Drug Product: Ketoconazole Shampoo, 2%
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Therapeutic Class Overview Antifungals, Topical
Therapeutic Class Overview Antifungals, Topical INTRODUCTION The topical antifungals are available in multiple dosage forms and are indicated for a number of fungal infections and related conditions. In general, these agents are Food and Drug Administration (FDA)-approved for the treatment of cutaneous candidiasis, onychomycosis, seborrheic dermatitis, tinea corporis, tinea cruris, tinea pedis, and tinea versicolor (Clinical Pharmacology 2018). The antifungals may be further classified into the following categories based upon their chemical structures: allylamines (naftifine, terbinafine [only available over the counter (OTC)]), azoles (clotrimazole, econazole, efinaconazole, ketoconazole, luliconazole, miconazole, oxiconazole, sertaconazole, sulconazole), benzylamines (butenafine), hydroxypyridones (ciclopirox), oxaborole (tavaborole), polyenes (nystatin), thiocarbamates (tolnaftate [no FDA-approved formulations]), and miscellaneous (undecylenic acid [no FDA-approved formulations]) (Micromedex 2018). The topical antifungals are available as single entity and/or combination products. Two combination products, nystatin/triamcinolone and Lotrisone (clotrimazole/betamethasone), contain an antifungal and a corticosteroid preparation. The corticosteroid helps to decrease inflammation and indirectly hasten healing time. The other combination product, Vusion (miconazole/zinc oxide/white petrolatum), contains an antifungal and zinc oxide. Zinc oxide acts as a skin protectant and mild astringent with weak antiseptic properties and helps to -

Assessment Report on Melaleuca Alternifolia (Maiden and Betch) Cheel, M
24 November 2014 EMA/HMPC/320932/2012 Committee on Herbal Medicinal Products (HMPC) Assessment report on Melaleuca alternifolia (Maiden and Betch) Cheel, M. linariifolia Smith, M. dissitiflora F. Mueller and/or other species of Melaleuca, aetheroleum Based on Article 16d(1), Article 16f and Article 16h of Directive 2001/83/EC as amended (traditional use) Final Herbal substance(s) (binomial scientific name of Melaleuca alternifolia (Maiden and Betch) Cheel, the plant, including plant part) M. linariifolia Smith, M. dissitiflora F. Mueller and/or other species of Melaleuca, leaf and terminal branchlets Herbal preparation(s) Melaleuca alternifolia, aetheroleum Pharmaceutical forms Herbal preparation in liquid and semi-solid dosage forms for cutaneous use or in liquid dosage form for oromucosal use. Rapporteur Marisa Delbò Assessor(s) Marisa Delbò Gioacchino Calapai Peer-reviewer Jacqueline Viguet Poupelloz 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2015. Reproduction is authorised provided the source is acknowledged. Table of contents Table of contents ................................................................................................................... 2 1. Introduction ....................................................................................................................... 5 1.1. Description of the herbal substance(s), -
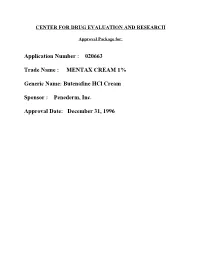
MENTAX CREAM 1% Generic Name: Butenafine Hcl Cream Sponsor : Penederm
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: Application Number : 020663 Trade Name : MENTAX CREAM 1% Generic Name: Butenafine HCl Cream Sponsor : Penederm, Inc. Approval Date: December 31, 1996 CENTER FOR DRUG EVALUATION AND RESEARCH Application Number 020663 APPROVAL LETTER DEC 3 I IW NDA 20-663 Penederm Incolpxated Attentiom John Quigley, Ph.D. Senior Vice President, Research and Development 320 Lakeside Drive, Suite A Foster City, CA W Dear Dr. QuigIey: Please refer to your December 22, 1995, new drug application submitted under section 505(b) of the Federal F@ Drug, and Cosmetic Act for Mentax (butenafine hydrochloride cream) cream, 1%. ● We acknowledge receipt of your amendments and correspondence dated December 27, 1995fi~ January 8 and 19, March 1 (two), 27 and 28, October 23,24 and 25, November 5 and 15, and December 12 and 31,1996. This new drug application provides for the treatment of tines corporis and tines cruris. We have completed the review of this application and have concluded that ;dequate information has been presented to demonstrate that the drug product is safe and effective for use as recommended in the enclosed revised draft labeling.- Accordingly, the application is approved effective on the date of this letter. The final printed labeling (FPL) must be identical to the enclosed revised drall labeling. The enclosed revised draft labeling was stated to be acceptable to you in the facsimile of your letter dated December 31,1996. Marketing the product with FPL that is not identical to the enclosed revised drafl labeling may render the product misbranded and an unapproved new drug. -

