Commonwealth Medicine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2004 Annual Report July 1, 2003 to June 30, 2004 Massachusetts Department of Mental Health
2004 Annual Report July 1, 2003 to June 30, 2004 Massachusetts Department of Mental Health Mitt Romney Governor Ronald Preston Secretary Elizabeth Childs, M.D. Commissioner “Bloom” — a public art installation of 28,000 pots of flowers at the Massachusetts Mental Health Center in November 2003 by artist Anna Schuleit commemorating the hospital’s closing. Mission The mission of the Department of Mental Health is to improve the quality of life for adults with serious and persistent mental illness and children with serious mental illness or severe emotional disturbance. This is accomplished by ensuring access to an integrated network of effective and effi- cient and culturally competent mental health services that promote consumer rights, responsibili- ties, rehabilitation, and recovery. Guiding Principles Provide responsive, high quality, cost effective services Focus support on the most vulnerable citizens of the Commonwealth Design programs using current scientific research, evaluation studies, and program outcome data Promote opportunities for individuals with mental illness to participate in rehabilitation and recov- ery no matter how severe their symptoms or pervasive their illness Offer individuals appropriate choices among services tailored to meet their unique needs Value managers who engage their colleagues and staff in entrepreneurial, innovative leadership that will improve the system Value input from a wide public audience and recognize that community advocacy and advisory groups are an essential component of system planning -

Annual Report of the Massachusetts Commission on Mental Diseases Of
TH** •O0«-»iA Public Document No. 117 SECOND ANNUAL EEPOET Massachusetts Commission on Mental Diseases THE COMMONWEALTH OF MASSACHUSETTS Year ending November 30, 1917. BOSTON: WRIGHT & POTTER PRINTING CO., STATE PRINTERS, 32 DERNE street. 1918. Publication of this Document approved by the Supervisor of Administration. TABLE OF CONTENTS. * PAGE Members of the Commission and List of Officers, 5 Letter of Transmission to Governor and Council, 7 Duties of the Commission, ..... 9,10 Activities of the Commission, ..... 10-15 Review of the Year: — All Classes under Care, ..... 16,17 The Insane, ....... 17-23 The Feeble-minded, . 23,24 The Epileptic, ....... 24,25 Report of the Pathologist, ..... 25-54 Reports of Committees on Nursing Service, . 54-61 Out-patient Departments, ..... 61-71 Commitments for Observation and Temporary Care, 71-73 Stability of Service, ...... 74,75 Capacity for Patients, ..... 76-78 Institutions : — Public 79-127 Private, . 127-130 Unlicensed Homes, . 131 Family Care of the Insane, .... 131-134 The Commission: — Proceedings of, . 135 Plans and Specifications, ..... 135 Estimates of State Expenses for 1918: — The Commission, 135, 136 Maintenance Appropriations, 136-138 Special Appropriations, .... 139-142 Financial Statement of Commission, 143, 144 Support Department, ..... 145-148 Deportations, ....... 148, 149 Transfers, ....... 150 Financial Department, . 150 General Matters : — New Legislation, ...... 151-160 Nineteen-year Statement as to Special Appropriations, 160-162 Financial Statistics, ....... 163-201 General Statistics, ....... 203-265 Directors^ of Institutions, ...... 266-278 Index, ......... 279-286 Digitized by the Internet Archive in 2010 with funding from Boston Library Consortium IVIember Libraries http://www.archive.org/details/annualreportofma1917mass2 Members of the Massachusetts Commission on Mental Diseases. -

DMH Connections
