membrane has a sufficiently large surface area to volume ratio to act as an efficient gas exchange surface. In larger organisms, permeable, thin, flat structures have all the properties of efficient gas exchange surfaces but need water to prevent their dehydration and give them mechanical support. Since the solubility of oxygen in water is low, organisms that obtain their oxygen from water can maintain only a low metabolic rate. In small and thin organisms, the distance from gas exchange surface to the inside of the organism is short enough for diffusion of gases to be efficient. Diffusion gradients are maintained because gases are continually used up or produced. In larger organisms, simple diffusion is not an efficient way of transporting gases between cells in the body and the gas exchange surface. In many animals a blood circulatory system carries gases to and from the gas exchange surface. The gas-carrying capacity of the blood is increased by respiratory pigments, such as haemoglobin. -

Mechanisms of Pulmonary Gas Exchange Abnormalities During Experimental Group B Streptococcal Infusion
003 I -3998/85/1909-0922$02.00/0 PEDIATRIC RESEARCH Vol. 19, No. 9, I985 Copyright 0 1985 International Pediatric Research Foundation, Inc. Printed in (I.S. A. Mechanisms of Pulmonary Gas Exchange Abnormalities during Experimental Group B Streptococcal Infusion GREGORY K. SORENSEN, GREGORY J. REDDING, AND WILLIAM E. TRUOG ABSTRACT. Group B streptococcal sepsis in newborns obtained from GBS (5, 6). Arterial Poz fell by 9 torr in association produces pulmonary arterial hypertension and hypoxemia. with the increase in pulmonary arterial pressure (4). In contrast, The purpose of this study was to investigate the mecha- the neonatal piglet infused with GBS demonstrated both pul- nisms by which hypoxemia occurs. Ten anesthetized, ven- monary arterial hypertension and profound arterial hypoxemia tilated piglets were infused with 2 x lo9 colony forming (7). These results suggest that the neonatal pulmonary vascula- unitstkg of Group B streptococci over a 30-min period. ture may respond to bacteremia differently from that of adults. Pulmonary arterial pressure rose from 14 ? 2.8 to 38 ? The relationship between Ppa and the matching of alveolar 6.7 torr after 20 min of the bacterial infusion (p< 0.01). ventilation and pulmonary perfusion, a major determinant of During the same period, cardiac output fell from 295 to arterial oxygenation during room air breathing (8), has not been 184 ml/kg/min (p< 0.02). Arterial Po2 declined from 97 studied in newborns. The predictable rise in Ppa with an infusion 2 7 to 56 2 11 torr (p< 0.02) and mixed venous Po2 fell of group B streptococcus offers an opportunity to delineate the from 39.6 2 5 to 28 2 8 torr (p< 0.05). -

CARBON MONOXIDE: the SILENT KILLER Information You Should
CARBON MONOXIDE: THE SILENT KILLER Information You Should Know Carbon monoxide is a silent killer that can lurk within fossil fuel burning household appliances. Many types of equipment and appliances burn different types of fuel to provide heat, cook, generate electricity, power vehicles and various tools, such as chain saws, weed eaters and leaf blowers. When these units operate properly, they use fresh air for combustion and vent or exhaust carbon dioxide. When fresh air is restricted, through improper ventilation, the units create carbon monoxide, which can saturate the air inside the structure. Carbon Monoxide can be lethal when accidentally inhaled in concentrated doses. Such a situation is referred to as carbon monoxide poisoning. This is a serious condition that is a medical emergency that should be taken care of right away. What Is It? Carbon monoxide, often abbreviated as CO, is a gas produced by burning fossil fuel. What makes it such a silent killer is that it is odorless and colorless. It is extremely difficult to detect until the body has inhaled a detrimental amount of the gas, and if inhaled in high concentrations, it can be fatal. Carbon monoxide causes tissue damage by blocking the body’s ability to absorb enough oxygen. In fact, poisoning from this gas is one of the leading causes of unintentional death from poison. Common Sources of CO Kerosene or fuel-based heaters Fireplaces Gasoline powered equipment and generators Charcoal grills Automobile exhaust Portable generators Tobacco smoke Chimneys, furnaces, and boilers Gas water heaters Wood stoves and gas stoves Properly installed and maintained appliances are safe and efficient. -

