Primary Health Care in Rural Southland
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te Anau Area Community Response Plan 2019
Southland has NO Civil Defence sirens (fire brigade sirens are not used to warn of Civil Defence emergency) Please take note of natural warning signs as your first and best warning for any emergency. Te Anau Area Community Response Plan 2019 Find more information on how you can be prepared for an emergency www.cdsouthland.nz In the event of an emergency, communities may need to support themselves for up to 10 days before assistance arrives. Community Response Planning The more prepared a community is the more likely it is that the community will be able to look after themselves and others. This plan contains a short demographic description of information for the Te Anau area, including key hazards and risks, information about Community Emergency Hubs where the community can gather, and important contact information to help the community respond effectively. Members of the Te Anau and Manapouri Community Response Groups have developed the information contained in this plan and will be Emergency Management Southlands first points of community contact in an emergency. The Te Anau/Manapouri Response Group Procedure and Milford Sound Emergency Response Plan include details for specific response planning for the Te Anau and wider Fiordland areas. Demographic details • Te Anau and Manapouri are contained within the Southland District Council area. • Te Anau has a resident population of approx. 2,000 people. • Manapouri has a resident population of approx. 300 people • Te Anau Airport, Manapouri is located 15 km south of Te Anau and 5 km north of Manapouri, on State Highway 95 • The basin community has people from various service industries, tourism-related businesses, Department of Conservation, fishing, transport, food, catering, and farming. -
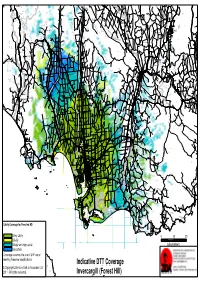
Indicative DTT Coverage Invercargill (Forest Hill)
Blackmount Caroline Balfour Waipounamu Kingston Crossing Greenvale Avondale Wendon Caroline Valley Glenure Kelso Riversdale Crossans Corner Dipton Waikaka Chatton North Beaumont Pyramid Tapanui Merino Downs Kaweku Koni Glenkenich Fleming Otama Mt Linton Rongahere Ohai Chatton East Birchwood Opio Chatton Maitland Waikoikoi Motumote Tua Mandeville Nightcaps Benmore Pomahaka Otahu Otamita Knapdale Rankleburn Eastern Bush Pukemutu Waikaka Valley Wharetoa Wairio Kauana Wreys Bush Dunearn Lill Burn Valley Feldwick Croydon Conical Hill Howe Benio Otapiri Gorge Woodlaw Centre Bush Otapiri Whiterigg South Hillend McNab Clifden Limehills Lora Gorge Croydon Bush Popotunoa Scotts Gap Gordon Otikerama Heenans Corner Pukerau Orawia Aparima Waipahi Upper Charlton Gore Merrivale Arthurton Heddon Bush South Gore Lady Barkly Alton Valley Pukemaori Bayswater Gore Saleyards Taumata Waikouro Waimumu Wairuna Raymonds Gap Hokonui Ashley Charlton Oreti Plains Kaiwera Gladfield Pikopiko Winton Browns Drummond Happy Valley Five Roads Otautau Ferndale Tuatapere Gap Road Waitane Clinton Te Tipua Otaraia Kuriwao Waiwera Papatotara Forest Hill Springhills Mataura Ringway Thomsons Crossing Glencoe Hedgehope Pebbly Hills Te Tua Lochiel Isla Bank Waikana Northope Forest Hill Te Waewae Fairfax Pourakino Valley Tuturau Otahuti Gropers Bush Tussock Creek Waiarikiki Wilsons Crossing Brydone Spar Bush Ermedale Ryal Bush Ota Creek Waihoaka Hazletts Taramoa Mabel Bush Flints Bush Grove Bush Mimihau Thornbury Oporo Branxholme Edendale Dacre Oware Orepuki Waimatuku Gummies Bush -

