203629Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent N0.: US 8,343,962 B2 Kisak Et Al
US008343962B2 (12) United States Patent (10) Patent N0.: US 8,343,962 B2 Kisak et al. (45) Date of Patent: *Jan. 1, 2013 (54) TOPICAL FORMULATION (58) Field of Classi?cation Search ............. .. 514/226.5, 514/334, 420, 557, 567 (75) Inventors: Edward T. Kisak, San Diego, CA (US); See application ?le fOr Complete Search history. John M. NeWsam, La Jolla, CA (US); _ Dominic King-Smith, San Diego, CA (56) References C‘ted (US); Pankaj Karande, Troy, NY (US); Samir Mitragotri, Goleta, CA (US) US' PATENT DOCUMENTS 5,602,183 A 2/1997 Martin et al. (73) Assignee: NuvoResearchOntano (CA) Inc., Mississagua, 6,328,979 2B1 12/2001 Yamashita et a1. 7,001,592 B1 2/2006 Traynor et a1. ( * ) Notice: Subject to any disclaimer, the term of this 7,795,309 B2 9/2010 Kisak eta1~ patent is extended or adjusted under 35 2002/0064524 A1 5/2002 Cevc U.S.C. 154(b) by 212 days. FOREIGN PATENT DOCUMENTS This patent is subject to a terminal dis- W0 WO 2005/009510 2/2005 claimer- OTHER PUBLICATIONS (21) APPI' NO‘, 12/848,792 International Search Report issued on Aug. 8, 2008 in application No. PCT/lB2007/0l983 (corresponding to US 7,795,309). _ Notice ofAlloWance issued on Apr. 29, 2010 by the Examiner in US. (22) Med Aug- 2’ 2010 Appl. No. 12/281,561 (US 7,795,309). _ _ _ Of?ce Action issued on Dec. 30, 2009 by the Examiner in US. Appl. (65) Prior Publication Data No, 12/281,561 (Us 7,795,309), Us 2011/0028460 A1 Feb‘ 3’ 2011 Primary Examiner * Raymond Henley, 111 Related U 5 Application Data (74) Attorney, Agent, or Firm * Foley & Lardner LLP (63) Continuation-in-part of application No. -

Comparative Study of Different Doses of Rocuronium Bromide For
MedDocs Publishers Annals of Anesthesia and Pain Medicine Open Access | Research Article Comparative study of different doses of rocuronium bromide for endotracheal intubation Nidhi V Sardhara1*; Sonal A Shah2; Dhaval P Pipaliya3; Shivansh Gupta3 1SVP hospital, 13th floor, Room no 13125, Near Ellis bridge, Ahmedabad, Gujarat-380006 2Assistant Professor, Department of anesthesia, Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India 3First year Resident, Department of anesthesia, Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India *Corresponding Author(s): Nidhi V Sardhara Abstract SVP hospital, 13th floor, Room no 13125, Near Ellis Background: Endotracheal intubation is one of such bridge, Ahmedabad, Gujarat-380006 development without which general anesthesia cannot be Tel: +91-9428-44-7878, Fax: 7926-57-8452 considered safe for any major surgery particularly head and Email: [email protected] neck, thoracic and abdominal surgeries. Ever since the ad- vent of anesthesia, anesthesiologists have been in search of an ideal muscle relaxants which can provide ideal intu- bating conditions in ultrashort duration with minimal side effects. Rocuronium bromide provides fast onset of action, Received: Mar 11, 2020 an intermediate duration of action and rapid recovery, good Accepted: Apr 24, 2020 to excellent intubating conditions at doses having minimal Published Online: Apr 30, 2020 or no haemodynamic changes. Present study is to compare the effect of different doses (0.6 mg/kg, 0.9 mg/kg, 1.2 mg/ Journal: Annals of Anesthesia and Pain Medicine kg) of Rocuronium bromide for endotracheal intubation at Publisher: MedDocs Publishers LLC 60 seconds. Online edition: http://meddocsonline.org/ Material and methods: This study was carried out by Copyright: © Sardhara NV (2020). -

12-6202 Document: 01018895054 Date Filed: 08/10/2012 Page: 1 FILED United States Court of Appeals UNITED STATES COURT of APPEALS Tenth Circuit