Jp Xvii the Japanese Pharmacopoeia
JP XVII THE JAPANESE PHARMACOPOEIA SEVENTEENTH EDITION Official from April 1, 2016 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the convenience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 64 Pursuant to Paragraph 1, Article 41 of the Law on Securing Quality, Efficacy and Safety of Products including Pharmaceuticals and Medical Devices (Law No. 145, 1960), the Japanese Pharmacopoeia (Ministerial Notification No. 65, 2011), which has been established as follows*, shall be applied on April 1, 2016. However, in the case of drugs which are listed in the Pharmacopoeia (hereinafter referred to as ``previ- ous Pharmacopoeia'') [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as ``new Pharmacopoeia'')] and have been approved as of April 1, 2016 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as of March 31, 2016 as those exempted from marketing approval pursuant to Paragraph 1, Article 14 of the Same Law (hereinafter referred to as ``drugs exempted from approval'')], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on September 30, 2017. -

Comparison of Efficacy and Safety of Topical 1% Butenafine and Topical 1% Ciclopirox Olamine in the Treatment of Tinea Pedis An
174 Turk J Dermatol 2017;11:174-8 • DOI: 10.4274/tdd.3324 Original Investigation / Özgün Araştırma Asude Kara Polat, Comparison of Efficacy and Safety of Topical 1% Aslı Akın Belli*, Emine Tuğba Butenafine and Topical 1% Ciclopirox Olamine Alataş**, in the Treatment of Tinea Pedis and Evaluation Gürsoy Doğan** of the Effects on the Quality of Life of These Treatmens: A Randomized Single-Blind Trial Tinea Pedis Tedavisinde Topikal %1 Butenafin ve Topikal %1 Siklopiroks Olaminin Etkinlik, Güvenilirliğinin Karşılaştırılması ve Bu Tedavilerin Yaşam Kalitesi Üzerine Etkilerinin Değerlendirilmesi: Randomize Tek Kör Bir Çalışma Abstract Objective: The aim of the study is to compare efficacy and safety of topical 1% butenafine and topical 1% ciclopirox olamine in tinea pedis and to evaluate effects of these treatments on quality of life. Methods: We conducted a randomized controlled trial on 80 patients with tinea pedis between May 2014 and May 2015. Of 80 patients, 40 were treated with 1% butenafine cream and 40 were treated with 1% ciclopirox olamine cream for one month. Clinical characteristics, Dermatology Life Quality Index (DLQI) scores, Physician’s Global Assessment (PhGA), and Patient’s Global Assessment were recorded. İstanbul Training and Results: Forty patients (21 male, 19 female) on butenafine therapy and 40 patients Research Hospital, Clinic of (15 male, 25 female) on ciclopirox olamine therapy were enrolled in the study. Both Dermatology, İstanbul, Turkey treatments significantly improved the clinical signs and symptoms, but no significant difference was found between the groups (p>0.05). The DLQI scores decreased *Muğla Sıtkı Koçman significantly after the treatments in both groups. -