DMH Connections A publication of the Massachusetts Department of Mental Health Office of Communications & Community Engagement December 2009 In This Issue It's Clear: Facilities Are Ready to Check Out the Department of Public Help Staff and Clients Implement Health Blog a Tobacco Free Culture Multicultural Corner: Faith, Spirituality and Natural Supports in Today December 7, Recovery 2009, DMH begins the EOHHS Tobacco Free New Research Center Supports Youth Campus Initiative. All Employment DMH hospitals and facilities located on state property Commissioner Leadholm and DMH are now smoke free inside Staff Serve Up Thanksgiving for and out. The DMH Tobacco Hundreds of DMH Clients Free Policy is designed to provide a safe and healthy environment and Music Thearpy: Opportunities in model healthy behaviors. Sound Treatment For smokers, this culture change may be a Assistant Commissioner Claritza difficult adjustment. EOHHS and DMH recognize Abreu Awarded for her Leadership in that both patients and clients will struggle with the Latino Community the transition. Each facility has composed a Tobacco Free Planning Committee and is Conferences and Events working towards implementation of ongoing It's Clear: Facilities Are Ready to supports for staff and clients as they adapt to Help Staff and Clients Implement a this new policy and make the transition to a smoke free campus. Tobacco Free Culture Congratulations to the DMH These supports include assignment of cultural Performance Recognition Award champions who participated in a series of Winners trainings. There has also been communication through letters, meetings, discussions, and Voter Registration is Available to All open forums with managers and their staff. -

Lloyd Franklin Price, MD
Curriculum Vitae Lloyd Franklin Price, M.D. Citizenship: United States Education: Boston University, Boston, Massachusetts B.A., Magna Cum Laude, June 1968 Boston University Medical School M.D., Cum Laude, June 1968 Honors: Scholastic Achievement Award: 1966, Boston University Medical School Malamud Prize in Psychiatry: 1968, Boston University Medical School American Medical Association: Physician Recognition Award for Continuing Education: 1971, 1974, 1979, 1982, 1985 Mental Health Recognition Award - Harvard Pilgrim Health Care: 1995 Honorary Societies: Phi Beta Kappa, Boston University, 1968 Alpha Omega Alpha, Boston University Medical School, 1968 Begg Honor Society, Boston University Medical School, 1968 Teaching: Clinical Fellow in Psychiatry, July 1968- June 1974, Harvard Medical School Clinical Assistant in Psychiatry, July 1974- July 1982, Harvard Medical School Clinical Instructor in Psychiatry, Harvard Medical School, 1982-present Licensure: Diplomate: National Board of Medical Examiners Diplomate: American Board of Psychiatry and Neurology: Psychiatry 1977 Child Psychiatry 1979 Forensic Psychiatry 1999: [Recertified in 2009] Massachusetts Medical License New Hampshire Medical License Hospital Affiliations: Assistant Attending Child Psychiatrist: McLean Hospital, Belmont, Mass., July 1974-June 1984 Assistant Attending Psychiatrist: McLean Hospital, Belmont, MA, July 1979- July 1981 Consultant in Child and Adolescent Psychiatry: Human Resource Institute, Brookline, Mass., July 1974- June 1986 Associate Attending Psychiatrist: -
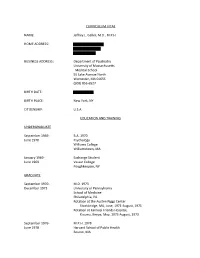
Jeffrey L. Geller, MD, MPH HOME ADDRESS
CURRICULUM VITAE NAME: Jeffrey L. Geller, M.D., M.P.H. HOME ADDRESS: BUSINESS ADDRESS: Department of Psychiatry University of Massachusetts Medical School 55 Lake Avenue North Worcester, MA 01655 (508) 856-6527 BIRTH DATE: BIRTH PLACE: New York, NY CITIZENSHIP: U.S.A. EDUCATION AND TRAINING UNDERGRADUATE September 1966- B.A. 1970 June 1970 Psychology Williams College Williamstown, MA January 1969- Exchange Student June 1969 Vassar College Poughkeepsie, NY GRADUATE September 1970- M.D. 1973 December 1973 University of Pennsylvania School of Medicine Philadelphia, PA Rotation at the Austen Riggs Center Stockbridge, MA, June, 1971-August, 1971 Rotation at Kaimosi Friends Hospital, Kisumu, Kenya, May, 1973-August, 1973 September 1976- M.P.H. 1978 June 1978 Harvard School of Public Health Boston, MA POST GRADUATE January 1974- Internship June 1974 Philadelphia General Hospital Philadelphia, PA July 1974- Psychiatric Residency June 1977 Beth Israel Hospital Boston, MA July 1977- N.I.M.H. Fellowship June 1978 Psychiatry in Primary Care Medicine Beth Israel Hospital Boston, MA APPOINTMENTS AND POSITIONS ACADEMIC APPOINTMENTS 1974-1978 Fellow Harvard Medical School Boston, MA 1979-1983 Assistant Professor University of Massachusetts Medical School Worcester, MA 1982-1984 Clinical Assistant Professor Smith School for Social Work Northampton, MA 1983-1984 Assistant Professor Harvard Medical School Cambridge, MA 1984, 1987, 1989 Adjunct Winter Study Faculty Williams College Williamstown, MA 1984-1986 Assistant Professor University of Pittsburgh, -

