An Introduction to Understanding Elevation-Based Topography: How Elevation Data Are Displayed–Areview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Shaded Elevation Map of Ohio
STATE OF OHIO DEPARTMENT OF NATURAL RESOURCES DIVISION OF GEOLOGICAL SURVEY Ted Strickland, Governor Sean D. Logan, Director Lawrence H. Wickstrom, Chief SHADED ELEVATION MAP OF OHIO 0 10 20 30 40 miles 0 10 20 30 40 kilometers SCALE 1:2,000,000 427-500500-600600-700700-800800-900900-10001000-11001100-12001200-13001300-14001400-1500>1500 Land elevation in feet Lake Erie water depth in feet 0-6 7-12 13-18 19-24 25-30 31-36 37-42 43-48 49-54 55-60 61-66 67-84 SHADED ELEVATION MAP This map depicts the topographic relief of Ohio’s landscape using color lier impeded the southward-advancing glaciers, causing them to split into to represent elevation intervals. The colorized topography has been digi- two lobes, the Miami Lobe on the west and the Scioto Lobe on the east. tally shaded from the northwest slightly above the horizon to give the ap- Ridges of thick accumulations of glacial material, called moraines, drape pearance of a three-dimensional surface. The map is based on elevation around the outlier and are distinct features on the map. Some moraines in data from the U.S. Geological Survey’s National Elevation Dataset; the Ohio are more than 200 miles long. Two other glacial lobes, the Killbuck grid spacing for the data is 30 meters. Lake Erie water depths are derived and the Grand River Lobes, are present in the northern and northeastern from National Oceanic and Atmospheric Administration data. This digi- portions of the state. tally derived map shows details of Ohio’s topography unlike any map of 4 Eastern Continental Divide—A continental drainage divide extends the past. -

Meyers Height 1
University of Connecticut DigitalCommons@UConn Peer-reviewed Articles 12-1-2004 What Does Height Really Mean? Part I: Introduction Thomas H. Meyer University of Connecticut, [email protected] Daniel R. Roman National Geodetic Survey David B. Zilkoski National Geodetic Survey Follow this and additional works at: http://digitalcommons.uconn.edu/thmeyer_articles Recommended Citation Meyer, Thomas H.; Roman, Daniel R.; and Zilkoski, David B., "What Does Height Really Mean? Part I: Introduction" (2004). Peer- reviewed Articles. Paper 2. http://digitalcommons.uconn.edu/thmeyer_articles/2 This Article is brought to you for free and open access by DigitalCommons@UConn. It has been accepted for inclusion in Peer-reviewed Articles by an authorized administrator of DigitalCommons@UConn. For more information, please contact [email protected]. Land Information Science What does height really mean? Part I: Introduction Thomas H. Meyer, Daniel R. Roman, David B. Zilkoski ABSTRACT: This is the first paper in a four-part series considering the fundamental question, “what does the word height really mean?” National Geodetic Survey (NGS) is embarking on a height mod- ernization program in which, in the future, it will not be necessary for NGS to create new or maintain old orthometric height benchmarks. In their stead, NGS will publish measured ellipsoid heights and computed Helmert orthometric heights for survey markers. Consequently, practicing surveyors will soon be confronted with coping with these changes and the differences between these types of height. Indeed, although “height’” is a commonly used word, an exact definition of it can be difficult to find. These articles will explore the various meanings of height as used in surveying and geodesy and pres- ent a precise definition that is based on the physics of gravitational potential, along with current best practices for using survey-grade GPS equipment for height measurement. -