Appellate Case: 12-6202 Document: 01018895054 Date Filed: 08/10/2012 Page: 1 FILED United States Court of Appeals UNITED STATES COURT OF APPEALS Tenth Circuit FOR THE TENTH CIRCUIT August 10, 2012 Elisabeth A. Shumaker Clerk of Court MICHAEL EDWARD HOOPER, Plaintiff-Appellant, v. No. 12-6202 (D.C. No. 5:12-cv-00758-M) JUSTIN JONES, Director DOC; (W.D. Okla.) RANDALL G. WORKMAN, Warden; DOES, Unknown Executioners, Defendants-Appellees. ORDER AND JUDGMENT* Before MURPHY, O’BRIEN, and HOLMES, Circuit Judges. Michael Edward Hooper, an Oklahoma state prisoner scheduled for execution by lethal injection on August 14, 2012, appeals from the district court’s order * After examining the briefs and appellate record, this panel has determined unanimously that oral argument would not materially assist the determination of this appeal. See Fed. R. App. P. 34(a)(2); 10th Cir. R. 34.1(G). The case is therefore ordered submitted without oral argument. This order and judgment is not binding precedent, except under the doctrines of law of the case, res judicata, and collateral estoppel. It may be cited, however, for its persuasive value consistent with Fed. R. App. P. 32.1 and 10th Cir. R. 32.1. Appellate Case: 12-6202 Document: 01018895054 Date Filed: 08/10/2012 Page: 2 denying his motion for a preliminary injunction seeking to stay his execution. Exercising jurisdiction under 28 U.S.C. § 1292(a)(1), we AFFIRM.1 I Mr. Hooper was tried and convicted on three counts of first-degree murder and sentenced to death. See Hooper v. State, 947 P.2d 1090 (Okla. -

Expression of Multiple Populations of Nicotinic Acetylcholine
EXPRESSION OF MULTIPLE POPULATIONS OF NICOTINIC ACETYLCHOLINE RECEPTORS IN BOVINE ADRENAL CHROMAFFIN CELLS DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in the Graduate School of The Ohio State University By Bryan W. Wenger, B.A. The Ohio State University 2003 Dissertation Committee: Approved by: Professor Dennis B. McKay, Advisor Professor R. Thomas Boyd ________________________ Advisor Professor Popat N. Patil College of Pharmacy Professor Lane Wallace, Ph.D. ABSTRACT The importance of the role of nAChRs in physiological and pathological states is becoming increasingly clear. It is apparent that there are multitudes of nAChR subtypes with different expression patterns, pharmacologies and functions that may be important in various disease states. Therefore, a greater understanding of nAChR subtypes is essential for potential pharmacological intervention in nAChR systems. Bovine adrenal chromaffin cells are a primary culture of a neuronal type cell that express ganglionic types of nAChRs whose activation can be related to a functional response. While much is known about the outcome of functional activation of adrenal nAChRs, little work has been done in characterizing populations of nAChRs in adrenal chromaffin cells. These studies characterize the pharmacology and regulation of populations of nAChRs found in bovine adrenal chromaffin cells. The primary findings of this research include 1) the characterization of an irreversible antagonist of adrenal nAChRs, 2) the discovery of -

Muscle Relaxants Physiologic and Pharmacologic Aspects
