Weston State Hospital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The American Midwest Haunting: the Asylum Lives on Adam Ladner, Ball State University
Digital Literature Review1 113 The American Midwest Haunting: The Asylum Lives On Adam Ladner, Ball State University Ghost stories, while seeming unique This paper explores the similarities and and individual to many cities, towns, and differences of Midwestern American small states, often fit into a practiced formula town ghost stories, as well as the haunt- and outline that isn’t always apparent. ed asylums of the Midwest and their own ghost stories. The essay explores asylum In the Midwestern region of the United histories and shows what makes up the States, there are countless stories of wom- American Midwest cultural haunting and en in white, hitchhikers who disappear why those fears are pushed onto asylums halfway through the car ride, wailing and and their ghosts. screaming coming from woods and aban- doned sites, figures wandering lighthous- es and the lakeshores, and haunted houses at the ends of streets—just to name a few. Stories like these all have common themes and structures, the most prominent being the idea and painful realization of a permanent and unbreakable isolation. Upon closer examination, these stories show that women in white are always left to wander the area where they died alone, hitchhikers never reach their destination and often vanish half- way through the car ride, and ghostly lighthouse keepers stay locked in their lighthouses. Unbreakable isolation is common theme scattered in many American Midwestern ghost stories, but its origin lies in the residual hauntings of the reformatories and asylums scat- tered throughout the solitary and empty midlands of America. The haunted insane asylum is a prevalent story in the American Midwest. -

2004 Annual Report July 1, 2003 to June 30, 2004 Massachusetts Department of Mental Health
2004 Annual Report July 1, 2003 to June 30, 2004 Massachusetts Department of Mental Health Mitt Romney Governor Ronald Preston Secretary Elizabeth Childs, M.D. Commissioner “Bloom” — a public art installation of 28,000 pots of flowers at the Massachusetts Mental Health Center in November 2003 by artist Anna Schuleit commemorating the hospital’s closing. Mission The mission of the Department of Mental Health is to improve the quality of life for adults with serious and persistent mental illness and children with serious mental illness or severe emotional disturbance. This is accomplished by ensuring access to an integrated network of effective and effi- cient and culturally competent mental health services that promote consumer rights, responsibili- ties, rehabilitation, and recovery. Guiding Principles Provide responsive, high quality, cost effective services Focus support on the most vulnerable citizens of the Commonwealth Design programs using current scientific research, evaluation studies, and program outcome data Promote opportunities for individuals with mental illness to participate in rehabilitation and recov- ery no matter how severe their symptoms or pervasive their illness Offer individuals appropriate choices among services tailored to meet their unique needs Value managers who engage their colleagues and staff in entrepreneurial, innovative leadership that will improve the system Value input from a wide public audience and recognize that community advocacy and advisory groups are an essential component of system planning -

Annual Report of the Massachusetts Commission on Mental Diseases Of
TH** •O0«-»iA Public Document No. 117 SECOND ANNUAL EEPOET Massachusetts Commission on Mental Diseases THE COMMONWEALTH OF MASSACHUSETTS Year ending November 30, 1917. BOSTON: WRIGHT & POTTER PRINTING CO., STATE PRINTERS, 32 DERNE street. 1918. Publication of this Document approved by the Supervisor of Administration. TABLE OF CONTENTS. * PAGE Members of the Commission and List of Officers, 5 Letter of Transmission to Governor and Council, 7 Duties of the Commission, ..... 9,10 Activities of the Commission, ..... 10-15 Review of the Year: — All Classes under Care, ..... 16,17 The Insane, ....... 17-23 The Feeble-minded, . 23,24 The Epileptic, ....... 24,25 Report of the Pathologist, ..... 25-54 Reports of Committees on Nursing Service, . 54-61 Out-patient Departments, ..... 61-71 Commitments for Observation and Temporary Care, 71-73 Stability of Service, ...... 74,75 Capacity for Patients, ..... 76-78 Institutions : — Public 79-127 Private, . 127-130 Unlicensed Homes, . 131 Family Care of the Insane, .... 131-134 The Commission: — Proceedings of, . 135 Plans and Specifications, ..... 135 Estimates of State Expenses for 1918: — The Commission, 135, 136 Maintenance Appropriations, 136-138 Special Appropriations, .... 139-142 Financial Statement of Commission, 143, 144 Support Department, ..... 145-148 Deportations, ....... 148, 149 Transfers, ....... 150 Financial Department, . 150 General Matters : — New Legislation, ...... 151-160 Nineteen-year Statement as to Special Appropriations, 160-162 Financial Statistics, ....... 163-201 General Statistics, ....... 203-265 Directors^ of Institutions, ...... 266-278 Index, ......... 279-286 Digitized by the Internet Archive in 2010 with funding from Boston Library Consortium IVIember Libraries http://www.archive.org/details/annualreportofma1917mass2 Members of the Massachusetts Commission on Mental Diseases. -
The Donegal District Lunatic Asylum
‘A WORLD APART’ – The Donegal District Lunatic Asylum Number of Registrar Name Where Chargable This exhibition curated by the Donegal County Museum and the Archives Service, Donegal County Council in association with the HSE was inspired by the ending of the provision of residential mental health services at the St. Conal’s Hospital site. The hospital has been an integral part of Letterkenny and County Donegal for 154 years. Often shrouded by mythology and stigma, the asylum fulfilled a necessary role in society but one that is currently undergoing radical change.This exhibition, by putting into context the earliest history of mental health services in Donegal hopes to raise public awareness of mental health. The exhibition is organised in conjunction with Little John Nee’s artist’s residency in An Grianan Theatre and his performance of “The Mental”. This project is supported by PEACE III Programme managed for the Special EU Programmes Body by Donegal County Council. Timeline This Timeline covers the period of the reforms in the mental health laws. 1745 - Dean Jonathan Swift: 1907 - Eugenics Education Society: On his death he left money for the building of Saint Patrick’s This Society was established to promote population control Hospital (opened 1757), the first in Ireland to measures on undesirable genetic traits, including mental treat mental health patients. defects. 1774 - An Act for Regulating Private Madhouses: 1908 Report by Royal Commission This act ruled that there should be inspections of asylums once on Care of Feeble-Minded a year at least, but unfortunately, this only covered London. 1913 Mental Deficiency Act: 1800 - Pressure for reform is growing: This Act established the Board of Control to replace the Lunacy This is sparked off by the terrible conditions in London’s Commission. -