The New Zealand Gazette. 331
JAN. 20.] THE NEW ZEALAND GAZETTE. 331 MILITARY AREA No, 12 (INVERCARGILL)-continued. MILITARY AREA No.· 12 (INVERCARGILL)-oontinued. 499820 Irwin, Robert William Hunter, mail-contractor, Riversdale, 532403 Kindley, Arthur William,·farm labourer, Winton. Southland. 617773 King, Duncan McEwan, farm hand, South Hillend Rural 598228 Irwin, Samuel David, farmer, Winton, Otapiri Rural Delivery, Winton. Delivery, Brown. 498833 King, Robert Park, farmer, Orepuki, Rural Delivery, 513577 Isaacs, Jack, school-teacher, The School, Te Anau. Riverton-Tuatapere. 497217 Jack, Alexander, labourer, James St., Balclutha. 571988 King, Ronald H. M., farmer, Orawia. 526047 Jackson, Albert Ernest;plumber, care of R. G. Speirs, Ltd., 532584 King, Thomas James, cutter, Rosebank, Balclutha. Dee St., Invercargill. 532337 King, Tom Robert, agricultural contractor, Drummond. 595869 James, Francis William, sheep,farmer, Otautau. 595529 Kingdon, Arthur Nehemiah, farmer, Waikaka Rural De. 549289 James, Frederick Helmar, farmer, Bainfield Rd., Waiki.wi livery, Gore. West Plains Rural Delivery, Inveroargill, 595611 Kirby, Owen Joseph, farmer, Cardigan, Wyndham. 496705 James, Norman Thompson, farmer, Otautau, Aparima 571353 Kirk, Patrick Henry, farmer, Tokanui, Southland. Rural Delivery, Southland. 482649 Kitto, Morris Edward, blacksmith, Roxburgh. 561654 Jamieson, Thomas Wilson, farmer, Waiwera South. 594698 Kitto, Raymond Gordon, school-teacher, 5 Anzac St., Gore. 581971 Jardine, Dickson Glendinning, sheep-farmer, Kawarau Falls 509719 Knewstubb, Stanley Tyler, orchardist, Coal Creek Flat, Station, Queenstown. Roxburgh. , 580294 Jeffrey, Thomas Noel, farmer, Wendonside Rural Delivery, 430969 Knight, David Eric Sinclair, tallow assistant, Selbourne St. Gore. Mataura. 582520 Jenkins, Colin Hendry, farm manager, Rural Delivery, 467306 Knight, John Havelock, farmer, Riverton, Rural Delivery, · Balclutha. Tuatapere. 580256 Jenkins, John Edward, storeman - timekeeper, Homer 466864 Knight, Ralph Condie, civil servant, 83 Ohara St., Inver. -

Section 6 Schedules 27 June 2001 Page 197
SECTION 6 SCHEDULES Southland District Plan Section 6 Schedules 27 June 2001 Page 197 SECTION 6: SCHEDULES SCHEDULE SUBJECT MATTER RELEVANT SECTION PAGE 6.1 Designations and Requirements 3.13 Public Works 199 6.2 Reserves 208 6.3 Rivers and Streams requiring Esplanade Mechanisms 3.7 Financial and Reserve 215 Requirements 6.4 Roading Hierarchy 3.2 Transportation 217 6.5 Design Vehicles 3.2 Transportation 221 6.6 Parking and Access Layouts 3.2 Transportation 213 6.7 Vehicle Parking Requirements 3.2 Transportation 227 6.8 Archaeological Sites 3.4 Heritage 228 6.9 Registered Historic Buildings, Places and Sites 3.4 Heritage 251 6.10 Local Historic Significance (Unregistered) 3.4 Heritage 253 6.11 Sites of Natural or Unique Significance 3.4 Heritage 254 6.12 Significant Tree and Bush Stands 3.4 Heritage 255 6.13 Significant Geological Sites and Landforms 3.4 Heritage 258 6.14 Significant Wetland and Wildlife Habitats 3.4 Heritage 274 6.15 Amalgamated with Schedule 6.14 277 6.16 Information Requirements for Resource Consent 2.2 The Planning Process 278 Applications 6.17 Guidelines for Signs 4.5 Urban Resource Area 281 6.18 Airport Approach Vectors 3.2 Transportation 283 6.19 Waterbody Speed Limits and Reserved Areas 3.5 Water 284 6.20 Reserve Development Programme 3.7 Financial and Reserve 286 Requirements 6.21 Railway Sight Lines 3.2 Transportation 287 6.22 Edendale Dairy Plant Development Concept Plan 288 6.23 Stewart Island Industrial Area Concept Plan 293 6.24 Wilding Trees Maps 295 6.25 Te Anau Residential Zone B 298 6.26 Eweburn Resource Area 301 Southland District Plan Section 6 Schedules 27 June 2001 Page 198 6.1 DESIGNATIONS AND REQUIREMENTS This Schedule cross references with Section 3.13 at Page 124 Desig. -

