Ectopic Insulinoma: Case Report Mengqing Sun1, Yaping Luo2, Yan You3, Xianlin Han1 , Yupei Zhao1, Xianlin Han1* and Yupei Zhao1*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E
Peer Reviewed PRACTICAL ONCOLOGY CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E. Burgess, DVM, Diplomate ACVIM (Oncology) Tufts University An insulinoma is a malignant pancreatic tumor that DIAGNOSIS inappropriately secretes excessive insulin, resulting in Aside from a histologic confirmation of insulinoma, profound hypoglycemia.1 no currently available diagnostic test provides a de- Pancreatic tumors are classified as: finitive diagnosis of insulinoma. Existing techniques • Exocrine, which includes adenocarcinomas of may help increase suspicion for an insulin-secreting ductular or acinar origin tumor but, with most diagnostic testing, it is im- • Endocrine, which arise from the islets of perative to interpret all results in the context of the Langerhans. coexisting clinical signs. Insulinomas are functional neuroendocrine tumors that originate in the beta cells of the islets Differential Diagnosis of Langerhans.1 A complete work-up, including careful patient history, physical examination, bloodwork, and PRESENTATION diagnostic imaging tests, should be performed to Signalment rule out other causes of hypoglycemia, such as Any breed of dog can be affected, but large sepsis, hepatic failure, adrenal cortical insufficiency, breeds tend to be overrepresented.1 While, in toxin ingestion, and other forms of neoplasia. humans, insulinomas affect females far more frequently than males, there is no apparent sex Laboratory Tests predilection in dogs.1-3 Dogs also commonly Blood Glucose present with a malignant variant, while humans A simple fasting blood glucose level of less than often have a benign adenoma (80%).1 Insulino- 40 mg/dL can suggest hyperinsulinemia, although ma is rare in cats.4 careful monitoring of a fasted dog with suspected insulinoma is strongly recommended due to high Clinical Signs risk for seizure activity. -

Primary Hepatic Neuroendocrine Carcinoma: Report of Two Cases and Literature Review
The Jackson Laboratory The Mouseion at the JAXlibrary Faculty Research 2018 Faculty Research 3-1-2018 Primary hepatic neuroendocrine carcinoma: report of two cases and literature review. Zi-Ming Zhao The Jackson Laboratory, [email protected] Jin Wang Ugochukwu C Ugwuowo Liming Wang Jeffrey P Townsend Follow this and additional works at: https://mouseion.jax.org/stfb2018 Part of the Life Sciences Commons, and the Medicine and Health Sciences Commons Recommended Citation Zhao, Zi-Ming; Wang, Jin; Ugwuowo, Ugochukwu C; Wang, Liming; and Townsend, Jeffrey P, "Primary hepatic neuroendocrine carcinoma: report of two cases and literature review." (2018). Faculty Research 2018. 71. https://mouseion.jax.org/stfb2018/71 This Article is brought to you for free and open access by the Faculty Research at The ousM eion at the JAXlibrary. It has been accepted for inclusion in Faculty Research 2018 by an authorized administrator of The ousM eion at the JAXlibrary. For more information, please contact [email protected]. Zhao et al. BMC Clinical Pathology (2018) 18:3 https://doi.org/10.1186/s12907-018-0070-7 CASE REPORT Open Access Primary hepatic neuroendocrine carcinoma: report of two cases and literature review Zi-Ming Zhao1,2*† , Jin Wang3,4,5†, Ugochukwu C. Ugwuowo6, Liming Wang4,8* and Jeffrey P. Townsend2,7* Abstract Background: Primary hepatic neuroendocrine carcinoma (PHNEC) is extremely rare. The diagnosis of PHNEC remains challenging—partly due to its rarity, and partly due to its lack of unique clinical features. Available treatment options for PHNEC include surgical resection of the liver tumor(s), radiotherapy, liver transplant, transcatheter arterial chemoembolization (TACE), and administration of somatostatin analogues. -