Wellness for All the Southcoast Health Plan Offers All Employees Resources to Live Healthier Lives
January 2 012 A not-for-profit, charitable organization. wellness fOR all The Southcoast Health Plan offers all employees resources to live healthier lives. s the new year rolls around, many of us pledge to do something to improve our health — get more a exercise, lose a few pounds, stop smoking, de-stress our lives, the list goes on. But sometimes it can be difficult to find the resources and support needed to turn these desires into realities. That is where the new Southcoast Health Plan comes in with even more wellness options — and all employees can use it. “The goal of the Southcoast Health Plan is to help create a not they purchase health insurance through Southcoast. culture of wellness throughout the organization,” said David “HealthQuest gives employees tools to help identify health DeJesus Jr., Senior Vice President of Human Resources. “Our aim risks and maintain or improve their health and well-being,” said is to help employees improve their health so they can be at their Kris Aimone, Wellness Coordinator. Offerings include: best both while at work and at home with their families.” • Free biometric health screenings. “Many employees think that the Southcoast Health Plan • HealthQuest Assessment. is health insurance and that only people who purchase their • Education classes. insurance through Southcoast are eligible to use its components,” • A personalized website. said Beth Barker, Director of Compensation & Benefits. “But health • Weight loss management programs. insurance is just a portion of what the Southcoast Health Plan • Quit smoking programs. offers. It also provides a wide variety of resources to all employees • Events and competitions. -
Annual Report of the Trustees of the Danvers State Hospital
Digitized by the Internet Archive in 2010 with funding from Boston Library Consortium Member Libraries http://www.archive.org/details/annualreportoftr1224danv Public Document No. 20 THIRTY-FIFTH ANNUAL REPORT THE TRUSTEES Danvers State Hospital, DANVERS, MASS. i (POST-OFFICE, HATHORNE), Year ending November 30, 1912. BOSTON: WRIGHT & POTTER PRINTING CO., STATE PRINTEES, 18 Post Office Square. 1913. Approved by The State Board of Publication. CONTENTS. PAGE Report of Trustees, 9 Report of Superintendent, 12 Report of Treasurer, 29 Statistics, 35 OFFICERS OF THE DANVERS STATE HOSPITAL. Nov. 30, 1912. TRUSTEES. Mr. Samuel Cole, Corresponding Secretary, . Beverly. Mr. Horace H. Atherton, ..... Saugus. Miss Mary Ward Nichols, Recording Secretary, . Danvers. Mr. S. Herbert Wilkins, Chairman, . Salem. Mr. Seward W. Jones, ...... Newton Highlands. Mr. Ernest B. Dane, ...... Boston. Miss Annie M. Kilham, Beverly. RESIDENT OFFICERS. George M. Kline, M.D., Physician and Superintendent. John B. Macdonald, M.D., Senior Assistant Physician. Wm. B. Cornell, M.D., Assistant Physician. Harlan L. Paine, M.D., . Assistant Physician. Anna H. Peabody, M.D., . Assistant Physician. Nelson G. Trtjeman, M.D., . Assistant Physician. Burton D. Thorpe, M.D., Assistant Physician. F. D. Streeter, M.D., . Assistant Physician. Mr. Edward S. Groves, Steward. NON-RESIDENT OFFICERS. Earl D. Bond, M.D., Assistant Physician and Pathologist. Mr. Scott Whitcher, Treasurer and Clerk. HEADS OF DEPARTMENTS. Mr. Adam D. Smith, Supervisor Male Department. Miss Eunice A. Fisk, Superintendent of Nurses and Prin- cipal of Training School. Mrs. Harriet A. Read, . Supervisor Female Department. Mr. Charles Lindgren, . Engineer. Mr. Junius C. Wing, Farmer. Mr. George W. Gardner, Carpenter. CONSULTING BOARD OF PHYSICIANS. -

1 There Is No “I” in “Follow
