What Published Literature Tells Us About Nanosilver
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Scabies in Healthcare Facilities
Scabies in Healthcare Facilities Tammra L. Morrison, RN BSN Healthcare Associated Infections Coordinator Communicable Disease Branch, Epidemiology Section December 9, 2016 Symptoms • In a person who has never had scabies: • May take 4-6 weeks for symptom onset • In a person who has had scabies in the past: • Symptoms may start in 1-4 days • May be spread PRIOR to symptom onset What to Look for • Intense itching • Especially at night • Pimple-like itchy rash • May affect entire body OR Dermatologie.md common sites: • Wrist, elbow, armpit, webbing between the fingers, nipple, penis, waist, belt-line, and buttocks • Burrows (tunnels) may be seen on the skin • Tiny raised and crooked grayish-white or skin- colored lines Transmission • Direct, prolonged, skin-to-skin contact with an infested person • Sexual partners • Household members • Quick handshake/hug will usually not spread scabies How Long Do Mites Live? • 1-2 months on a person • 48-72 hours off a person • Scabies mites will die at 122 degrees for 10 minutes Webmd.com 5 Diagnosis • Customary appearance and distribution of the rash and presence of burrows. • Confirm diagnosis: • Obtain a skin scraping to examine under a microscope for mites, eggs, or mite fecal matter • Person can still be infested even if mites, eggs, or fecal matter cannot be found • Typically fewer than 10-15 mites present on the entire body • **Crusted scabies may be thousands of mites and should be considered highly contagious** How Do You Treat Scabies? 7 Treatment • Available only by prescription • No "over-the-counter“ -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

CCA Senior Care Options Formulary
Commonwealth Care Alliance Senior Care Option HMO SNP 2021 List of Covered Drugs Formulary 30 Winter Street • Boston, MA 02108 PLEASE READ: THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN This formulary was updated on 08/01/2021. For more recent information or other questions, please contact Senior Care Options Program (HMO SNP) Member Services, at 1-866-610-2273 or, for TTY users, 711, 8 a.m. – 8 p.m., 7 days a week, or visit www.commonwealthcaresco.org. HPMS Approved Formulary File Submission ID 00021589, Version Number 13 Senior Care Options Program (HMO SNP) 2021 Formulary (List of Covered Drugs) PLEASE READ: THIS DO CUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN HPMS Approved Formulary File Submission ID 00021589, Version Number 13 Note to existing members: This formulary has changed since last year. Please review this document to make sure that it still contains the drugs you take. When this drug list (formulary) refers to “we,” “us”, or “our,” it means Commonwealth Care Alliance. When it refers to “plan” or “our plan,” it means 2021 Senior Care Options Program. This document includes list of the drugs (formulary) for our plan which is current as of 08/01/2021. This formulary document applies to all SCO members. For an updated formulary, please contact us. Our contact information, along with the date we last updated the formulary, appears on the front and back cover pages. You must generally use network pharmacies to use your prescription drug benefit. Benefits, formulary, pharmacy n etwork, and/or copayments/coinsurance may change on January 1, 2022, and from time to time during the year. -

Therapeutic Class Overview Antifungals, Topical
Therapeutic Class Overview Antifungals, Topical INTRODUCTION The topical antifungals are available in multiple dosage forms and are indicated for a number of fungal infections and related conditions. In general, these agents are Food and Drug Administration (FDA)-approved for the treatment of cutaneous candidiasis, onychomycosis, seborrheic dermatitis, tinea corporis, tinea cruris, tinea pedis, and tinea versicolor (Clinical Pharmacology 2018). The antifungals may be further classified into the following categories based upon their chemical structures: allylamines (naftifine, terbinafine [only available over the counter (OTC)]), azoles (clotrimazole, econazole, efinaconazole, ketoconazole, luliconazole, miconazole, oxiconazole, sertaconazole, sulconazole), benzylamines (butenafine), hydroxypyridones (ciclopirox), oxaborole (tavaborole), polyenes (nystatin), thiocarbamates (tolnaftate [no FDA-approved formulations]), and miscellaneous (undecylenic acid [no FDA-approved formulations]) (Micromedex 2018). The topical antifungals are available as single entity and/or combination products. Two combination products, nystatin/triamcinolone and Lotrisone (clotrimazole/betamethasone), contain an antifungal and a corticosteroid preparation. The corticosteroid helps to decrease inflammation and indirectly hasten healing time. The other combination product, Vusion (miconazole/zinc oxide/white petrolatum), contains an antifungal and zinc oxide. Zinc oxide acts as a skin protectant and mild astringent with weak antiseptic properties and helps to -