Neuroendocrine Tumors of the Pancreas (Including Insulinoma, Gastrinoma, Glucogacoma, Vipoma, Somatostatinoma)
Neuroendocrine tumors of the pancreas (including insulinoma, gastrinoma, glucogacoma, VIPoma, somatostatinoma) Neuroendocrine pancreatic tumors (pancreatic NETs or pNETs) account for about 3% of all primary pancreatic tumors. They develop in neuroendocrine cells called islet cells. Neuroendocrine tumors of the pancreas may be nonfunctional (not producing hormones) or functional (producing hormones). Most pNETs do not produce hormones and, as a result, these tumors are diagnosed incidentally or after their growth causes symptoms such as abdominal pain, jaundice or liver metastasis. pNETs that produce hormones are named according to the type of hormone they produce and / or clinical manifestation: Insulinoma - An endocrine tumor originating from pancreatic beta cells that secrete insulin. Increased insulin levels in the blood cause low glucose levels in blood (hypoglycemia) with symptoms that may include sweating, palpitations, tremor, paleness, and later unconsciousness if treatment is delayed. These are usually benign and tend to be small and difficult to localize. Gastrinoma - a tumor that secretes a hormone called gastrin, which causes excess of acid secretion in the stomach. As a result, severe ulcerative disease and diarrhea may develop. Most gastrinomas develop in parts of the digestive tract that includes the duodenum and the pancreas, called "gastrinoma triangle". These tumors have the potential to be malignant. Glucagonoma is a rare tumor that secretes the hormone glucagon, which may cause a typical skin rash called migratory necrolytic erythema, elevated glucose levels, weight loss, diarrhea and thrombotic events. VIPoma - a tumor that secretes Vasoactive peptide (VIP) hormone causing severe diarrhea. The diagnosis is made by finding a pancreatic neuroendocrine tumor with elevated VIP hormone in the blood and typical clinical symptoms. -

What Is a Gastrointestinal Carcinoid Tumor?
cancer.org | 1.800.227.2345 About Gastrointestinal Carcinoid Tumors Overview and Types If you have been diagnosed with a gastrointestinal carcinoid tumor or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Gastrointestinal Carcinoid Tumor? Research and Statistics See the latest estimates for new cases of gastrointestinal carcinoid tumor in the US and what research is currently being done. ● Key Statistics About Gastrointestinal Carcinoid Tumors ● What’s New in Gastrointestinal Carcinoid Tumor Research? What Is a Gastrointestinal Carcinoid Tumor? Gastrointestinal carcinoid tumors are a type of cancer that forms in the lining of the gastrointestinal (GI) tract. Cancer starts when cells begin to grow out of control. To learn more about what cancer is and how it can grow and spread, see What Is Cancer?1 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 To understand gastrointestinal carcinoid tumors, it helps to know about the gastrointestinal system, as well as the neuroendocrine system. The gastrointestinal system The gastrointestinal (GI) system, also known as the digestive system, processes food for energy and rids the body of solid waste. After food is chewed and swallowed, it enters the esophagus. This tube carries food through the neck and chest to the stomach. The esophagus joins the stomachjust beneath the diaphragm (the breathing muscle under the lungs). The stomach is a sac that holds food and begins the digestive process by secreting gastric juice. The food and gastric juices are mixed into a thick fluid, which then empties into the small intestine. -