Queenstown, Milford Sound, Doubtful Sound, Te Anau
For all enquiries and reservations contact a Real Journeys Visitor Centre Queenstown, QUEENSTOWN: 88 Beach Street, Steamer Wharf Milford Sound, TE ANAU: 85 Lakefront Drive MANAPOURI: 64 Waiau Street Doubtful Sound, FREEPHONE 0800 65 65 01 Te Anau & [email protected] www.realjourneys.co.nz Stewart Island See our website for more info and booking conditions ACTIVITY GUIDE Check us out on: VGDLE 06/16 VGDLE Printed in New Zealand using environmentally friendly inks and paper ABOUT US 02 MILFORD SOUND Nature Cruises 04 Scenic Cruises 06 Overnight Cruises 08 Getting to Milford Sound 10 Milford Track Day Walk 12 WELCOME TE ANAU Let us introduce you to this Te Anau Glowworm Caves 14 stunning wilderness we call DOUBTFUL SOUND / MANAPOURI home… Southern New Zealand. Wilderness Cruises 16 Overnight Cruises 18 Manapouri Underground Power Station 20 MULTI-DAY DISCOVERY EXPEDITIONS 22 QUEENSTOWN TSS Earnslaw Steamship Cruises 24 Walter Peak High Country Farm 26 Colonel's Homestead Restaurant 28 Walter Peak Guided Cycling 30 Walter Peak Horse Treks 31 Cardrona Alpine Resort 44 Queenstown Rafting 43 STEWART ISLAND Ferry Services 32 Paterson Inlet Cruises 34 Rental Services 35 Village and Bays Tours 36 Guided Walks 37 Stewart Island Lodge 38 CHRISTCHURCH / AKAROA International Antarctic Centre 40 Black Cat Cruises 42 PROMOTIONS 13 CONSERVATION 46 SUGGESTED ITINERARIES / MAPS 48 MILFORD SOUND, FIORDLAND NATIONAL PARK FIORDLANDMILFORD SOUND, NATIONAL Be it rescuing the TSS Earnslaw from being scuttled and turning it into a national icon; The journey introducing overnight cruises in Fiordland; or designing unique glass roofed coaches to maximize the view, Real Journeys has always been at the forefront of the tourism so far.. -

Waste Options in Rural Southland
Waste Options in Rural Southland armers have always been great at giving new life to old materials, but there is plenty Fmore that can be done to improve waste management on the farm. Southland has a variety of waste facilities ranging from recycling centres where people freely drop off recyclables to waste transfer stations that accept household and commercial rubbish. Rural Refuse Collection Rural properties have several options for rubbish collection. Private contractors that offer collection services are listed in the yellow pages under ‘Waste Disposal’ and ‘Recycling’. However it could be just as easy to take your rubbish/recycling to the nearest transfer station, or recycling to your local recycling centre. Waste Transfer Stations Waste Transfers Stations are for the disposal of rubbish, greenwaste (garden waste), scrap metal recyclables, pre-loved materials and small quantities of hazardous chemicals. Some fees do apply. • Lumsden Transfer Station, 35 Oxford Street, Lumsden • Otautau Transfer Station, 5 Bridport Road, Otautau • Riverton Transfer Station, 1 Havelock Street, Riverton • Gore Transfer Station, Toronto Street, Gore • Invercargill Waste Transfer Station, 303 Bond Street, Invercargill • Bluff Transfer Station, 75 Suir Street, Bluff • Wyndale Transfer Station, 190 Edendale Wyndham Road, Edendale • Winton Transfer Station, 193 Florence Road, Winton • Te Anau Transfer Station, Te Anau Manapouri Highway, Te Anau Recycle Drop-off Centre There are recycle drop-off centres located throughout the district for household recyclables. -

Bullinggillianm1991bahons.Pdf (4.414Mb)
THE UNIVERSITY LIBRARY PROTECTION OF AUTHOR ’S COPYRIGHT This copy has been supplied by the Library of the University of Otago on the understanding that the following conditions will be observed: 1. To comply with s56 of the Copyright Act 1994 [NZ], this thesis copy must only be used for the purposes of research or private study. 2. The author's permission must be obtained before any material in the thesis is reproduced, unless such reproduction falls within the fair dealing guidelines of the Copyright Act 1994. Due acknowledgement must be made to the author in any citation. 3. No further copies may be made without the permission of the Librarian of the University of Otago. August 2010 Preventable deaths? : the 1918 influenza pandemic in Nightcaps Gillian M Bulling A study submitted for the degree of Bachelor of Arts with Honours at the University of Otago, Dunedin, New Zealand. 1991 Created 7/12/2011 GILLIAN BULLING THE 1918 INFLUENZA PANDEMIC IN NIGHTCAPS PREFACE There are several people I would like to thank: for their considerable help and encouragement of this project. Mr MacKay of Wairio and Mrs McDougall of the Otautau Public Library for their help with the research. The staff of the Invercargill Register ofBirths, Deaths and Marriages. David Hartley and Judi Eathorne-Gould for their computing skills. Mrs Dorothy Bulling and Mrs Diane Elder 3 TABLE OF CONTENTS List of Tables and Figures 4 List of illustrations 4 Introduction , 6 Chapter one - Setting the Scene 9 Chapter two - Otautau and Nightcaps - Typical Country Towns? 35 Chapter three - The Victims 53 Conclusion 64 Appendix 66 Bibliography 71 4 TABLE OF ILLUSTRATIONS Health Department Notices .J q -20 Source - Southland Times November 1918 Influenza Remedies. -