Geographical Influences on Climate Teacher Guide
Geographical Influences on Climate Teacher Guide Lesson Overview: Students will compare the climatograms for different locations around the United States to observe patterns in temperature and precipitation. They will describe geographical features near those locations, and compare graphs to find patterns in the effect of mountains, oceans, elevation, latitude, etc. on temperature and precipitation. Then, students will research temperature and precipitation patterns at various locations around the world using the MY NASA DATA Live Access Server and other sources, and use the information to create their own climatogram. Expected time to complete lesson: One 45 minute period to compare given climatograms, one to two 45 minute periods to research another location and create their own climatogram. To lessen the time needed, you can provide students data rather than having them find it themselves (to focus on graphing and analysis), or give them the template to create a climatogram (to focus on the analysis and description), or give them the assignment for homework. See GPM Geographical Influences on Climate – Climatogram Template and Data for these options. Learning Objectives: - Students will brainstorm geographic features, consider how they might affect temperature and precipitation, and discuss the difference between weather and climate. - Students will examine data about a location and calculate averages to compare with other locations to determine the effect of geographic features on temperature and precipitation. - Students will research the climate patterns of a location and create a climatogram and description of what factors affect the climate at that location. National Standards: ESS2.D: Weather and climate are influenced by interactions involving sunlight, the ocean, the atmosphere, ice, landforms, and living things. -
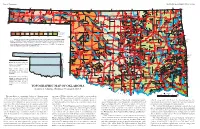
TOPOGRAPHIC MAP of OKLAHOMA Kenneth S
Page 2, Topographic EDUCATIONAL PUBLICATION 9: 2008 Contour lines (in feet) are generalized from U.S. Geological Survey topographic maps (scale, 1:250,000). Principal meridians and base lines (dotted black lines) are references for subdividing land into sections, townships, and ranges. Spot elevations ( feet) are given for select geographic features from detailed topographic maps (scale, 1:24,000). The geographic center of Oklahoma is just north of Oklahoma City. Dimensions of Oklahoma Distances: shown in miles (and kilometers), calculated by Myers and Vosburg (1964). Area: 69,919 square miles (181,090 square kilometers), or 44,748,000 acres (18,109,000 hectares). Geographic Center of Okla- homa: the point, just north of Oklahoma City, where you could “balance” the State, if it were completely flat (see topographic map). TOPOGRAPHIC MAP OF OKLAHOMA Kenneth S. Johnson, Oklahoma Geological Survey This map shows the topographic features of Oklahoma using tain ranges (Wichita, Arbuckle, and Ouachita) occur in southern contour lines, or lines of equal elevation above sea level. The high- Oklahoma, although mountainous and hilly areas exist in other parts est elevation (4,973 ft) in Oklahoma is on Black Mesa, in the north- of the State. The map on page 8 shows the geomorphic provinces The Ouachita (pronounced “Wa-she-tah”) Mountains in south- 2,568 ft, rising about 2,000 ft above the surrounding plains. The west corner of the Panhandle; the lowest elevation (287 ft) is where of Oklahoma and describes many of the geographic features men- eastern Oklahoma and western Arkansas is a curved belt of forested largest mountainous area in the region is the Sans Bois Mountains, Little River flows into Arkansas, near the southeast corner of the tioned below. -

Datums in Texas NGS: Welcome to Geodesy
Datums in Texas NGS: Welcome to Geodesy Geodesy is the science of measuring and monitoring the size and shape of the Earth and the location of points on its surface. NOAA's National Geodetic Survey (NGS) is responsible for the development and maintenance of a national geodetic data system that is used for navigation, communication systems, and mapping and charting. ln this subject, you will find three sections devoted to learning about geodesy: an online tutorial, an educational roadmap to resources, and formal lesson plans. The Geodesy Tutorial is an overview of the history, essential elements, and modern methods of geodesy. The tutorial is content rich and easy to understand. lt is made up of 10 chapters or pages (plus a reference page) that can be read in sequence by clicking on the arrows at the top or bottom of each chapter page. The tutorial includes many illustrations and interactive graphics to visually enhance the text. The Roadmap to Resources complements the information in the tutorial. The roadmap directs you to specific geodetic data offered by NOS and NOAA. The Lesson Plans integrate information presented in the tutorial with data offerings from the roadmap. These lesson plans have been developed for students in grades 9-12 and focus on the importance of geodesy and its practical application, including what a datum is, how a datum of reference points may be used to describe a location, and how geodesy is used to measure movement in the Earth's crust from seismic activity. Members of a 1922 geodetic suruey expedition. Until recent advances in satellite technology, namely the creation of the Global Positioning Sysfem (GPS), geodetic surveying was an arduous fask besf suited to individuals with strong constitutions, and a sense of adventure. -
LCD): Computerized Corneal Topography (L33810
Local Coverage Determination (LCD): Computerized Corneal Topography (L33810) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT NUMBER JURISDICTION STATE(S) First Coast Service Options, Inc. A and B MAC 09102 - MAC B J - N Florida First Coast Service Options, Inc. A and B MAC 09202 - MAC B J - N Puerto Rico First Coast Service Options, Inc. A and B MAC 09302 - MAC B J - N Virgin Islands LCD Information Document Information LCD ID Original Effective Date L33810 For services performed on or after 10/01/2015 LCD Title Revision Effective Date Computerized Corneal Topography For services performed on or after 01/08/2019 Proposed LCD in Comment Period Revision Ending Date N/A N/A Source Proposed LCD Retirement Date N/A N/A AMA CPT / ADA CDT / AHA NUBC Copyright Notice Period Start Date Statement N/A CPT codes, descriptions and other data only are copyright 2019 American Medical Association. All Rights Notice Period End Date Reserved. Applicable FARS/HHSARS apply. N/A Current Dental Terminology © 2019 American Dental Association. All rights reserved. Copyright © 2019, the American Hospital Association, Chicago, Illinois. Reproduced with permission. No portion of the AHA copyrighted materials contained within this publication may be copied without the express written consent of the AHA. AHA copyrighted materials including the UB-04 codes and descriptions may not be removed, copied, or utilized within any Created on 01/02/2020. Page 1 of 7 software, product, service, solution or derivative work without the written consent of the AHA. -

