Acute Otitis Externa (Swimmer's Ear)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Temporo-Mandibular Joint (Tmj) Dysfunction
Office: (310) 423-1220 BeverlyHillsENT.com Fax: (310) 423-1230 TEMPORO-MANDIBULAR JOINT (TMJ) DYSFUNCTION You may not have heard of it, but you use it hundreds of times every day. It is the Temporo- Mandibular Joint (TMJ), the joint where the mandible (the lower jaw) joins the temporal bone of the skull, immediately in front of the ear on each side of your head. You move the joint every time you chew or swallow. You can locate this joint by putting your finger on the triangular structure in front of your ear. Then move your finger just slightly forward and press firmly while you open your jaw all the way and shut it. The motion you feel is the TMJ. You can also feel the joint motion in your ear canal. These maneuvers can cause considerable discomfort to a patient who is having TMJ trouble, and physicians use these maneuvers with patients for diagnosis. TMJ Dysfunction can cause the following symptoms: Ear pain Sore jaw muscles Temple/cheek pain Jaw popping/clicking Locking of the jaw Difficulty in opening the mouth fully Frequent head/neck aches The pain may be sharp and searing, occurring each time you swallow, yawn, talk, or chew, or it may be dull and constant. It hurts over the joint, immediately in front of the ear, but pain can also radiate elsewhere. It often causes spasms in the adjacent muscles that are attached to the bones of the skull, face, and jaws. Then, pain can be felt at the side of the head (the temple), the cheek, the lower jaw, and the teeth. -

UPDATE VOLUME 20 • ISSUE 3 the Newsletter of the Council for Accreditation in Occupational Hearing Conservation
Fall 2008 UPDATE VOLUME 20 • ISSUE 3 The Newsletter of the Council for Accreditation in Occupational Hearing Conservation Hearing noise-induced hearing loss and further degradation of communication. If too much hearing protection is provided, Conservation the combined effects of the hearing loss and the attenuation provided by the hearing protector may result in critical sounds for the Hearing- and communication signals becoming inaudible. I’m often asked what type of hearing protector is best for Impaired Worker workers with hearing impairment. Considering that there is no ‘best’ HPD for all workers in any hearing category, it Introduction by Ted Madison should come as no surprise that no single type of device will The prevalence of hearing loss among persons enrolled meet the needs of all those with hearing loss. What seems in occupational hearing conservation programs (HCPs) is to be consistent, however, is that each case is unique, and difficult to determine. Recently, Tak and Calvert (2008) that extra time and effort is required to help these workers estimated that 11.4% of the overall US workforce reports find the right combination of protection, having hearing difficulty of varying communication and auditory awareness. degrees and that approximately ¼ of Consultation with an audiologist or other the hearing difficulty reported can hearing health care professional is also be attributed to employment. These an important step in most cases. estimates are based on analysis of data One valuable resource is the OSHA from the US National Health Interview Safety & Health Information Bulletin Survey (NHIS) that were collected (SHIB) titled “Hearing Conservation from 1997 to 2003. -
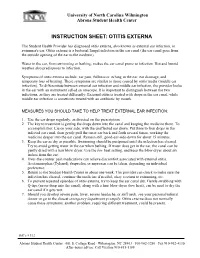
Instruction Sheet: Otitis Externa
University of North Carolina Wilmington Abrons Student Health Center INSTRUCTION SHEET: OTITIS EXTERNA The Student Health Provider has diagnosed otitis externa, also known as external ear infection, or swimmer's ear. Otitis externa is a bacterial/fungal infection in the ear canal (the ear canal goes from the outside opening of the ear to the eardrum). Water in the ear, from swimming or bathing, makes the ear canal prone to infection. Hot and humid weather also predisposes to infection. Symptoms of otitis externa include: ear pain, fullness or itching in the ear, ear drainage, and temporary loss of hearing. These symptoms are similar to those caused by otitis media (middle ear infection). To differentiate between external ear infection and middle ear infection, the provider looks in the ear with an instrument called an otoscope. It is important to distinguish between the two infections, as they are treated differently: External otitis is treated with drops in the ear canal, while middle ear infection is sometimes treated with an antibiotic by mouth. MEASURES YOU SHOULD TAKE TO HELP TREAT EXTERNAL EAR INFECTION: 1. Use the ear drops regularly, as directed on the prescription. 2. The key to treatment is getting the drops down into the canal and keeping the medicine there. To accomplish this: Lie on your side, with the unaffected ear down. Put three to four drops in the infected ear canal, then gently pull the outer ear back and forth several times, working the medicine deeper into the ear canal. Remain still, good-ear-side-down for about 15 minutes. -