K. Fukushima • R. Ochiai (Eds.) Muscle Relaxants Physiologic and Pharmacologic Aspects With 125 Figures Springer Contents Preface V List of Contributors XVII 1. History of Muscle Relaxants Some Early Approaches to Relaxation in the United Kingdom J.P. Payne 3 The Final Steps Leading to the Anesthetic Use of Muscle Relaxants F.F. Foldes 8 History of Muscle Relaxants in Japan K. Iwatsuki 13 2. The Neuromuscular Junctions - Update Mechanisms of Action of Reversal Agents W.C. Bowman 19 Nicotinic Receptors F.G. Standaert 31 The Neuromuscular Junction—Basic Receptor Pharmacology J.A. Jeevendra Martyn 37 Muscle Contraction and Calcium Ion M. Endo 48 3. Current Basic Experimental Works Related to Neuromuscular Blockade in Present and Future Prejunctional Actions of Neuromuscular Blocking Drugs I.G. Marshall, C. Prior, J. Dempster, and L. Tian 51 VII VIII Approaches to Short-Acting Neuromuscular Blocking Agents J.B. Stenlake 62 Effects Other than Relaxation of Non-Depolarizing Muscle Relaxants E.S. Vizi 67 Regulation of Innervation-Related Properties of Cultured Skeletal Muscle Cells by Transmitter and Co-Transmitters R.H. Henning 82 4. Current Clinical Experimental Works Related to Neuromuscular Blockade in Present and Future Where Should Experimental Works Be Conducted? R.D. Miller 93 Muscle Relaxants in the Intensive Care Unit ! J.E. Caldwell 95 New Relaxants in the Operating Room R.K. Mirakhur 105 Kinetic-Dynamic Modelling of Neuromuscular Blockade C. Shanks Ill 5. Basic Aspects of Neuromuscular Junction Physiology of the Neuromuscular Junction W.C. Bowman 117 Properties of <x7-Containing Acetylcholine Receptors and Their Expression in Both Neurons and Muscle D.K. -

Quantitative Analysis of the Aminosteroidal Muscle Relaxant
J. Ecophysiol. Occup. Hlth. 3 & 4 (2013) 29-37 ® 2013 The Academy of Environmental Biology, India Quantitative Analysis of the Aminosteroidal Muscle Relaxant Vecuronium in Rat Liver and Kidneys using Ion-pairing and Liquid Chromatography-Tandem Mass Spectrometry Risha Jasmine Nathan*, P. Sharma, Lily Saroj Nathan1 Forensic Chemistry and Toxicology, Lok Nayak Jayaprakash Narayan National Institute of Criminology, New Delhi 1Ewing Christian College, University of Allahabad Abstract : Muscle relaxants are occasionally encountered in forensic toxicological cases for identification and quantitation. Due to unavailability of human samples, the analysis of the muscle relaxant vecuronium was done using post-mortem rat visceral samples. Rats were injected with bolus overdose of the drug and the post mortem samples were subject to ion-pair extraction with metanil yellow dye. Method for identification of the drug by LC-MS-MS was established first with secondary standard aqueous vecuronium solutions and then applied on the questioned samples. Quantitation was done to find the quantity of the drug in liver and kidney samples. Keywords : Aminosteroid, Muscle relaxant Vecuronium, Liquid Chromatography-Tandem Mass Spectrometry. Introduction ventilation is made available to the patient so as Muscle relaxants, better known as neuro- to maintain respiration as these drugs may also muscular-blocking drugs, are a class of drugs paralyze the diaphragm at the therapeutic dose that block neuromuscular transmission at required (Dripps, 1959). Despite taking neuromuscular junction which causes paralysis precautions, neuromuscular blocking drugs of the affected skeletal muscles. Of the two have been reported to have inadvertently classes, non-depolarizing neuromuscular caused deaths of patients by accident agents work without depolarizing the motor end (Newsletters, Nurse Advise, 2006). -

Product Monograph Vecuronium Bromide For