The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board
The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board Introduction • Nitrogen makes up 78% of the air we breath; because of this it is often assumed that nitrogen is not hazardous. • However, nitrogen is safe to breath only if it is mixed with an appropriate amount of oxygen. • Additional nitrogen (lower oxygen) cannot be detected by the sense of smell. Introduction • Nitrogen is used commercially as an inerting agent to keep material free of contaminants (including oxygen) that may corrode equipment, present a fire hazard, or be toxic. • A lower oxygen concentration (e.g., caused by an increased amount of nitrogen) can have a range of effects on the human body and can be fatal if if falls below 10% Effects of Oxygen Deficiency on the Human Body Atmospheric Oxygen Concentration (%) Possible Results 20.9 Normal 19.0 Some unnoticeable adverse physiological effects 16.0 Increased pulse and breathing rate, impaired thinking and attention, reduced coordination 14.0 Abnormal fatigue upon exertion, emotional upset, faulty coordination, poor judgment 12.5 Very poor judgment and coordination, impaired respiration that may cause permanent heart damage, nausea, and vomiting <10 Inability to move, loss of consciousness, convulsions, death Source: Compressed Gas Association, 2001 Statistics on Incidents CSB reviewed cases of nitrogen asphyxiation that occurred in the US between 1992 and 2002 and determined the following: • 85 incidents of nitrogen asphyxiation resulted in 80 deaths and 50 injuries. • The majority of -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

Gas-Liquid Hollow Fiber Membrane Contactors for Different Applications
Review Gas-Liquid Hollow Fiber Membrane Contactors for Different Applications Stepan D. Bazhenov 1,*, Alexandr V. Bildyukevich 2 and Alexey V. Volkov 1 1 A.V. Topchiev Institute of Petrochemical Synthesis, Russian Academy of Sciences, Moscow 119991, Russia; [email protected] 2 Institute of Physical Organic Chemistry, National Academy of Sciences of Belarus, Minsk 220072, Belarus; [email protected] * Correspondence: [email protected]; Tel.: +7-495-647-5927 (ext. 202) Received: 14 September 2018; Accepted: 2 October 2018; Published: 10 October 2018 Abstract: Gas-liquid membrane contactors that were based on hollow fiber membranes are the example of highly effective hybrid separation processes in the field of membrane technology. Membranes provide a fixed and well-determined interface for gas/liquid mass transfer without dispensing one phase into another while their structure (hollow fiber) offers very large surface area per apparatus volume resulted in the compactness and modularity of separation equipment. In many cases, stated benefits are complemented with high separation selectivity typical for absorption technology. Since hollow fiber membrane contactors are agreed to be one of the most perspective methods for CO2 capture technologies, the major reviews are devoted to research activities within this field. This review is focused on the research works carried out so far on the applications of membrane contactors for other gas-liquid separation tasks, such as water deoxygenation/ozonation, air humidity control, ethylene/ethane separation, etc. A wide range of materials, membranes, and liquid solvents for membrane contactor processes are considered. Special attention is given to current studies on the capture of acid gases (H2S, SO2) from different mixtures. -

Effects of Anaesthesia Techniques and Drugs on Pulmonary Function
Review Article Effects of anaesthesia techniques and drugs on pulmonary function Address for correspondence: Vijay Saraswat Dr. Vijay Saraswat, Department of Anaesthesiology, Apollo Hospitals, Nashik, Maharashtra, India Apollo Hospitals, Nashik, Maharashtra, India. E‑mail: drvsaraswat@gmail. ABSTRACT com The primary task of the lungs is to maintain oxygenation of the blood and eliminate carbon dioxide through the network of capillaries alongside alveoli. This is maintained by utilising ventilatory reserve capacity and by changes in lung mechanics. Induction of anaesthesia impairs pulmonary functions by the loss of consciousness, depression of reflexes, changes in rib cage and haemodynamics. All drugs used during anaesthesia, including inhalational agents, affect pulmonary functions directly by acting on respiratory system or indirectly through their actions on other systems. Volatile anaesthetic agents have more pronounced effects on pulmonary functions compared to intravenous induction agents, leading to hypercarbia and hypoxia. The posture of the patient also leads to major changes in pulmonary functions. Anticholinergics and neuromuscular blocking agents have little effect. Analgesics and Access this article online sedatives in combination with volatile anaesthetics and induction agents may exacerbate Website: www.ijaweb.org their effects. Since multiple agents are used during anaesthesia, ultimate effect may be DOI: 10.4103/0019‑5049.165850 different from when used in isolation. Literature search was done using MeSH key words ‘anesthesia’, -
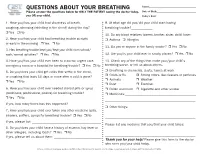
QUESTIONS ABOUT YOUR BREATHING Name:______Please Answer the Questions Below for ONLY the PATIENT Seeing the Doctor Today, Date of Birth:______You OR Your Child
QUESTIONS ABOUT YOUR BREATHING Name:_____________________________________ Please answer the questions below for ONLY THE PATIENT seeing the doctor today, Date of Birth:_______________________________ you OR your child. Today’s Date:_______________________________ 1. Have you/has your child had shortness of breath, 9. At what age did you/did your child start having coughing, wheezing (whistling in the chest) during the day? breathing trouble?_____________ r Yes r No 10. Do any blood relatives (parent, brother, sister, child) have: 2. Have you/has your child had breathing trouble at night r Asthma r Allergies or early in the morning r Yes r No 11. Do you or anyone in the family smoke? r Yes r No 3. Has breathing trouble kept you/kept your child from school/ work/normal activities? r Yes r No 12. Are you/is your child ever in smoky places? r Yes r No 4. Have you/has your child ever been to a doctor, urgent care, 13. Check any of the things that make your/your child’s emergency room or a hospital for breathing trouble? r Yes r No breathing worse, or tell us about others. 5. Do you/does your child get colds that settle in the chest, r Breathing in chemicals, dusts, fumes at work r Colds or flu r Strong odors, like cleaners or perfumes or coughing that lasts 10 days or more after a cold is gone? r Animals r Weather r Yes r No r Dust r Exercise 6. Have you/has your child ever needed steroid pills or syrup r Pollen and mold r Cigarette and other smoke (prednisone, prednisolone, prelone) for breathing trouble? r Medicines:___________________________________________ r Yes r No _______________________________________________________ If yes, how many times has this happened? ___________________ r Other things: 7. -