Salicylic Acid
Treatment Guide to Common Skin Conditions Prepared by Loren Regier, BSP, BA, Sharon Downey -www.RxFiles.ca Revised: Jan 2004 Dermatitis, Atopic Dry Skin Psoriasis Step 1 - General Treatment Measures Step 1 - General Treatment Measures Step 1 • Avoid contact with irritants or trigger factors • Use cool air humidifiers • Non-pharmacologic measures (general health issues) • Avoid wool or nylon clothing. • Lower house temperature (minimize perspiration) • Moisturizers (will not clear skin, but will ↓ itching) • Wash clothing in soap vs detergent; double rinse/vinegar • Limit use of soap to axillae, feet, and groin • Avoid frequent or prolonged bathing; twice weekly • Topical Steroids Step 2 recommended but daily bathing permitted with • Coal Tar • Colloidal oatmeal bath products adequate skin hydration therapy (apply moisturizer • Anthralin • Lanolin-free water miscible bath oil immediately afterwards) • Vitamin D3 • Intensive skin hydration therapy • Limit use of soap to axillae, feet, and groin • Topical Retinoid Therapy • “Soapless” cleansers for sensitive skin • Apply lubricating emollients such as petrolatum to • Sunshine Step 3 damp skin (e.g. after bathing) • Oral antihistamines (1st generation)for sedation & relief of • Salicylic acid itching give at bedtime +/- a daytime regimen as required Step 2 • Bath additives (tar solns, oils, oatmeal, Epsom salts) • Topical hydrocortisone (0.5%) for inflammation • Colloidal oatmeal bath products Step 2 apply od-tid; ointments more effective than creams • Water miscible bath oil • Phototherapy (UVB) may use cream during day & ointment at night • Humectants: urea, lactic acid, phospholipid • Photochemotherapy (Psoralen + UVA) Step 4 Step 3 • Combination Therapies (from Step 1 & 2 treatments) • Prescription topical corticosteroids: use lowest potency • Oral antihistamines for sedation & relief of itching steroid that is effective and wean to twice weekly. -

Dermatological Effects of Different Keratolytic Agents on Acne Vulgaris
Clin l of ica a l T n r r i u a l o s J Alodeani, J Clin Trials 2016, 6:2 Journal of Clinical Trials DOI: 10.4172/2167-0870.1000262 ISSN: 2167-0870 Research Article Open Access Dermatological Effects of Different Keratolytic Agents on Acne Vulgaris Essa Ajmi Alodeani* College of Medicine at AD-Dwadmi, Shaqra University, Saudi Arabia *Corresponding author: Essa Ajmi Alodeani, College of Medicine at AD-Dwadmi, Shaqra University, Saudi Arabia, Tel: +966 55 075 9042; E-mail: [email protected] Received date: March 24, 2016; Accepted date: April 18, 2016; Published date: April 25, 2016 Copyright: © 2016 Alodeani EA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Acne vulgaris is a chronic inflammatory skin disease; it's one of the most common skin disorders and affects mainly adolescents and young adults. Keratolytic agents are widely used in treatment of acne from several years. In this study we aimed to evaluate and compare the cutaneous response of different keratolytic agents in management of acne vulgaris. Ninety patients were selected among those attending the outpatient dermatology clinic in AD- Dwadmi hospital during the period from October 2015 to February 2016. The selected patients had different forms of acne vulgaris, papulo-pustular, comedonal and post acne scar. Three types of keratolytic agents were used, glycolic acid 50%, salicylic acid 20% and jessner solution. In papulopustular lesions, the three agents were effective with non-significant difference between them; however, there was more excellent results with jessner solution (70 % of patients) then glycolic acid (50%) and lastly salicylic acid (40%). -