Liver, Gallbladder, Bile Ducts, Pancreas
Liver, gallbladder, bile ducts, pancreas Coding issues Otto Visser May 2021 Anatomy Liver, gallbladder and the proximal bile ducts Incidence of liver cancer in Europe in 2018 males females Relative survival of liver cancer (2000 10% 15% 20% 25% 30% 35% 40% 45% 50% 0% 5% Bulgaria Latvia Estonia Czechia Slovakia Malta Denmark Croatia Lithuania N Ireland Slovenia Wales Poland England Norway Scotland Sweden Netherlands Finland Iceland Ireland Austria Portugal EUROPE - Germany 2007) Spain Switzerland France Belgium Italy five year one year Liver: topography • C22.1 = intrahepatic bile ducts • C22.0 = liver, NOS Liver: morphology • Hepatocellular carcinoma=HCC (8170; C22.0) • Intrahepatic cholangiocarcinoma=ICC (8160; C22.1) • Mixed HCC/ICC (8180; TNM: C22.1; ICD-O: C22.0) • Hepatoblastoma (8970; C22.0) • Malignant rhabdoid tumour (8963; (C22.0) • Sarcoma (C22.0) • Angiosarcoma (9120) • Epithelioid haemangioendothelioma (9133) • Embryonal sarcoma (8991)/rhabdomyosarcoma (8900-8920) Morphology*: distribution by sex (NL 2011-17) other other ICC 2% 3% 28% ICC 56% HCC 41% HCC 70% males females * Only pathologically confirmed cases Liver cancer: primary or metastatic? Be aware that other and unspecified morphologies are likely to be metastatic, unless there is evidence of the contrary. For example, primary neuro-endocrine tumours (including small cell carcinoma) of the liver are extremely rare. So, when you have a diagnosis of a carcinoid or small cell carcinoma in the liver, this is probably a metastatic tumour. Anatomy of the bile ducts Gallbladder -
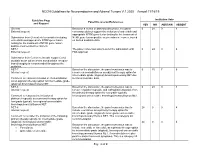
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19 Guideline Page Institution Vote Panel Discussion/References and Request YES NO ABSTAIN ABSENT General Based on a review of data and discussion, the panel 0 24 0 4 External request: consensus did not support the inclusion of entrectinib and appropriate NTRK gene fusion testing for the treatment of Submission from Genentech to consider including NTRK gene fusion-positive neuroendocrine cancer, based entrectinib and appropriate NTRK gene fusion on limited available data. testing for the treatment of NTRK gene fusion- positive neuroendocrine cancers. NET-1 The panel consensus was to defer the submission until 0 24 0 4 External request: FDA approval. Submission from Curium to include copper Cu 64 dotatate as an option where somatostatin receptor- based imaging is recommended throughout the guideline. NET-7 Based on the discussion, the panel consensus was to 0 15 7 6 Internal request: remove chemoradiation as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET due Comment to reassess inclusion of chemoradiation to limited available data. as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET. NET-8 Based on the discussion, the panel consensus was to 0 24 0 4 Internal request: remove cisplatin/etoposide and carboplatin/etoposide from the primary therapy option for low grade (typical), Comment to reassess the inclusion of locoregional unresectable bronchopulmonary/thymus NET. platinum/etoposide as a primary therapy option for low grade (typical), locoregional unresectable bronchopulmonary/thymus NET. NET-8 Based on the discussion, the panel consensus was to 24 0 0 4 Internal request: include everolimus as a primary therapy option for intermediate grade (atypical), locoregional unresectable Comment to consider the inclusion of the following bronchopulmonary/thymus NET. -

A New Theranostic Paradigm for Advanced Thyroid Cancer
INVITED PERSPECTIVES A New Theranostic Paradigm for Advanced Thyroid Cancer David A. Pattison1,2, Benjamin Solomon3,4, and Rodney J. Hicks1,4 1Centre for Cancer Imaging, Peter MacCallum Cancer Centre, Melbourne, Victoria, Australia; 2Endocrinology Service, Peter MacCallum Cancer Centre, Melbourne, Victoria, Australia; 3Department of Medical Oncology, Peter MacCallum Cancer Centre, Melbourne, Victoria, Australia; and 4Sir Peter MacCallum Department of Oncology, University of Melbourne, Parkville, Victoria, Australia Differentiation status and metabolic reprogramming are increas- The successful use of 131I as a systemic treatment of a patient ingly being recognized as determinants of imaging phenotype. In with metastatic thyroid cancer was first reported in 1948 (1). This contrast to well-differentiated tumors, which are reliant on mitochon- agent has subsequently become firmly established as part of the treat- drial oxidative phosphorylation to generate the energy needed for ment of high-risk thyroid cancer and especially for metastatic dis- cellular processes, poorly differentiated cancer cells depend on the ease. There has been an evolution in the quality of assessment of the inefficient mechanism of aerobic glycolysis—the Warburg effect. distribution of radioactive iodine (RAI) within the body, progressing Notably, Hurthle cell (or oncocytic) tumors, both benign and malig- 18 from Geiger–Muller¨ counting to imaging, first with the rectilinear nant, are generally characterized by intense F-FDG avidity represent- scanning and then with the g-camera. The physical characteristics ing inherent constitutive activation of glycolytic pathways (6). Loss of 123I as a diagnostic tracer compared with 131I further improved of the mitochondrial respiratory chain complex I has been shown to imaging by facilitating higher quality SPECT and SPECT/CT. -