Compounding for Scalp Disorders and Conditions
COMPOUNDING FOR SCALP DISORDERS AND CONDITIONS ACPE UAN#: 0145-9999-12-007-H04-P, 0145-9999-12-007-H04-T 1.0 Contact Hours (0.1 CEU), Expires 03/19/2015 Activity Type: Knowledge Y. Pramar, Ph.D., Professor of Pharmaceutics Xavier University of Louisiana, College of Pharmacy, New Orleans, Louisiana. Reprinted with permission of the author and the Louisiana Pharmacists Association where this article originally appeared. This activity may appear in other state pharmacy association journals. Participants should not seek credit for duplicate content. Goals: The goals of this article are to provide information on the physiology and disorders of the scalp, and typical drug therapy used to treat these disorders. Objectives Pharmacists & Technicians: At the conclusion of this lesson, the reader should be able to: 1. Discuss the physiology of the scalp and the function of the sebum, sweat glands and pores. 2. List at least five disorders/conditions of the scalp. 3. Describe different treatment approaches used in scalp disorders. 4. Recognize various formulations used in the treatment of seborrheic dermatitis, dandruff, psoriasis, hair loss, lice and ringworm. Introduction the hair follicle. Sebum consists of fatty acids and other Scalp disorders may be painful, annoying, unsightly and substances and protects the skin by reducing the embarrassing. Scalp problems may require short-term evaporation of water from the skin and blocks the treatment, but many of them need long-term therapy penetration of excess water into the skin. This sebum is over months, and sometimes years. Compounding one of two constituents making up the lipid film present pharmacists have a significant role in achieving on the skin surface, the other being the lipids of the successful therapeutic outcomes in this emerging field. -

What Published Literature Tells Us About Nanosilver
What Published Studies Tell Us Regarding Nanoparticles, N-acetyl-l-cysteine, Urea and Tea Tree Oil Chem Pharm Bull (Tokyo). 1998 Nov;46(11):1797-802. Enhancing effect of N-acetyl-l-cysteine or 2-mercaptoethanol on the in vitro permeation of 5-fluorouracil or tolnaftate through the human nail plate. Kobayashi Y1, Miyamoto M, Sugibayashi K, Morimoto Y. 1Faculty of Pharmaceutical Sciences, Josai University, Saitama, Japan. Abstract The enhancing effects of various vehicles on the in vitro permeation of a hydrophilic model drug, 5- fluorouracil (5-FU), or a lipophilic model drug, tolnaftate (TN), through human nail plates were investigated using a modified side-by-side diffusion cell. Tip pieces from the 5th finger-nail, clipped from healthy volunteers, were used in this permeation study. The swelling and softening properties of the nail pieces were also measured in each vehicle. The weights and stresses of the nail pieces were dramatically changed after immersion in aqueous solvents containing N-acetyl-L-cysteine (AC) or 2-mercaptoethanol (ME). However, no significant change in the physicochemical properties of the nail pieces was found in the lipophilic vehicles. Thus, the water content in the nail plates absorbed from vehicles may relate to their physicochemical properties. Although keratin-softening agents and new skin permeation enhancers did not significantly promote 5-FU permeation compared with water alone, the flux from solvent systems containing AC or ME was substantially higher. In addition, TN permeation from solvents containing AC or ME could be measured, whereas that from other solvents was undetectable. When the AC concentration was increased, the 5- FU permeation and the nail weight increased, and the stress of each nail piece decreased. -