PRODUCT MONOGRAPH PrVECURONIUM BROMIDE FOR INJECTION Non-depolarizing Skeletal Neuromuscular Blocking Agent Pharmaceutical Partners of Canada Inc. Date of Preparation: 45 Vogell Road, Suite 200 January 15, 2008 Richmond Hill, ON L4B 3P6 Control No.: 119276 PRODUCT MONOGRAPH PrVECURONIUM BROMIDE FOR INJECTION Non-depolarizing Skeletal Neuromuscular Blocking Agent THIS DRUG SHOULD BE ADMINISTERED ONLY BY ADEQUATELY TRAINED INDIVIDUALS FAMILIAR WITH ITS ACTIONS, CHARACTERISTICS AND HAZARDS ACTIONS AND CLINICAL PHARMACOLOGY Vecuronium Bromide for Injection is a non-depolarizing neuromuscular blocking agent of intermediate duration possessing all of the characteristic pharmacological actions of this class of drugs (curariform). It acts by competing for cholinergic receptors at the motor end-plate. The antagonism to acetylcholine is inhibited and neuromuscular block reversed by acetylcholinesterase inhibitors such as neostigmine. Vecuronium Bromide for Injection is about 1/3 more potent than pancuronium; the duration of neuromuscular blockade produced by Vecuronium Bromide for Injection is shorter than that of pancuronium at initially equipotent doses. The time to onset of paralysis decreases and the duration of maximum effect increases with increasing Vecuronium Bromide for Injection doses. The use of a peripheral nerve stimulator is of benefit in assessing the degree of muscular relaxation. The ED90 (dose required to produce 90% suppression of the muscle twitch response with balanced anesthesia) has averaged 0.057 mg/kg (0.049 to 0.062 mg/kg in various studies). An initial Vecuronium Bromide for Injection dose of 0.08 to 0.10 mg/kg generally produces first depression of twitch in approximately 1 minute, good or excellent intubation conditions within 2.5 to 3 minutes, and maximum neuromuscular blockade within 3 to 5 minutes of injection in Vecuronium Bromide for Injection, Product Monograph Page 2 of 28 most patients. -

Factors That Affect the Onset of Action of Non-Depolarizing Neuromuscular
Review Article pISSN 2005-6419 • eISSN 2005-7563 KJA Factors that affect the onset Korean Journal of Anesthesiology of action of non-depolarizing neuromuscular blocking agents Yong Byum Kim1, Tae-Yun Sung2, and Hong Seuk Yang3 Department of Anesthesiology and Pain Medicine, 1Gil Medical Center, Gachon University College of Medicine, Incheon, 2Konyang University Hospital, Konyang University College of Medicine, Daejeon, 3Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea Neuromuscular blockade plays an important role in the safe management of patient airways, surgical field improvement, and respiratory care. Rapid-sequence induction of anesthesia is indispensable to emergency surgery and obstetric an- esthesia, and its purpose is to obtain a stable airway, adequate depth of anesthesia, and appropriate respiration within a short period of time without causing irritation or damage to the patient. There has been a continued search for new neu- romuscular blocking drugs (NMBDs) with a rapid onset of action. Factors that affect the onset time include the potency of the NMBDs, the rate of NMBDs reaching the effect site, the onset time by dose control, metabolism and elimination of NMBDs, buffered diffusion to the effect site, nicotinic acetylcholine receptor subunit affinity, drugs that affect acetylcho- line (ACh) production and release at the neuromuscular junction, drugs that inhibit plasma cholinesterase, presynaptic receptors responsible for ACh release at the neuromuscular junction, anesthetics or drugs that affect muscle contractil- ity, site and methods for monitoring neuromuscular function, individual variability, and coexisting disease. NMBDs with rapid onset without major adverse events are expected in the next few years, and the development of lower potency NMBDs will continue. -

Muscle Relaxants Femoral Arteriography.,,>