Rising Incidence of Neuroendocrine Tumors
Rising Incidence of Neuroendocrine Tumors Dasari V, Yao J, et al. JAMA Oncology 2017 S L I D E 1 Overview Pancreatic Neuroendocrine Tumors • Tumors which arise from endocrine cells of the pancreas • 5.6 cases per million – 3% of pancreatic tumors • Median age at diagnosis 60 years • More indolent course compared to adenocarcinoma – 10-year overall survival 40% • Usually sporadic but can be associated with hereditary syndromes – Core genetic pathways altered in sporadic cases • DNA damage repair (MUTYH) Chromatin remodeling (MEN1) • Telomere maintenance (MEN1, DAXX, ATRX) mTOR signaling – Hereditary: 17% of patients with germline mutation Li X, Wang C, et al. Cancer Med 2018 Scarpa A, Grimond S, et al. NatureS L I2017 D E 2 Pathology Classification European American Joint World Health Organization Neuroendocrine Committee on Cancer (WHO) Tumor Society (AJCC) (ENETS) Grade Ki-67 Mitotic rt TNM TNM T1: limit to pancreas, <2 cm T1: limit to pancreas, ≦2 cm T2: limit to pancreas, 2-4 cm T2: >limit to pancreas, 2 cm T3: limit to pancreas, >4 cm, T3: beyond pancreas, no celiac or Low ≤2% <2 invades duodenum, bile duct SMA T4: beyond pancreas, invasion involvement adjacent organs or vessels T4: involves celiac or SMA N0: node negative No: node negative Intermed 3-20% 2-20 N1: node positive N1: node positive M0: no metastases M0: no metastases High >20% >20 M1: metastases M1: metastases S L I D E 3 Classification Based on Functionality • Nonfunctioning tumors – No clinical symptoms (can still produce hormone) – Accounts for 40% of tumors – 60-85% -

Primary Neuroendocrine Neoplasms of the Kidney, a Distinct Entity but Classifiable- Like the Gastroenteropancreatic Neuroendocrine Neoplasms
C-60 Primary Neuroendocrine Neoplasms of the Kidney, A Distinct Entity but Classifiable- Like the Gastroenteropancreatic Neuroendocrine Neoplasms Manik Amin1; Deyali Chatterjee2 1Washington University in St Louis; 2Washington University School of Medicine BACKGROUND: Primary neuroendocrine neoplasms of the kidney are a distinct and rare entity, but classifiable-like the gastroenteropancreatic neuroendocrine neoplasms. Due to rarity of these tumors, not much is known about histopathology and behaviors of these tumors. We attempted to review pathology of primary kidney neuroendocrine tumor patients at our institution. METHODS: Retrospective chart review identified 8 primary kidney neuroendocrine tumors from Siteman Cancer Registry database from 1/1/2000 until 1/1/2018. Pathology review was done for all the patients to confirm their diagnosis and other pathological features. RESULTS: In our cohort, we identified eight cases of neuroendocrine neoplasms of the kidney. Three of the cases were poorly differentiated neuroendocrine carcinoma. All cases of well-differentiated neuroendocrine tumor (either grade 1 or grade 2) were identified in females (age range 44 – 60). All the tumors characteristically extended to the perirenal fat. These tumors showed diffuse positivity for synaptophysin, variable positivity for chromogranin, and did not stain for markers specific for renal differentiation (PAX-8). The growth pattern in well differentiated neuroendocrine tumors is predominantly trabeculated, but a diffuse plasmacytoid growth is also noted, which is unusual in gastroenteropancreatic neuroendocrine neoplasms. Two patients had Primary tumor measuring 9 cm and 14 cm respectively also presented with positive lymph nodes and lymphovascular invasion developed metastatic disease in 2 years. NANETS 2019 Symposium Abstracts | 175 CONCLUSION: Primary kidney neuroendocrine tumors are very rare. -

Solitary Duodenal Metastasis from Renal Cell Carcinoma with Metachronous Pancreatic Neuroendocrine Tumor: Review of Literature with a Case Discussion
Published online: 2021-05-24 Practitioner Section Solitary Duodenal Metastasis from Renal Cell Carcinoma with Metachronous Pancreatic Neuroendocrine Tumor: Review of Literature with a Case Discussion Abstract Saphalta Baghmar, Renal cell cancinoma (RCC) is a unique malignancy with features of late recurrences, metastasis S M Shasthry1, to any organ, and frequent association with second malignancy. It most commonly metastasizes Rajesh Singla, to the lungs, bones, liver, renal fossa, and brain although metastases can occur anywhere. RCC 2 metastatic to the duodenum is especially rare, with only few cases reported in the literature. Herein, Yashwant Patidar , 3 we review literature of all the reported cases of solitary duodenal metastasis from RCC and cases Chhagan B Bihari , of neuroendocrine tumor (NET) as synchronous/metachronous malignancy with RCC. Along with S K Sarin1 this, we have described a unique case of an 84‑year‑old man who had recurrence of RCC as solitary Departments of Medical duodenal metastasis after 37 years of radical nephrectomy and metachronous pancreatic NET. Oncology, 1Hepatology, 2Radiology and 3Pathology, Keywords: Late recurrence, pancreatic neuroendocrine tumor, renal cell carcinoma, second Institute of Liver and Biliary malignancy, solitary duodenal metastasis Sciences, New Delhi, India Introduction Case Presentation Renal cell carcinoma (RCC) is unique An 84‑year‑old man with a medical history to have many unusual features such as notable for hypertension and RCC, 37 years metastasis to almost every organ in the body, postright radical nephrectomy status, late recurrences, and frequent association presented to his primary care physician with second malignancy. The most common with fatigue. When found to be anemic, sites of metastasis are the lung, lymph he was treated with iron supplementation nodes, liver, bone, adrenal glands, kidney, and blood transfusions. -