Novel Small Molecule Antifungals for Invasive Fungal Infections
University of Kentucky UKnowledge Theses and Dissertations--Pharmacy College of Pharmacy 2020 NOVEL SMALL MOLECULE ANTIFUNGALS FOR INVASIVE FUNGAL INFECTIONS Emily Dennis University of Kentucky, [email protected] Author ORCID Identifier: https://orcid.org/0000-0001-7928-9705 Digital Object Identifier: https://doi.org/10.13023/etd.2020.506 Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation Dennis, Emily, "NOVEL SMALL MOLECULE ANTIFUNGALS FOR INVASIVE FUNGAL INFECTIONS" (2020). Theses and Dissertations--Pharmacy. 121. https://uknowledge.uky.edu/pharmacy_etds/121 This Doctoral Dissertation is brought to you for free and open access by the College of Pharmacy at UKnowledge. It has been accepted for inclusion in Theses and Dissertations--Pharmacy by an authorized administrator of UKnowledge. For more information, please contact [email protected]. STUDENT AGREEMENT: I represent that my thesis or dissertation and abstract are my original work. Proper attribution has been given to all outside sources. I understand that I am solely responsible for obtaining any needed copyright permissions. I have obtained needed written permission statement(s) from the owner(s) of each third-party copyrighted matter to be included in my work, allowing electronic distribution (if such use is not permitted by the fair use doctrine) which will be submitted to UKnowledge as Additional File. I hereby grant to The University of Kentucky and its agents the irrevocable, non-exclusive, and royalty-free license to archive and make accessible my work in whole or in part in all forms of media, now or hereafter known. -

Antifungal Pharmacologypharmacology
AntifungalAntifungal PharmacologyPharmacology Deborah Fox, Ph.D. Children’s Hospital 3219 RIC 504-896-2766 [email protected] Special thanks to: John Perfect, MD Andy Alspaugh, MD Sevtap Arikan, MD John Rex, MD www.doctorfungus.org Objectives • To recognize the clinical significance of fungal infections • To identify the antifungal agents and their mechanisms of action • To evaluate potential antifungal drug interactions and toxicities • To differentiate the mechanisms of antifungal drug resistance LectureLecture outlineoutline • Clinical significance of fungal infection • Fungal cell structure and targets • Antifungal agents and mechanism of action • Antifungal drug interactions & nephrotoxicity • Mechanisms of antifungal resistance • Summary MycologyMycology ResourcesResources • http://www.doctorfungus.org • http://mycology.adelaide.edu.au/mycoses • http://mycology.cornell.edu/ • http://www.mycology.net/ LectureLecture outlineoutline • Clinical significance of fungal infection • Fungal cell structure and targets • Antifungal agents and mechanism of action • Antifungal drug interactions & nephrotoxicity • Mechanisms of antifungal resistance • Summary MedicalMedical ProblemsProblems CausedCaused byby FungiFungi 1) Allergic disease 2) “Mushroom” poisoning 3) Mycotoxins Secondary metabolites --many have industrial uses --Fusarium mycotoxin -- USSR after WWII --A. flavus “aflatoxin” 4) Mycoses -- infection and resulting disease cause by fungi TheThe FungiFungi 150 primary human fungal pathogens 100,000 Validly described species of fungi Fungi yet to be discovered -Kwon-Chung and Bennett, 1992 TheThe FungiFungi 150 primary human fungal pathogens 100,000 Validly described species of fungi Fungi yet to be discovered -Kwon-Chung and Bennett, 1992 TheThe FungiFungi Candida, 150 Aspergillus, primary human Crypto, Blasto, Histo, Cocci, Dermatophytes fungal pathogens 100,000 Validly described species of fungi Fungi yet to be discovered -Kwon-Chung and Bennett, 1992 RecentRecent eventsevents inin fungalfungal diseasesdiseases Problems of today: a. -
Alphabetical Listing by Therapeutic Category Dod UNIFORM
DoD UNIFORM OUTPATIENTFORMULARY Alphabetical Listing by Therapeutic Category This document is current as of July 14, 2021 The availability of formulary items is subject to change. 1 ABORTIFACIENT Abortifacient Dextromethorphan and Chlorpheniramine .............................................35 Carboprost Tromethamine ..................................................................... 23 Hydrocodone and Chlorpheniramine ..................................................... 60 Dinoprostone .......................................................................................... 37 Ibuprofen, Phenylephrine, and Chlorpheniramine ................................. 62 MiFEPRIStone ........................................................................................81 Ibuprofen, Pseudoephedrine, and Chlorpheniramine ............................ 62 Naphazoline and Pheniramine ...............................................................83 Acetylcholinesterase Inhibitor Triprolidine ............................................................................................ 116 Echothiophate Iodide ............................................................................. 40 Triprolidine and Pseudoephedrine ....................................................... 117 Edrophonium .......................................................................................... 40 Edrophonium and Atropine .................................................................... 41 Allergen-Specific Immunotherapy Neostigmine ............................................................................................84 -