The Ear, Nose, and Throat Exam Jeffrey Texiera, MD and Joshua Jabaut, MD CPT, MC, USA LT, MC, USN
The Ear, Nose, and Throat Exam Jeffrey Texiera, MD and Joshua Jabaut, MD CPT, MC, USA LT, MC, USN Midatlantic Regional Occupational and Environmental Medicine Conference Sept. 23, 2017 Disclosures ●We have no funding or financial interest in any product featured in this presentation. The items included are for demonstration purposes only. ●We have no conflicts of interest to disclose. Overview ● Overview of clinically oriented anatomy - presented in the format of the exam ● The approach ● The examination ● Variants of normal anatomy ● ENT emergencies ● Summary/highlights ● Questions Anatomy ● The head and neck exam consists of some of the most comprehensive and complicated anatomy in the human body. ● The ear, nose, and throat comprise a portion of that exam and a focused clinical encounter for an acute ENT complaint may require only this portion of the exam. Ears www.Medscape.com www.taqplayer.info Ear – Vestibular organ www.humanantomylibrary.com Nose/Sinus Anatomy Inferior Middle Turbinate Turbinate Septum Dorsum Sidewalls Ala Floor Tip www.ENT4Students.blogspot.com Columella Vestibule www.beautyepic.com Oral cavity and oropharynx (throat) www.apsubiology.org Neck www.rdhmag.com The Ear, Nose, and Throat exam Perform in a standardized systematic way that works for you Do it the same way every time, this mitigates risk of missing a portion of the exam Practice the exam to increase comfort with performance and familiarize self with variants of normal Describe what you are doing to the patient, describe what you see in your documentation Use your PPE as appropriate A question to keep in mind… ●T/F: The otoscope is the optimal tool for examining the tympanic membrane. -

Investigation of the Incidence of Eustachian Tube Dysfunction in Patients with Sinonasal Disease*
ORIGINAL CONTRIBUTION Investigation of the incidence of Eustachian tube dysfunction in patients with sinonasal disease* 1 2 1 1 C.E. Rennie , M. Gutierrez , Y. Darby , V.J. Lund Rhinology Online, Vol 1: 85 - 89, 2018 http://doi.org/10.4193/RHINOL/18.050 1 Royal National Throat Nose and Ear Hospital, ENT, London, United Kingdom 2 University of North Carolina, Medical student, North Carolina, USA *Received for publication: August 12, 2018 Accepted: August 14, 2018 Abstract Background: Rhinosinusitis is characterised by inflammation affecting the respiratory mucosa of the nose and sinuses. Since the Eustachian tube and the middle ear cavity are also lined by the same mucosa, it is likely that the pathophysiological processes that give rise to rhinosinusitis will also affect these areas. Eustachian tube dysfunction (ETD) is a common condition, but it is often dismissed as a "minor" symptom in rhinology patients. Objective: The aim of this study was to determine the frequency of otologic symptoms in patients attending the rhinology clinic. The seven-item Eustachian Tube Dysfunction Questionnaire (ETDQ-7), a validated disease-specific instrument was used to assess symptoms with respect to ETD7. Study design: 119 patients attending the rhinology outpatient clinic completed ETDQ-7, a SNOT 22 and had their PNIF measured. Results: The results showed a significantly higher rate of ETD (p<0.01 paired t-test) in the rhinology patients (mean score 3.1, SD 1.64) as compared to a control population (mean 1.3, SD 0.3). Conclusion: Eustachian tube dysfunction is more common in rhinology patients then the general population, and within the rhinology population. -

Assessment of Antimicrobial Activity of Cerumen (Earwax) and Antibiotics
Microbiology Research 2020; volume 11:8565 Assessment of antimicrobial nation of fatty acid). Another gland i.e. apoc- activity of cerumen (earwax) rine sweat glands release secretion that com- Correspondence: Iffat Naz, Department of bines with the sebum to form cerumen. It Biology, Scientific Unit, Deanship of and antibiotics against picks up discarded cells, ear follicles and Educational Services, Qassim University, pathogenic bacteria isolated may contain dust or other debris, but the Buraidah, 51452, Qassim, Kingdom of Saudi from ear pus samples resulting compound forms earwax or ceru- Arabia (KSA). men.6 Tel.: +966 533897891 E-mail: [email protected] ; There are two different types of geneti- [email protected] Iffat Naz cally determined earwax such as wet type Department of Biology, Scientific Unit, and dry type. The dry type is most common Key words: Ear pus samples; Pathogenic bac- Deanship of Educational Services, in Asians and Native Americans and has a teria; Antibiotics; Cerumen; Antibacterial Qassim University, Buraidah, Qassim, grey brownish colour while the wet type can potency. Kingdom of Saudi Arabia be found in Caucasians and Africians and has a brown or dark colour.7 About 30-50% of Acknowledgements: The author would like to South Asians, Central Asians and Pacific thanks Mr. Jamil & Miss. Javeria (M. Phil islanders have the dry type of cerumen. Scholars), for assisting in collection of ear pus Abstract Cerumen type has been used by anthropolo- samples from different hospitals of Peshawar, gist to track human migratory patterns, such KP, Pakistan. She is also grateful to Dr. Abdul The present study is focused on the Rehman for providing laboratory facilities, at as those of Eskimas.8 Further, the study of assessment of the antimicrobial activity of Department of Microbiology, Abasyn cerumen and antibiotics against bacteria earwax has shown controversy, as some University Peshawar, KP, Pakistan. -