Division of Health Care Financing & Policy SB 278 Section 16
Division of Health Care Financing & Policy SB 278 Section 16 - Physician Rates Reporting Facility & Non-Facility Rate Comparison Nevada 2016 2016 Medicaid Medicaid Medicaid Medicare Medicare vs. vs. Procedure Code & Description Rates (1) Non-Facility Facility Medicare Medicare Rates for Rates for Non-Facility Facility 10021 Fna w/o image 70.92 128.90 72.80 (57.98) (1.88) 10022 Fna w/image 65.39 148.21 68.38 (82.82) (2.99) 10030 Guide cathet fluid drainage 154.73 827.01 176.71 (672.28) (21.98) 10035 Perq dev soft tiss 1st imag 86.35 568.38 90.92 (482.03) (4.57) 10036 Perq dev soft tiss add imag 43.52 495.42 45.82 (451.90) (2.30) 10040 Acne surgery 87.47 106.03 92.10 (18.56) (4.63) 10060 Drainage of skin abscess 95.60 122.68 101.60 (27.08) (6.00) 10061 Drainage of skin abscess 178.04 215.50 188.01 (37.46) (9.97) 10080 Drainage of pilonidal cyst 103.29 188.83 107.87 (85.54) (4.58) 10081 Drainage of pilonidal cyst 172.45 281.57 177.64 (109.12) (5.19) 10120 Remove foreign body 103.22 159.56 108.73 (56.34) (5.51) 10121 Remove foreign body 185.58 287.08 194.44 (101.50) (8.86) 10140 Drainage of hematoma/fluid 118.06 170.87 124.18 (52.81) (6.12) 10160 Puncture drainage of lesion 95.62 136.49 100.72 (40.87) (5.10) 10180 Complex drainage wound 178.97 258.94 188.14 (79.97) (9.17) 11000 Debride infected skin 28.42 56.88 29.76 (28.46) (1.34) 11001 Debride infected skin add-on 14.22 22.40 14.87 (8.18) (0.65) 11004 Debride genitalia & perineum 579.35 608.28 608.28 (28.93) (28.93) 11005 Debride abdom wall 781.65 822.97 822.97 (41.32) (41.32) 11006 Debride -