IN THIS ISSUE: , .:t.i ". Muscle Relaxants fI, \'.' \., Femoral ArteriographY.,,> University of Minnesota Medical Bulletin Editor ROBERT B. HOWARD, M.D. Associate Editors RAY M. AMBERG GILBERT S. CAMPBELL, M.D. ELLIS S. BENSON, MD. BYRON B. COCHRANE, M.D. E. B. BROWN, PhD. RICHARD T. SMITH, M.D. WESLEY W. SPINK, MD. University of Minnesota Medical School J. 1. MORRILL, President, University of Minnesota HAROLD S. DIEHL, MD., Dean, College of Medical SciencBs WILLIAM F. MALONEY, M.D., Assistant Dean N. 1. GAULT, JR., MD., Assistant Dean University Hospitals RAY M. AMBERG, Director Minnesota Medical Foundation WESLEY W. SPINK, M.D., President R. S. YLVISAKER, MD., Vice-President ROBERT B. HOWARD, M.D., Secretary-Treasurer Minnesota Medical Alumni Association BYRON B. COCHRANE, M.D., President VIRGIL J. P. LUNDQUIST, M.D., First Vice-President SHELDON M. LAGAARD, MD., Second Vice-President LEONARD A. BOROWICZ, M.D., Secretary JAMES C. MANKEY, M.D., Treasurer UNIVERSITY OF MINNESOTA Medical Bulletin OFFICIAL PUBLICATION OF THE UNIVERSITY OF MINNESOTA HOSPITALS, MINNE· SOTA MEDICAL FOUNDATION, AND MINNESOTA MEDICAL ALUMNI ASSOCIATION VOLUME XXVIII December 1, 1956 NUMBER 4 CONTENTS STAFF MEETING REPORTS Current Status of Muscle Relaxants BY J. Albert Jackson, MD., J. H. Matthews, M.D., J. J. Buckley, M.D., D.S.P. Weatherhead, M.D., AND F. H. Van Bergen, M.D. 114 Small Vessel Changes in Femoral Arteriography BY Alexander R. Margulis, M.D. AND T. O. Murphy, MD.__ 123 EDITORIALS .. - -. - ---__ __ _ 132 MEDICAL SCHOOL ACTIVITIES ----------- 133 POSTGRADUATE EDUCATION - 135 COMING EVENTS 136 PIIb1ished semi.monthly from October 15 to JUDe 15 at Minneapolis, Minnesota. -

Vecuronium Bromide As Control
A COMPARATIVE STUDY TO FIND AN IDEAL INTUBATING DOSE OF INJ. ROCURONIUM BROMIDE USING INJ. VECURONIUM BROMIDE AS CONTROL. Dissertation submitted In partial fulfillment for the award of M.D DEGREE EXAMINATION M.D. ANAESTHESIOLOGY & CRITICAL CARE BRANCH X GOVT KILPAUK MEDICAL COLLEGE AND HOSPITAL SUBMITTED TO THE TAMILNADU DR. MGR MEDICAL UNIVERSITY CHENNAI APRIL – 2011 1 DECLARATION I, Dr. D.Shunmuga Priya, solemnly declare that the dissertation, “A COMPARATIVE STUDY TO FIND AN IDEAL INTUBATING DOSE OF INJ. ROCURONIUM BROMIDE USING INJ. VECURONIUM BROMIDE AS CONTROL” is a bonafide work done by me in the Department of Anaesthesiology and Critical Care, Government Kilpauk, Medical College, Chennai under the able guidance of Prof. Dr. P.S. Shanmugam, MD., DA., Professor and HOD, Department of Anaesthesiology and Critical Care, Government Kilpauk Medical College, Chennai. Place : Chennai Date : (Dr. D.SHUNMUGA PRIYA) 5 CERTIFICATE This is to certify that this dissertation titled “A COMPARATIVE STUDY TO FIND AN IDEAL INTUBATING DOSE OF INJ. ROCURONIUM BROMIDE USING INJ. VECURONIUM BROMIDE AS CONTROL” has been prepared by Dr. D.SHUNMUGA PRIYA under my supervision in the Department of Anaesthesiology and Critical Care, Government Kilpauk Medical College, Chennai during the academic period 2008-2011 and is being submitted to the Tamil Nadu Dr. M.G.R. Medical University, Chennai in partial fulfillment of the University regulation for the award of the Degree of Doctor of Medicine (MD Anaesthesiology and Critical Care) and her dissertation is a bonafide work. Prof..Dr. V.Kanagasabai, M.D Prof. Dr. P.S.Shanmugam, M.D., D.A. DEAN Professor & HOD, Government Kilpauk Medical College Department of Anaesthesiology and & Hospital, Critical Care, Chennai. -

Pharmacological Studies on Pupillary Reflex Dilatation