Queenstown, Milford Sound, Doubtful Sound, Te Anau & Stewart Island
“ Even torrential rain adds to the atmosphere For all enquiries and reservations Queenstown, contact a Real Journeys Visitor Centre of this magical place, as an ethereal mist QUEENSTOWN: 88 Beach Street, Steamer Wharf descends, periodically lifting to reveal the TE ANAU: 85 Lakefront Drive Milford Sound, MANAPOURI: 64 Waiau Street waterfalls at their thunderous best.” FREEPHONE 0800 65 65 01 Doubtful Sound, ROUGH GUIDE TO NEW ZEALAND [email protected] www.realjourneys.co.nz Te Anau & Stewart Island See our website for more info and booking conditions ACTIVITY GUIDE Check us out on: VGA4 06/16 VGA4 Printed in New Zealand using environmentally friendly inks and paper ABOUT US 2 - 3 MILFORD SOUND Nature Cruises 4 - 5 Scenic Cruises 6 - 7 Overnight Cruises 8 - 9 Getting to Milford Sound 10 - 11 Milford Track Day Walk 13 TE ANAU Te Anau Glowworm Caves 14 - 15 Let us introduce you to this DOUBTFUL SOUND Wilderness Cruises 16 - 17 stunning wilderness we call Overnight Cruises 18 - 19 home… Southern New Zealand. DISCOVERY EXPEDITIONS 20 - 21 QUEENSTOWN TSS Earnslaw Steamship Cruises 22 - 23 Walter Peak Farm Tours 24 - 25 Colonel’s Homestead Restaurant 26 - 27 Walter Peak Cycling 28 Walter Peak Horse Treks 28 Cardrona Alpine Resort 29 Queenstown Rafting 30 SPECIAL EVENTS & FUNCTIONS 31 STEWART ISLAND Ferry Services 32 - 33 Rental Services 33 Paterson Inlet Cruises 34 Village & Bays Tours 35 Guided Walks 35 Stewart Island Lodge 36 CHRISTCHURCH / AKAROA International Antarctic Centre 38 Black Cat Cruises 39 CONSERVATION 12 PROMOTIONS 37 SUGGESTED ITINERARIES & MAPS 40 - 42 MILFORD SOUND, FIORDLAND NATIONAL PARK FIORDLANDMILFORD SOUND, NATIONAL For over 60 years we’ve ensured visitors to this incredible part of the world receive The journey so far.. -

Southland Trail Notes Contents
22 October 2020 Southland trail notes Contents • Mararoa River Track • Tākitimu Track • Birchwood to Merrivale • Longwood Forest Track • Long Hilly Track • Tīhaka Beach Track • Oreti Beach Track • Invercargill to Bluff Mararoa River Track Route Trampers continuing on from the Mavora Walkway can walk south down and around the North Mavora Lake shore to the swingbridge across the Mararoa River at the lake’s outlet. From here the track is marked and sign-posted. It stays west of but proximate to the Mararoa River and then South Mavora Lake to this lake’s outlet where another swingbridge provides an alternative access point from Mavora Lakes Road. Beyond this swingbridge, the track continues down the true right side of the Mararoa River to a third and final swing bridge. Along the way a careful assessment is required: if the Mararoa River can be forded safely then Te Araroa Trampers can continue down the track on the true right side to the Kiwi Burn then either divert 1.5km to the Kiwi Burn Hut, or ford the Mararoa River and continue south on the true left bank. If the Mararoa is not fordable then Te Araroa trampers must cross the final swingbridge. Trampers can then continue down the true left bank on the riverside of the fence and, after 3km, rejoin the Te Araroa opposite the Kiwi Burn confluence. 1 Below the Kiwi Burn confluence, Te Araroa is marked with poles down the Mararoa’s true left bank. This is on the riverside of the fence all the way down to Wash Creek, some 16km distant. -
Fiordland Day Walks Te Wāhipounamu – South West New Zealand World Heritage Area
FIORDLAND SOUTHLAND Fiordland Day Walks Te Wāhipounamu – South West New Zealand World Heritage Area South West New Zealand is one of the great wilderness areas of the Southern Hemisphere. Known to Māori as Te Wāhipounamu (the place of greenstone), the South West New Zealand World Heritage Area incorporates Aoraki/Mount Cook, Westland Tai Poutini, Fiordland and Mount Aspiring national parks, covering 2.6 million hectares. World Heritage is a global concept that identifies natural and cultural sites of world significance, places so special that protecting them is of concern for all people. Some of the best examples of animals and plants once found on the ancient supercontinent Gondwana live in the World Heritage Area. Left: Lake Marian in Fiordland National Park. Photo: Henryk Welle Contents Fiordland National Park 3 Be prepared 4 History 5 Weather 6 Natural history 6 Formation ������������������������������������������������������� 7 Fiordland’s special birds 8 Marine life 10 Dogs and other pets 10 Te Rua-o-te-moko/Fiordland National Park Visitor Centre 11 Avalanches 11 Walks from the Milford Road Highway ����������������������������� 13 Walking tracks around Te Anau ����������� 21 Punanga Manu o Te Anau/ Te Anau Bird Sanctuary 28 Walks around Manapouri 31 Walking tracks around Monowai Lake, Borland and the Grebe valley ��������������� 37 Walking tracks around Lake Hauroko and the south coast 41 What else can I do in Fiordland National Park? 44 Contact us 46 ¯ Mi lfor d P S iop ound iota hi / )" Milford k r a ¯ P Mi lfor -