Current Developments in Corneal Topography and Tomography
diagnostics Review Current Developments in Corneal Topography and Tomography Piotr Kanclerz 1,2,* , Ramin Khoramnia 3 and Xiaogang Wang 4 1 Hygeia Clinic, Department of Ophthalmologyul, Ja´skowaDolina 57, 80-286 Gda´nsk,Poland 2 Helsinki Retina Research Group, University of Helsinki, 00100 Helsinki, Finland 3 The David J. Apple International Laboratory for Ocular Pathology, Department of Ophthalmology, University of Heidelberg, 69120 Heidelberg, Germany; [email protected] 4 Department of Cataract, Shanxi Eye Hospital, Taiyuan 030002, China; [email protected] * Correspondence: [email protected] Abstract: Introduction: Accurate assessment of the corneal shape is important in cataract and refractive surgery, both in screening of candidates as well as for analyzing postoperative outcomes. Although corneal topography and tomography are widely used, it is common that these technologies are confused. The aim of this study was to present the current developments of these technologies and particularly distinguish between corneal topography and tomography. Methods: The PubMed, Web of Science and Embase databases were the main resources used to investigate the medical literature. The following keywords were used in various combinations: cornea, corneal, topography, tomography, Scheimpflug, Pentacam, optical coherence tomography. Results: Topography is the study of the shape of the corneal surface, while tomography allows a three-dimensional section of the cornea to be presented. Corneal topographers can be divided into large- and small-cone Placido-based devices, as well as devices with color-LEDs. For corneal tomography, scanning slit or Scheimpflug imaging and optical coherence tomography may be employed. In several devices, corneal topography and tomography have been successfully combined with tear-film analysis, aberrometry, optical biometry and anterior/posterior segment optical coherence tomography. -

Safety and Effectiveness of the UV-X System for Corneal Collagen Cross
Evaluation of two Riboflavin Dosing Regimens for Corneal Collagen Cross-Linking in Eyes with Progressive Keratoconus or Ectasia Protocol 2010-0243, Version: 15 Protocol Date: September 16, 2016 PHYSICIAN SPONSOR: Francis W. Price, Jr. MD CONFIDENTIAL Background This clinical protocol is designed to evaluate two riboflavin-dosing regimens for treatment of patients with progressive keratoconus or corneal ectasia using investigational technology that increases the cross linking of the corneal stroma using the photochemical interaction of UVA light with the chromophore riboflavin. In this treatment, the corneal stroma is saturated with riboflavin by irrigating the surface after removal of the corneal epithelium. The riboflavin-saturated cornea is then exposed to a uniform field of UVA light with a narrow bandwidth centered at 365 nm. The light is generated by an IROC UV-X irradiation system that creates a uniform 11 mm circle of UVA light. The device has a timer that allows a precise 30-minute exposure of the corneal tissues. The irradiation field of the UVX system produces UVA light with a uniform irradiance of 3 mj/cm2 at the corneal surface. The FDA has classified this technology as a combination product with two components. First is the UV-X light source, which has an LED source and is calibrated and rendered uniform by the use of an optical homogenizer. The second component is a riboflavin ophthalmic solution. This solution is used to saturate the corneal stroma prior to its photochemical activation. This combination product has been studied in a FDA-approved, randomized, placebo- controlled, multi-center trial that has enrolled patients. -

Using a Surveyor's Level to Generate a Topographical
Using a Surveyor’s Level to Generate a Topographical Map This application note describes the process of using a surveyor's level for generating a topography (topo) map. The site survey described below uses San Francisco's Yerba Buena Gardens as a site for recording relative elevations over a specific area. With these relative elevations organized into a grid, a topographical map can be created. Equipment: (most available from Tool Lending Library): Surveyor's Level Level Tripod Leveling Rod Compass 100' Tape Measure Notebook and Pencil Procedure: Step 1: Find a Reference Point (Benchmark Elevation) Step 2: Set up the Surveyor's Level Step 3: Reading the Leveling Rod Step 4: Taking Readings Step 5: Make a Grid Over the Chosen Plot Step 6: Making Sense of the Collected Data Step 7: Drawing Topography Lines Figure 1: Surveyor’s level Step 1: Find a Reference Point (Benchmark Elevation) 1. Establish a reference point, also known as the benchmark elevation. A list of official benchmark elevations in San Francisco is available from the Bureau of Street Use and Mapping. (located at 875 Stevenson Street, Room 460 /// San Francisco, CA. 94103 /// 415.554.5810). The nearest benchmark to the plot is the intersection of 4th and Mission Street. (Figure 2). Using a Surveyor’s Level to Generate a Topography Map Page 1 of 8 Copyright© Pacific Gas and Electric Company, all rights reserved www.pge.com/pec Figure 2: Benchmark descriptions as printed by the SF Bureau of Street Use and Mapping. The benchmark on the list in Figure 2 is a fire hydrant with the word "OPEN" on top. -