Assessment Report on Melaleuca Alternifolia (Maiden and Betch) Cheel, M
24 November 2014 EMA/HMPC/320932/2012 Committee on Herbal Medicinal Products (HMPC) Assessment report on Melaleuca alternifolia (Maiden and Betch) Cheel, M. linariifolia Smith, M. dissitiflora F. Mueller and/or other species of Melaleuca, aetheroleum Based on Article 16d(1), Article 16f and Article 16h of Directive 2001/83/EC as amended (traditional use) Final Herbal substance(s) (binomial scientific name of Melaleuca alternifolia (Maiden and Betch) Cheel, the plant, including plant part) M. linariifolia Smith, M. dissitiflora F. Mueller and/or other species of Melaleuca, leaf and terminal branchlets Herbal preparation(s) Melaleuca alternifolia, aetheroleum Pharmaceutical forms Herbal preparation in liquid and semi-solid dosage forms for cutaneous use or in liquid dosage form for oromucosal use. Rapporteur Marisa Delbò Assessor(s) Marisa Delbò Gioacchino Calapai Peer-reviewer Jacqueline Viguet Poupelloz 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2015. Reproduction is authorised provided the source is acknowledged. Table of contents Table of contents ................................................................................................................... 2 1. Introduction ....................................................................................................................... 5 1.1. Description of the herbal substance(s), -
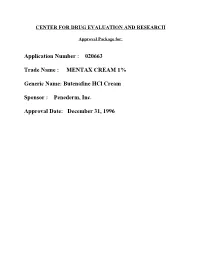
MENTAX CREAM 1% Generic Name: Butenafine Hcl Cream Sponsor : Penederm
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: Application Number : 020663 Trade Name : MENTAX CREAM 1% Generic Name: Butenafine HCl Cream Sponsor : Penederm, Inc. Approval Date: December 31, 1996 CENTER FOR DRUG EVALUATION AND RESEARCH Application Number 020663 APPROVAL LETTER DEC 3 I IW NDA 20-663 Penederm Incolpxated Attentiom John Quigley, Ph.D. Senior Vice President, Research and Development 320 Lakeside Drive, Suite A Foster City, CA W Dear Dr. QuigIey: Please refer to your December 22, 1995, new drug application submitted under section 505(b) of the Federal F@ Drug, and Cosmetic Act for Mentax (butenafine hydrochloride cream) cream, 1%. ● We acknowledge receipt of your amendments and correspondence dated December 27, 1995fi~ January 8 and 19, March 1 (two), 27 and 28, October 23,24 and 25, November 5 and 15, and December 12 and 31,1996. This new drug application provides for the treatment of tines corporis and tines cruris. We have completed the review of this application and have concluded that ;dequate information has been presented to demonstrate that the drug product is safe and effective for use as recommended in the enclosed revised draft labeling.- Accordingly, the application is approved effective on the date of this letter. The final printed labeling (FPL) must be identical to the enclosed revised drall labeling. The enclosed revised draft labeling was stated to be acceptable to you in the facsimile of your letter dated December 31,1996. Marketing the product with FPL that is not identical to the enclosed revised drafl labeling may render the product misbranded and an unapproved new drug. -

Jp Xvii the Japanese Pharmacopoeia
JP XVII THE JAPANESE PHARMACOPOEIA SEVENTEENTH EDITION Official from April 1, 2016 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the convenience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 64 Pursuant to Paragraph 1, Article 41 of the Law on Securing Quality, Efficacy and Safety of Products including Pharmaceuticals and Medical Devices (Law No. 145, 1960), the Japanese Pharmacopoeia (Ministerial Notification No. 65, 2011), which has been established as follows*, shall be applied on April 1, 2016. However, in the case of drugs which are listed in the Pharmacopoeia (hereinafter referred to as ``previ- ous Pharmacopoeia'') [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as ``new Pharmacopoeia'')] and have been approved as of April 1, 2016 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as of March 31, 2016 as those exempted from marketing approval pursuant to Paragraph 1, Article 14 of the Same Law (hereinafter referred to as ``drugs exempted from approval'')], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on September 30, 2017. -