Acoustic Trauma and Hyperbaric Oxygen Treatment
Acoustic Trauma and Hyperbaric Oxygen Treatment Mesut MUTLUOGLU Department of Underwater and Hyperbaric Medicine Gulhane Military Medical Academy Haydarpasa Teaching Hospital 34668, Uskudar, Istanbul TURKEY [email protected] ABSTRACT As stated in the conclusions of the HFM-192 report on hyperbaric oxygen therapy (HBOT) in military medical setting, acoustic trauma is a frequent consequence of military activity in operation. Acoustic trauma refers to an acute hearing loss following a single sudden and very intense noise exposure. It differs from chronic noise induced hearing (NIHL) loss in that it is usually unilateral and causes sudden profound hearing loss. Acoustic trauma is a type of sensorineural hearing loss affecting inner ear structures; particularly the inner and outer hair cells of the organ of Corti within the cochlea. Exposure to noise levels above 85 decibel (dB) may cause hearing loss. While long-term exposure to repetitive or continuous noise above 85 dB may cause chronic NIHL, a single exposure above 130-140 dB, as observed in acoustic trauma, may cause acute NIHL. The loudest sound a human ear may tolerate without pain varies individually, but is usually around 120dB. Military personnel are especially at increased risk for acoustic trauma due to fire arm use in the battle zone. While a machine gun generates around 145dB sound, a rifle generates 157- 163dB, a 105 mm towed howitzer 183dB and an improvised explosive device around 180dB sound. Acoustic trauma displays a gradually down-slopping pattern in the audiogram, particularly after 3000Hz and is therefore described as high-frequency hearing loss. Tinnitus is almost always associated with acoustic trauma. -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired -

Older Adult Hearing Loss and Screening Key Points • Eighty Percent of Older American Adults Have Untreated Hearing Loss. •
Older Adult Hearing Loss and Screening Key Points Eighty percent of older American adults have untreated hearing loss. Hearing loss is associated with decreased quality of life, depression, communication disorders, social withdrawal and cognitive impairment. Overview Definition Presbycusis is another term for age-related sensorineural hearing loss (ARHL). o Damage to the cochlea, Cranial Nerve VIII, or Internal Auditory canal o Bilateral, symmetric, high-frequency sensorineural hearing loss Noise-induced hearing loss (NIHL) o Direct mechanical injury to sensory hair cells in the cochlea o Continuous noise exposure Aging and hearing loss Cell reduction in auditory cortex Acoustic nerve (CN VIII) fiber degeneration Inner ear sensory cell loss and membrane calcification Risk Factors Advancing Age (ARHI) Exposure to loud noises or ototoxic agents (i.e. loud machinery) (NIHL) Other External ear or middle ear conductive hearing loss risk factors include: o Cerumen impaction o Middle ear fluid o Perforated tympanic membrane Assessment Recommendations for hearing assessments: Screening all older adults over the age of 65 years. Screening should be conducted in a primary care setting. Obtain history of chronic medical conditions (diabetes mellitus, CAD), ear infections, ear trauma, occupation Medication review assessing for use of diuretics (loop), aspirin, antineoplastic (cisplatin, 5- fluorouracil), antimalarial (chloroquine, quinine), and antibiotic (aminoglycosides, erythromycin, tetracycline, vancomycin) Assessment Instruments available include: o Hearing Handicap Inventory for the Elderly Screening (HHIE-S) https://www.audiology.org/sites/default/files/PracticeManagement/Medicare_HHI.pdf . 10 question questionnaire . Score greater than 10 points should be referred to an audiologist o Audio Scope (Welch Allyn, Inc.) . Otoscope examination . Test hearing o Whispered Voice Test, finger rub or a watch tick test o Ask the question - “Do you have a hearing problem now?” If any of the above four are positive – referral to an Audiologist is indicated. -