(12) Patent Application Publication (10) Pub. No.: US 2006/0165747 A1 Rof (43) Pub
US 2006O165747A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0165747 A1 ROf (43) Pub. Date: Jul. 27, 2006 (54) ANTIFUNGAL COMPOSITION, METHOD (52) U.S. Cl. ...................................... 424/405; 514/254.07 AND KIT FOR TOPCALLY TREATING ONYCHOMYCOSIS (57) ABSTRACT (76) Inventor: David Rolf, Eden Prairie, MN (US) Correspondence Address: An activator comprising a biocompatible base and a known James V. Harmon fungicide in the form of an acid salt are mixed together by US Bank Plaza the user shortly before being applied to the infection so as to Suite 2000 react them chemically to produce the free base of the 220 South Sixth Street fungicide thereby rendering the composition capable of Minneapolis, MN 55402 (US) penetrating throughout the infected tissue. The free base form has been found to be much more lethal to the fungal (21) Appl. No.: 11/040,725 infection, particularly in the treatment of onychomycosis. The activator is formulated to be mixed within a few days of (22) Filed: Jan. 24, 2005 or just before application with the fungicide, e.g., terbinafine hydrochloride (an acid salt). Although the free base is Publication Classification Subject to degradation and has a shorter shelf life, it was found that mixing just prior to use eliminates problems that (51) Int. C. could be caused by degradation of an active ingredient. A A6 IK 3/496 (2006.01) preferred activator Solution also contains a penetration AOIN 25/00 (2006.01) enhancer and a tissue softener. US 2006/01 65 747 A1 Jul. 27, 2006 ANTIFUNGAL COMPOSITION, METHOD AND 0007. -

(Athlete's Foot)? Orally Administered Antifungal Agents Are Expensive EVIDENCE-BASED ANSWER and Can Have Systemic Side Effects
CLINICAL INQUIRIES What is the most effective treatment for 11 RCTs suggests that allylamines are slightly more effec- tive than azoles. tinea pedis (athlete's foot)? Orally administered antifungal agents are expensive EVIDENCE-BASED ANSWER and can have systemic side effects. Griseofulvin and Topical therapy is effective for tinea pedis. Topical ketoconazole are approved for oral therapy, but prod- terbinafine has a 70% cure rate, is available over the uct labels clearly state that they should be used only counter (OTC), and requires only 1 to 2 weeks of ther- after topical agents have failed. Griseofulvin has been apy. Two other OTC topicals, tolnaftate and micona- used for more than 30 years, is well tolerated, and effi- zole, require 2 to 4 weeks to achieve slightly lower cure cacious in treating dermatomycoses in the range of rates, but are considerably less expensive. (Grade of 60%.3 Ketoconazole's cure rate is similar, but its use in recommendation: A) cutaneous infections is limited by multiple drug inter- The most effective treatment for tinea pedis is oral actions and serious side effects. Three placebo-con- terbinafine 250 mg twice a day for 2 weeks (94% clini- trolled RCTs of itraconazole of varying doses and dura- cal cure rate). However, oral terbinafine is expensive tion of treatment suggested favorable clinical cure of and not approved for this indication. Oral therapy may moccasin-type tinea pedis (51%-85%) . The most effec- be required for patients with hyperkerototic soles, tive itraconazole regimen was 200 mg twice daily for 1 severe disease, topical therapy failure, chronic infection week.