There is No “I” in “Follow Me” July 15, 2018 Northminster Presbyterian Church Rev. Michael D. Kirby Romans 12:1-8 and Luke 9:23-25 It took every one of them. On Saturday, July 23rd, the Wild Boars European football club had completed its practice session but weren’t expected back at the gates of the church that served as their sponsor for at least another hour. Ekapol, their quiet, reserved, 25-year-old coach, worked as a concierge at the church — the Buddhist Temple called Pharathat Doi Wao — a temple famous for being the first temple one reaches in Thailand after crossing the border from Myanmar, also known as Burma. For that reason, it’s home to many stateless people who escaped from oppression in Myanmar over the years, people who have no country and no passport. Ekapol is one of those people, studying Buddhist practices while he works at the Temple and volunteers as a soccer coach. We now know the boys and the coach intended to spend one hour in the famous caves until the flood waters from recent rains entered the caves from thousands of crevasses some miles away from the cave itself. For the next 10 days, the community worried and turned to visitors in their midst. The Thai Navy Seals were brave, but they didn’t know these caves. But British cave enthusiast Vern Unsworth did. He’d spent years making those caves his second home. He knew every nook and cranny. But he wasn’t experienced in cave diving rescue. However, he knew three friends who were — British divers and rescue specialists John Volanthen, Rick Stanton and Robert Harper. -

Of 379 Institutons Receiving a Questionnaire on Their Paramedical
DOCUMENT RESUME ED 022 442 JC 680 311 INVENTORY 1967: MASSACHUSETTS HEALTH MANPOWER TRAINING AT LESS THAN A BACCALAUREATE LEVEL. PART I. Training Center for Comprehensive Care, Jamaica Plain, Mass. Pula Date 67 Note-96p. EDRS Price MF-S0.50 HC-$3.92 Descriptors-*HEALTH OCCUPATIONS, *JUNIOR COLLEGES, *MANPOWER DEVELOPMENT, MEDICAL RECORD TECHNICIANS, fvEDICAL SERVICES, NURSES, NURSES AIDES, *PARAMEDICAL OCCUPATIONS, *SUBPROFESSIONALS, THERAPISTS, VOCATIONAL EDUCATION Identifiers *Massachusetts Of 379 institutonsreceiving a questionnaire on their paramedical training programs, 369 replied. They supplied data on 465 courses in 56 job categories. Those conducting the courses include hospitals, nursing homes, highschools, colleges, universities, technical schools, community service agencies, the State Department of Public Health, and an industrial plant. For each job category are given (1) a definition, (2) a detailed description of the curriculum, (3) the teaching staff, (4) a hst of the places offering the course, (5) the cost of the course, (6) in-training payment, if any, for taking the course, (7) length of time required for the course, and (8) ehgibility requirements for the trainee. (HH) U.S.melitillMMIN DEPARIMENTOFFICE OF HEALTH, OF EDUCATION EDUCATION &WELFARE THIS DOCUMENT HAS BEEN REPRODUCEDEXACTLY AS RECEIVED FROM THE PERSONPOSITIONSTATEDMASSACHUSETTS DO OR OR NOT ORGANIZATION POLICY. NECESSARILY ORIGINATING REPRESENT IT.OFFICIALPOINTS OFFICE OF VIEW OF EDUCATION OR OPINIONS ATHEALTH LESS THANMANPOWERAINVENTORY BACCALAUREATETRAITLEVEL ING fteb 1967 Training Center170 Mortonfor Comprehensive Street Care i Jamaica PARTPlain, ONEMass. 02130 1 MASSACHUSETTS IHEALTH N V E N T O RMANPOWER Y 19 6 7 TRAINING 1 AT LESS THAN ACONTENTS BACCALAUREATELEVEL IntroductionSponsorship of the survey Pages1-2 TheMethodDefinition Situation used ofin trainingconducting the survey 3-5 Location.JobNumberrequirements. -

Hospital Charges Effective July 1, 1960
o ~ CLD . L1/!. '-1'/.. #._ J,...C!/ r!J(jm'NIA.mY1Meaal~ cr ~ ~ @~¥J~~ WHEN REPLYING PLEASE QUOTE LA.B. FILE NO. ATTENTION OF: June 29, 1960 CIRCULAR LETTER NO. 120 TO: ALL INSURANCE COMPANIES, ALL SELF-INSURERS, AND WORKMEN'S COMPENSATION AGENTS OF DEPARTMENTS OF THE COMMONWEALTH AND COUNTIES, CITIES, TOWNS AND DISTRICTS SUBJECT TO THE WORKMEN'S COMPENSA"; TION LAW (GENERAL LAWS, CHAPTER 152, AS AMENDED) IN RE: CHARGES OF HO SPITALS FOR SERVICES UNDER THE WORKMEN'S COMPENSATION ACT. Enclosed herewith is a list of hospitals, together with their respective per diem rates as approved by the Industrial Accident Board with relation to their charges for the above-captioned services. These rates are effective as of' July 1, 1960, and shall continue in effect until July 1, 1961. For cases requiring continuous hospitalization in excess of thirty days, the payments to the hospital for