Refractive Surgery
I explore and get information from inside the eye, that´s my job. You can then go deeper into the diagnosis. You decide, I explore! FOR ACCURACY IN REFRACTIVE SURGERY ACE® is a technology that utilizes the power of high-resolution swept-source OCT imaging to provide the key corneal measurements. Optimizing the quality of the preoperative data provides more information to help you to improve the safety of your refractive surgery procedures.1 ACE® and the TECHNOLAS® TeneoTM 317 Model 2 offer solutions that will refine your results. Transform your daily surgical routine into an exciting day with a platform that brings together corneal topography and tomography and allowing data transfer between both devices. All corneal measurements are based on high-resolution swept-source OCT images KEY FUNCTIONS Corneal topography Corneal wavefront analysis Corneal tomography Differential maps Pachymetry Progression analysis Total corneal power Data transfer with TECHNOLAS® TENEOTM 317 Model 2 * All corneal measurements based on high- resolution swept-source OCT images 1. Muriël Doors et al. Value of optical coherence tomography for anterior segment surgery. J Cataract Refract Surg 2010; 36:1213–1229 Q 2010 ADVANCED CORNEAL EXPLORER HIGHLY CUSTOMIZABLE MAP LAYOUT Display up to 6 maps simultaneously, compare OD and OS, or perform an analysis over time. 12 different map types: Assess each patient’s corneal topography and Anterior and posterior axial or Pachymetry tomography, including tangential curvature Total corneal power curvature and elevation Anterior and posterior elevation maps of the anterior and Anterior and total corneal wavefront (best fit sphere and best fit torus) posterior surfaces. -

Code Procedure Cpt Price University Physicians Group
UNIVERSITY PHYSICIANS GROUP (UPG) PRICES OF PROVIDER SERVICES CODE PROCEDURE MOD CPT PRICE 0001A IMM ADMN SARSCOV2 30MCG/0.3ML DIL RECON 1ST DOSE 0001A $40.00 0002A IMM ADMN SARSCOV2 30MCG/0.3ML DIL RECON 2ND DOSE 0002A $40.00 0011A IMM ADMN SARSCOV2 100 MCG/0.5 ML 1ST DOSE 0011A $40.00 0012A IMM ADMN SARSCOV2 100 MCG/0.5 ML 2ND DOSE 0012A $40.00 0021A IMM ADMN SARSCOV2 5X1010 VP/0.5 ML 1ST DOSE 0021A $40.00 0022A IMM ADMN SARSCOV2 5X1010 VP/0.5 ML 2ND DOSE 0022A $40.00 0031A IMM ADMN SARSCOV2 AD26 5X10^10 VP/0.5 ML 1 DOSE 0031A $40.00 0042T CEREBRAL PERFUS ANALYSIS, CT W/CONTRAST 0042T $954.00 0054T BONE SURGERY USING COMPUTER ASSIST, FLURO GUIDED 0054T $640.00 0055T BONE SURGERY USING COMPUTER ASSIST, CT/ MRI GUIDED 0055T $1,188.00 0071T U/S LEIOMYOMATA ABLATE <200 CC 0071T $2,500.00 0075T 0075T PR TCAT PLMT XTRC VRT CRTD STENT RS&I PRQ 1ST VSL 26 26 $2,208.00 0126T CAROTID INT-MEDIA THICKNESS EVAL FOR ATHERSCLER 0126T $55.00 0159T 0159T COMPUTER AIDED BREAST MRI 26 26 $314.00 PR RECTAL TUMOR EXCISION, TRANSANAL ENDOSCOPIC 0184T MICROSURGICAL, FULL THICK 0184T $2,315.00 0191T PR ANT SEGMENT INSERTION DRAINAGE W/O RESERVOIR INT 0191T $2,396.00 01967 ANESTH, NEURAXIAL LABOR, PLAN VAG DEL 01967 $2,500.00 01996 PR DAILY MGMT,EPIDUR/SUBARACH CONT DRUG ADM 01996 $285.00 PR PERQ SAC AGMNTJ UNI W/WO BALO/MCHNL DEV 1/> 0200T NDL 0200T $5,106.00 PR PERQ SAC AGMNTJ BI W/WO BALO/MCHNL DEV 2/> 0201T NDLS 0201T $9,446.00 PR INJECT PLATELET RICH PLASMA W/IMG 0232T HARVEST/PREPARATOIN 0232T $1,509.00 0234T PR TRANSLUMINAL PERIPHERAL ATHERECTOMY, RENAL