Possible Functional Regression of Insulinoma with Prolonged Octreotide C E H Craig, I W Gallen
623 Postgrad Med J: first published as 10.1136/pmj.78.924.623 on 1 October 2002. Downloaded from CASE REPORT Possible functional regression of insulinoma with prolonged octreotide C E H Craig, I W Gallen ............................................................................................................................. Postgrad Med J 2002;78:623–624 A 75 year old woman was treated for over three years with the somatostatin analogue, octreotide for an insulinoma. She had presented in a hypoglycaemic coma. C-peptide and insulin concentrations were both raised and an area of increased vascularity within the pancreas was shown by angiography. No lesion was found at laparotomy and no resection was performed. After over three years of octreotide treatment it was withdrawn for a week. Her insulin and C-peptide concentrations were greatly reduced at this time and remained so. he somatostatin analogue, octreotide inhibits secretion of a wide variety of peptide hormones including insulin.1 It Thas been successfully used in previous cases of insuli- noma. Other well differentiated endocrine tumours have Figure 1 Coeliac angiogram; area of increased vascularity is reduced in size when treated with drugs that inhibit hormone indicated by arrows. production—for example, bromocriptine in prolactinoma.2 Here we report a case of markedly reduced insulin production from an insulinoma, once octreotide treatment was with- concentration excluded hypothyroidism. Her admission insu- drawn. lin and C-peptide levels were later reported as 438.7 pmol/l (21.5–115.0) and 2810 pmol/l (180–630) respectively. A urinary sulphonylurea screen was negative. As her C-peptide CASE REPORT levels were raised, the presence of exogenous insulin was also http://pmj.bmj.com/ A 75 year old woman presented, unconscious, after a collapse excluded. -

Insulinoma Presenting As New-Onset Psychiatric Symptoms Introduction
Insulinoma Presenting as New-Onset Psychiatric Symptoms Lauren Cusick, PA-S, Peter Sandor, MHS, PA-C Quinnipiac University Physician Assistant Program Introduction Case Description Discussion • Insulinomas are rare insulin-secreting neuroendocrine History Physical Exam Diagnostic Results • Surgery was performed and an encapsulated 1.2 x 1.4 cm tumors that occur in approximately four out of a million • A 27-year-old African American • Figure 1 displays the patient’s recorded blood tumor was removed from the uncinate process toward the people each year.1 • Vitals in emergency department: male presented to the emergency - Temperature: 98.2℉ glucose levels. During this time, he was placed on superior aspect of the pancreatic head. Pathology later department with altered mental a 10% dextrose infusion due to continued confirmed that this tumor was an insulinoma. • Observational studies show that they occur more often in - Pulse: 62 bpm status following a syncopal event at - Blood pressure: 134/93 mm Hg hypoglycemia. women and those over the age of 50.2,3 home characterized by seizure-like - Respiratory rate: 18 bpm • According to the literature, most benign insulinoma cases activity, vomiting, urinary - Oxygen saturation: 99% on room air • EEG displayed no epileptiform discharges, consist of a solitary tumor located in the head of the • These pancreatic beta cell tumors are mostly benign and incontinence, and hypoglycemia electroencephalographic seizures, or lateralized pancreas with a median diameter less than 2 cm.2 occur sporadically. However, less than 10% of cases are • Oriented to person, place, and time. with a blood glucose level of 25 focal abnormalities. associated with Multiple Endocrine Neoplasia Type 1 Cooperative, behaving appropriately, mg/dl.