Oral Alitretinoin in Congenital Ichthyosis: a Pilot Study Shows Variable Effects and a Risk of Central Hypothyroidism
Included in the theme issue: 256 Letters to the Editor ACNE, RETINOIDS AND LYMPHOMAS Acta Derm Venereol 2012; 92: 256–257 Oral Alitretinoin in Congenital Ichthyosis: A Pilot Study Shows Variable Effects and a Risk of Central Hypothyroidism Agneta Gånemo1, Mette Sommerlund2 and Anders Vahlquist3* 1Department of Dermatology, Institute of Clinical Research in Malmö, Lund University, Skåne University Hospital, Malmö, Sweden, 2Department of Dermatology and Venereology, Aarhus University Hospital, Aarhus, Denmark, and 3Department of Medical Sciences (Dermatology), Uppsala University, Uppsala, Sweden. E-mail: [email protected] Accepted October 20, 2011. Congenital ichthyosis is a large group of hereditary skin planned treatment period of 3 months. Clinical and laboratory disorders with different aetiologies, all of which are pre- evaluations were performed before the start of therapy and at monthly intervals, and consisted of physical examination, pho- sent at birth (1). The patients have dry, widespread scaling tography, interviewing the patients about effects and side-effects and thickened skin (2). At present there is no cure for of therapy, and blood sampling for analysis of haematological ichthyosis and therapy is mostly symptomatic. Life-long parameters, liver enzymes, creatinine, cholesterol, triglycerides, treatment with emollients is essential, and some patients thyroxin (T4) and tyroid-stimulating hormone (TSH) levels. also use systemic therapy with retinoids, especially aci- tretin (3). The most serious adverse effect of retinoids is RESULTS teratogenicity, which is a special concern for acitretin as it is excreted from the body slowly (3). All 4 patients completed the 3-month long trial, and two Alitretinoin (9-cis retinoic acid) is a fairly new oral of them (nos 1 and 3) wished to continue alitretinoin retinoid with more rapid clearance than acitretin. -

History of Formulary Changes Contents
History of Formulary Changes Pre-Single PDL Changes (before October 1, 2020) Revised for 11/1/2020 Contents Medicaid Health Plan Common Formulary Changes Effective October 1, 2020 ................................................................................................................................... 2 Medicaid Health Plan Common Formulary Changes Effective July 1, 2020 .......................................................................................................................................... 4 Medicaid Health Plan Common Formulary Changes Effective April 1, 2020 ........................................................................................................................................ 6 Medicaid Health Plan Common Formulary Changes Effective January 1, 2020 .................................................................................................................................... 8 Medicaid Health Plan Common Formulary Changes Effective October 1, 2019 ................................................................................................................................. 10 Medicaid Health Plan Common Formulary Changes Effective July 1, 2019 ........................................................................................................................................ 12 Medicaid Health Plan Common Formulary Changes Effective April 1, 2019 ...................................................................................................................................... 14 -

ED227273.Pdf
DOCUMENT RESUft ED 227 273 y CE 035 300 ' TITLE APharmacy Spicialist, Militkry Curriculum Materials for Vocation47 andileChlaical Education. INSTITuTION Air Force Training Command, Sheppa* AFB, Tex.; Ohio State Univ., Columbus. Natfonal Center for Research in Vocational Education. SPONS AGENCY Office of Education (DHEW)x Washington, D.C. PUB DATE 18 Jul 75 NOTE 774p.; Some pages are marginally legible. ,PUB TYPE Guides - Classroom Use Guides (For Teachers) (052), , EDRS ?RICE 14P05/PC31 Plus Postage. ` DESCRIPTORS Behavioral Objectives; Course Descriptions; A Curriculum Guides; Drug Abuse; Drug,Therapy; 4Drug Use; Learning Activities; Lesson Plans; *Pharmaceutical Education; Pharmacists; *Pharmacology; *Pharmacy; Postsecondary Education; Programed Instructional Materials; Textbooks; Workbooks IDENTIFIERS. Military CuFr.iculum Project liBSTRACT These teacher and studdnt,materials for a . postsecondary-level course in pharmacy comprise one of a numberof military-developed curriculum packages selected for adaptation to voCational instruction 'and curriculum dei7elopment in acivilian setting. The purpose stated for the 256-hour course iS totrain students in the basic technical phases of pharmacy and theminimum essential knowledge and skills necessaryior.the compounding and - dispensing of drugs, the economical operation of a pharmacy,and the proper use of drugs, chemicals, andbiological products. The course consists of three blocks of instruction. Block I contains four, lessons: pharmaceutical calculations I and laboratory,inorganic chemistry, and organic chemistry. The five lessons in Block II cover anatomy ,and physiology, introduction topharmacoloe, toxicology, drug abuse, and pharmaceutical and medicinal agents. Block III provides five lessons: phdrmaceutical calculations\I and II, techniques"of pharmaceutical compounding, pharmaceutiCal dosage for s, and compounding laboratbry. Instructormaterials include a cb se chart, lesson plans, and aplan of instruction detailing instructional,bnits, criterion objectives, lesson duration,and support materials needed.