Agenda of Fiordland Community Board
Notice is hereby given that a Meeting of the Fiordland Community Board will be held on: Date: Tuesday, 13 April 2021 Time: 2pm Meeting Room: Community Room, Fiordland Health Centre Venue: 25 Luxmore Drive Te Anau Fiordland Community Board Agenda OPEN MEMBERSHIP Chairperson Sarah Greaney Deputy Chairperson Diane Holmes Members Mary Chartres Benjamin Killeen Ryan Murray Max Slee Councillor Ebel Kremer IN ATTENDANCE Committee Advisor Alyson Hamilton Community Liaison Officer Megan Seator Contact Telephone: 0800 732 732 Postal Address: PO Box 903, Invercargill 9840 Email: [email protected] Website: www.southlanddc.govt.nz www.southlanddc.govt.nz Note: The reports contained within this agenda are for consideration and should not be construed as Council policy unless and until adopted. Should Members require further information relating to any reports, please contact the relevant manager, Chairperson or Deputy Chairperson. Terms of Reference Community Boards TYPE OF COMMITTEE Community board RESPONSIBLE TO Council Each community board will have a relationship with the committees in section 8.4.2 to 8.4.5 of the delegations manual based on the scope of the activities/functions delegated to each committee. SUBCOMMITTEES As noted in section 8.5 of the delegations manual various subcommittees will report to specific community boards. LEGISLATIVE BASIS Resolution made by Council through the representation arrangements as per the Local Electoral Act 2001. Role, status and membership as per subpart 2 of Part 4 of the Local Government Act 2002 (LGA). Treaty of Waitangi as per section 4, Part 1 of the LGA. Opportunities for Maori to contribute to decision-making processes as per section 14 of Part 2 of the LGA. -

The Climate and Weather of Southland
THE CLIMATE AND WEATHER OF SOUTHLAND 2nd edition G.R. Macara © 2013. All rights reserved. The copyright for this report, and for the data, maps, figures and other information (hereafter collectively referred to as “data”) contained in it, is held by NIWA. This copyright extends to all forms of copying and any storage of material in any kind of information retrieval system. While NIWA uses all reasonable endeavours to ensure the accuracy of the data, NIWA does not guarantee or make any representation or warranty (express or implied) regarding the accuracy or completeness of the data, the use to which the data may be put or the results to be obtained from the use of the data. Accordingly, NIWA expressly disclaims all legal liability whatsoever arising from, or connected to, the use of, reference to, reliance on or possession of the data or the existence of errors therein. NIWA recommends that users exercise their own skill and care with respect to their use of the data and that they obtain independent professional advice relevant to their particular circumstances. NIWA SCIENCE AND TECHNOLOGY SERIES NUMBER 63 ISSN 1173-0382 Note to Second Edition This publication replaces the first edition of New Zealand Meteorological Service Miscellaneous Publication 115 (15), written in 1984 by J. Sansom. It was considered necessary to update the first edition, incorporating more recent data and updated methods of climatological variable calculation. THE CLIMATE AND WEATHER OF SOUTHLAND 2nd edition G. R. Macara CONTENTS SUMMARY 6 INTRODUCTION 7 TYPICAL