MASTOIDECTOMY (With Or Without Tympanoplasty)
MASTOIDECTOMY (with or without tympanoplasty) Informed Surgical Consent A mastoidectomy is a surgical procedure that removes diseased mastoid air cells. These cells sit behind your ear in a hollow space in your skull. Typically, a mastoidectomy (with or without tympanoplasty) is recommended for patients that have a cholesteatoma and/or a chronically infected ear that has failed medical management (chronic otitis media). Your doctor at Suburban Ear, Nose, and Throat is uniquely trained to perform mastoidectomy surgery. A cholesteatoma is a benign skin cyst that grows inside the ear. Most cholesteatomas occupy the middle ear space behind the tympanic membrane (eardrum). Occasionally, cholesteatomas arise from the external ear canal, and then are referred to as canal cholesteatomas. Canal cholesteatomas can usually be managed conservatively with routine ear cleaning in the office, but rarely they will require surgical intervention. Middle ear cholesteatomas, on the other hand, almost always require surgery. They typically occur in children and adults who have chronic eustachian tube dysfunction (ETD), a problem with ventilation or "popping" the ears. When ETD is present for many years, it can lead to development of a cholesteatoma. Although most cholesteatomas are acquired, some patients are actually born with the cholesteatoma; this is called a congenital cholesteatoma. Cholesteatomas grow very slowly, but they can cause significant damage to any structure in the ear that they come in contact with. Commonly, the cholesteatoma erodes into the tiny bones (ossicles) in the middle ear that allow for hearing. Untreated, cholesteatomas can lead to hearing loss, infection, chronic ear discharge, ear pain, dizziness, facial paralysis, or in rare cases, infection that spreads to the brain. -

What Causes Swimmer's Ear?
Swimmer’s Ear Affecting the outer ear, swimmer’s ear is a painful condition resulting from inflammation, irritation, or infection. These symptoms often occur after water gets trapped in your ear, with subsequent spread of bacteria or fungal organisms. Because this condition commonly affects swimmers, it is known as swimmer’s ear. Swimmer’s ear (also called acute otitis externa) often affects children and teenagers, but can also affect those with eczema (a condition that causes the skin to itch), or excess earwax. Your doctor will prescribe treatment to reduce your pain and to treat the infection. What causes swimmer’s ear? A common source of the infection is increased moisture trapped in the ear canal, from baths, showers, swimming, or moist environments. When water is trapped in the ear canal, bacteria that normally inhabit the skin and ear canal multiply, causing infection of the ear canal. Swimmer’s ear needs to be treated to reduce pain and eliminate any effect it may have on your hearing, as well as to prevent the spread of infection. Other factors that may contribute to swimmer’s ear include: ● Contact with excessive bacteria that may be present in hot tubs or polluted water ● Excessive cleaning of the ear canal with cotton swabs ● Contact with certain chemicals such as hair spray or hair dye (Avoid this by placing cotton balls in your ears when using these products.) ● Damage to the skin of the ear canal following water irrigation to remove wax ● A cut in the skin of the ear canal ● Other skin conditions affecting the ear canal, such as eczema or seborrhea What are the signs and symptoms? The most common symptoms of swimmer’s ear are itching inside the ear and pain that gets worse when you tug on the auricle (outer ear). -

Supplementary Methods Earwax Sample Extraction a Clinical Research Assistant Was Specifically Trained in the Use of the Reiner-A
Supplementary Methods Earwax Sample Extraction A clinical research assistant was specifically trained in the use of the Reiner-Alexander syringe by one ear-nose-throat specialist doctor. Before cleaning both ears, the external auditory canal was examined using an otoscope to rule out the presence of any external ear pathology, such as impacted earwax or perforated eardrum. Briefly, the Reiner-Alexander syringe slowly injects water at 37°C inside the external ear canal. The process of syringing creates a sensation of mild pressure in the ear as the warm water from the syringe flushes the wax out. The expelled water and the extracted earwax secretion were collected in a kidney basin. During the follow-up visit, participants self-clean their right ears using the earwax self-sampling device, according to the manufacturer instructions (www.trears.com). The four labelled earwax samples were stored at 4 °C until they were analysed. Earwax Analysis using the Reiner-Alexander Syringe The extracted solution of water plus earwax secretion was stored in a 50 ml cryovial. Earwax samples were then resuspended with 500 µl Phosphate-Buffered Saline (PBS) to homogenise the sample. Then, 500 µl of diethyl ether was added to each sample and wobbled for one minute using a vortex. The resulting solution was stored at -20°C for 2 hours. Glucose levels were then analysed from the hydrophilic fraction. The earwax solution was dried using the displacement method of N2 at 25 degree Celsius. Following this, 125 µl of PPBS was added to resuspend each solution. The resulting solution containing earwax samples was stored at 4 degrees Celsius until analysed.