in-patient care rendered after the thirtieth day shall be in accordance with the above mentioned per diem rates, or at the hospital's regular charges for like services to the general public, whichever in the aggregate is the lower. Very truly yours, ~~~ MICHAEL DE MARCO CHAIRMAN JEC/ec DIVISION OF INDUSTRIAL ACCIDENTS 150 TREMONT STREET BO STON 11, MASS. ALL-INCLUSIVE PER DIEM RATES EFFECTIVE JULY 1, 1960 Per Diem Hospital Location Rate Addison Gilbert Hosp. Gloucester. $26.69 Allerton Hosp. Brookline NOW BROOKLINE HOSPITAL Amesbury Hosp. Amesbury 23.43 Anna Jaques Hosp. Newburyport 26.23 Athol Memorial Hosp. Athol 25.50 Baker Memorial Hosp. Boston 37.53 (Mass. General) Barnstable County San. -

Ballot Paper
CAVE DIVERS ASSOCIATION OF AUSTRALIA INCORPORATED IN SOUTH AUSTRALIA 40TH ANNIVERSARY CELEBRATING 40 YEARS IN 2013 AGM and Symposium 2013 This year marks the 40th anniversary of the Cave Divers Association of Australia (CDAA). To celebrate, we are holding an exciting two day event on the 9th and 10th of November in conjunction with this year’s Annual General Meeting (AGM). There will be a number of talks, demonstrations and displays, at which we will also be inviting public participation. Speakers will include notable Australian and international cave divers. We are also planning on inviting various dignitaries including representatives from local and state government, private land owners and the local media. The venue, the Main Corner, is conveniently located in the centre of town at 1 Bay Road, Mount Gambier. The Symposium will be held in the Dress Circle commencing at 9:00am. The AGM will follow at 6:00pm and dinner will be served in City Hall at 7:30pm. We hope that you can join us to celebrate 40 years of CDAA history. 2013 SYMPOSIUM AGENDA & GUEST SPEAKERS PAGE 1 ~ GUEST SPEAKER BIO’S ~ Peter Horne & Ian Lewis Peter Horne & Ian Lewis are two of the CDAA’s longest serving members and their contributions to the Association are themselves “historic”. Both have acted in official capacity as Office Bearers, both have been amongst the first to find, explore and map a multitude of sites and both have had to work hard to ensure that the CDAA has continued access to many sites that it retains today. Peter “Puddles” Horne became interested in Mount Gambier's underground realm in 1976 after a workmate introduced him to Ewen's Ponds. -
Annual Report of the Department of Public Welfare
Public Document No. 17 ANNUAL REPORT OF THE DEPARTMENT OF Public Welfare FOR THE Year ending November 30, 1927 Publication of this Document approved by the Commi88ion on Admimhi 2M. 5-'28. Order 2207. T^-,' u m J f Cfte Commontoealrt) of illas(£facf)UfiJett£^. I DEPARTMENT OF PUBLIC WELFARE. To the Honorable Senate and House of Representaiives: The Eighth Annual Report of the Department of PubUc Welfare, covering the year from December 1, 1926, to November 30, 1927, is herewith respectfully ! presented. RICHARD K. COXAXT, Commissioner of Public Welfare. 37 State House, Boston. Present Members of the Advisory Board of the Department of Public Welfare. Date of Original Appointment Name Residence Term Expires December 10, 1919 A. C. Ratshesky .... Boston . December 10, 1928 December 10, 1919 Jeffrey R. Brackett .... Boston . December 10. 1928 December 10, 1919 George Crompton .... Worcester . December 10, 1930 December 10, 1919 George H. McClean . Springfield . December 10, 1930 December 10, 1919 Mrs. Ada Eliot Sheffield . Cambridge . December 10, 1929 December 10, 1919 Mrs. Mary P. H. Sherburne . Brookline . December 10, 1929 Divisions of the Department of Public Welfare. Division of Aid and Relief: Frank W. Goodhue, Director. Miss Flora E. Burton, Supervisor of Social Service, Mrs. Elizabeth F. Moloney, Supervisor of Mothers' Aid. Edward F. Morgan, Supervisor of Settlements. Division of Child Guardianship: Miss Winifred A. Keneran, Director. Division of Juvenile Training: Charles M. Davenport, Director. Robert J. Watson, Executive Secretary. Miss Almeda F. Cree, Superintendent, Girls' Parole Branch. John J. Smith, Superintendent, Boys' Parole Branch. Subdivision of Private Incorporated Charities: Miss Caroline J. Cook, Supervisor of Incorporated Charities.