Respiratory System
Respiratory System 1 Respiratory System 2 Respiratory System 3 Respiratory System 4 Respiratory System 5 Respiratory System 6 Respiratory System 7 Respiratory System 8 Respiratory System 9 Respiratory System 10 Respiratory System 11 Respiratory System • Pulmonary Ventilation 12 Respiratory System 13 Respiratory System 14 Respiratory System • Measuring of Lung Function œ Compliance œ the ease at which the lungs and thoracic wall can be expanded œ if reduced it is more difficult to inflate the lungs œ causes: • Damaged lung tissue • Fluid within lung tissue • Decrease in pulmonary surfactant • Anything that impedes lung expansion or contraction œ Respiratory Volumes and Capacities will be covered in Lab œ 15 Respiratory System • Exchange of Oxygen and Carbon Dioxide œ Charles‘ Law œ the volume of a gas is directly proportional to the absolute temperature, assuming the pressure remains constant As gases enter the lung they warm and expand, increasing lung volume œ Dalton‘s Law œ each gas of a mixture of gases exerts its own pressure as if all the other gases were not present œ Henry‘s Law œ the quantity of a gas that will dissolve in a liquid is proportional to the partial pressure of the gas and its solubility coefficient, when the temperature remains constant 16 Respiratory System • External and Internal Respiration 17 Respiratory System • Transport of Oxygen and Carbon Dioxide by the Blood œ Oxygen Transport • 1.5% dissolved in plasma • 98.5% carried with Hbinside of RBC‘s as oxyhemoglobin œ Hbœ made up of protein portion called the globinportion -

HANDOUT #1 CONCEPT INTRODUCTION PRESENTATION: PERFUSION Topic Description Definition of Perfusion the Passage of Oxygenated Capi
HANDOUT #1 CONCEPT INTRODUCTION PRESENTATION: PERFUSION Topic Description Definition of Perfusion The passage of oxygenated capillary blood through body tissues. Peripheral perfusion is passage (flow) of blood to the extremities of the body. Central perfusion is passage (flow) of blood to major body organs, including the heart and lungs. Scope of Perfusion Perfusion can be viewed on a continuum as adequate on one end and inadequate, decreased, or impaired on the other. Decreased Perfusion can range from minimal to severe. Ischemia refers to decreased Perfusion, while infarction is complete tissue death due to severe decreased Perfusion. Risk Factors/Populations at Risk for Examples of risk factors or populations at risk Impaired Perfusion for impaired Perfusion can be categorized as modifiable (can be changed) and nonmodifiable (cannot be changed) Modifiable factors include: • Obesity • Lack of physical activity/sedentary lifestyle • Smoking Nonmodifiable factors include age, gender, and race/ethnicity. Groups at risk for impaired Perfusion include those who are of advanced age (due to less elastic arterial vessels as a result of aging) and those who are African American and Hispanic. These racial/ethnic groups are most at risk for chronic diseases that can affect Perfusion such as diabetes mellitus, hypertension, hyperlipidemia, and peripheral vascular disease. The cause of these variations is not known, but dietary and environmental factors may contribute to the higher incidence of chronic disease in these groups. Newborns and infants who have congenital heart anomalies are also at risk for impaired central Perfusion. Many of these defects can be surgically repaired to regain adequate Perfusion. Physiologic Consequences of Impaired Consequences of impaired Perfusion vary Perfusion depending on the degree of impairment.