PHARMACOLOGICAL STUDIES ON PUPILLARY REFLEX DILATATION SHINJI OONO Departmentof Pharmacology,Faculty of Medicine,Kyushu University, Fukuoka Received for publication September 20, 1964 Concerning the role of sympathetic and parasympathetic mechanisms in reflex dilatation of the pupil elicited by painful stimuli, there have long been many argu ments. One group of authors, for example, Bechterew (1) and Braunstein (2) concluded that the pupillary dilatation resulting from painful stimuli was caused solely by inhibi tion of the third cranial nerve activity. Another group of investigators, for example, Lieben and Kahn (3), Bain, Irving and McSwiney (4), Ury and Gellhorn (5), Ury and Oldberg (6) and Seybold and Moore (7) were of the opinion that parasympathetic in hibition was the principal factor in the reflex dilatation while sympathetic excitation was a negligible one. On the contrary, others, for instance, Luchsinger (8), Anderson (9), and Dechaume (10) claimed that sympathetic excitation was responsible for the pupillary reaction which was absent after cervical sympathectomy. Weinstein and Bender (11) compared the pupillary reflex activity in cats and mon keys. They concluded that a species-difference exists: in both species pupillary dilata tion is accomplished by both parasympathetic inhibitory and sympathetic excitatory mechanism. In the cat, inhibition of the parasympathetic mechanism is predominant while in the monkey excitation of the sympathetic mechanism is of greater importance . Later Lowenstein and Loewenfeld (12) performed more detailed experiments in cats using their own pupillographic instrument; they observed that pupillary reflex dilata tion was mostly due to sympathetic excitation, and was reduced to less than one-fifth of the normal control dilatation after sympathectomy. -
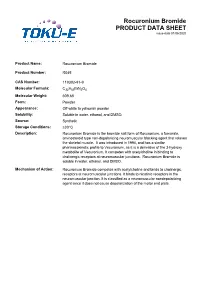
Rocuronium Bromide PRODUCT DATA SHEET Issue Date 01/06/2020
Rocuronium Bromide PRODUCT DATA SHEET issue date 01/06/2020 Product Name: Rocuronium Bromide Product Number: R045 CAS Number: 119302-91-9 Molecular Formula: C32H53BrN2O4 Molecular Weight: 609.68 Form: Powder Appearance: Off-white to yellowish powder Solubility: Soluble in water, ethanol, and DMSO. Source: Synthetic Storage Conditions: ≤30°C Description: Rocuronium Bromide is the bromide salt form of Rocuronium, a fumarate, aminosteroid type non-depolarizing neuromuscular blocking agent that relaxes the skeletal muscle. It was introduced in 1994, and has a similar pharmacokinetic profile to Vecuronium, as it is a derivative of the 3-hydroxy metabolite of Vecuronium. It competes with acetylcholine in binding to cholinergic receptors at neuromuscular junctions. Rocuronium Bromide is soluble in water, ethanol, and DMSO. Mechanism of Action: Rocuronium Bromide competes with acetylcholine and binds to cholinergic receptors at neuromuscular junctions. It binds to nicotinic receptors in the neuromuscular junction. It is classified as a neuromuscular nondepolarizing agent since it does not cause depolarization of the motor end plate. References: Anzenbacherova et al (2015) Interaction of Rocuronium with human liver cytochromes P450. J. Pharmacol. Sci. 127(2):190-195 PMID 25727956 Cembala TM, Sherwin JD, Tidmarsh MD, Appadu BL and Lambert DG (1998) Interaction of neuromuscular blocking drugs with recombinant human m1-m5 muscarinic receptors expressed in Chinese hamster ovary cells. B. J. Pharmacol. 125(5):1088-1094 PMID 9846649 Koksal PM and Gürbüzel M(2015) Analysis of genotoxic activity of ketamine and Rocuronium Bromide using the somatic mutation and recombination test in Drosophila melanogaster. Environ Toxicol Pharmacol. 39(2):628-634 PMID 25682000 Sauer et al (2017) Rocuronium is more hepatotoxic than succinylcholine in vitro.