DMH Connections
DMH Connections A publication of the Massachusetts Department of Mental Health Office of Communications & Community Engagement December 2009 In This Issue It's Clear: Facilities Are Ready to Check Out the Department of Public Help Staff and Clients Implement Health Blog a Tobacco Free Culture Multicultural Corner: Faith, Spirituality and Natural Supports in Today December 7, Recovery 2009, DMH begins the EOHHS Tobacco Free New Research Center Supports Youth Campus Initiative. All Employment DMH hospitals and facilities located on state property Commissioner Leadholm and DMH are now smoke free inside Staff Serve Up Thanksgiving for and out. The DMH Tobacco Hundreds of DMH Clients Free Policy is designed to provide a safe and healthy environment and Music Thearpy: Opportunities in model healthy behaviors. Sound Treatment For smokers, this culture change may be a Assistant Commissioner Claritza difficult adjustment. EOHHS and DMH recognize Abreu Awarded for her Leadership in that both patients and clients will struggle with the Latino Community the transition. Each facility has composed a Tobacco Free Planning Committee and is Conferences and Events working towards implementation of ongoing It's Clear: Facilities Are Ready to supports for staff and clients as they adapt to Help Staff and Clients Implement a this new policy and make the transition to a smoke free campus. Tobacco Free Culture Congratulations to the DMH These supports include assignment of cultural Performance Recognition Award champions who participated in a series of Winners trainings. There has also been communication through letters, meetings, discussions, and Voter Registration is Available to All open forums with managers and their staff. -

MASTER PLAN DOCUMENT.Indd
Master Plan for the RICHARDSON OLMSTED COMPLEX Buffalo, NY September 2009 9.29.09 Prepared For: THE RICHARDSON CENTER CORPORATION By: CHAN KRIEGER SIENIEWICZ CKS ARCHITECTURE AND URBAN DESIGN in collaboration with: Richardson Center Corporation (RCC) Richardson Architecture Center, Inc Reed Hilderbrand *Stanford Lipsey, Chairman Peter J. Atkinson - Capital Projects Manager, Landscape Architecture Publisher, The Buffalo News Harvard University Art Museums Watertown, MA *Howard Zemsky, Vice Chairman Anthony Bannon - Director, Urban Design Project President, Taurus Capital Partners, LLC. George Eastman House Public Process URBAN DESIGN PROJECT Buffalo, NY *Christopher Greene, Secretary Barbara A. Campagna, FAIA, LEED AP - Graham Gund Architect of the Partner, Damon & Morey, LLP National Trust for Historic Preservation City Visions/ City Properties Real Estate Development *Paul Hojnacki, Treasurer Brian Carter, Ex Offi cio - Dean and Professor, Louisville, KY President, Curtis Screw Company University at Buffalo School of Architecture and Planning Clarion Associates Carol Ash, Commissioner Louis Grachos - Director, Economic Modeling NYS Offi ce of Parks, Recreation, and Historic Preservation Albright-Knox Art Gallery Chicago, Il *Clinton Brown, President Robert Kresse – Attorney, Parsons Brinckerhoff Clinton Brown Co. Architecture, PC Hiscock & Barclay, LLP Permitting Buffalo, NY Paul Ciminelli, President & CEO Lynn J. Osmond - President and CEO, Ciminelli Development Company Chicago Architecture Foundation Bero Architecture Historic Preservation -

Lloyd Franklin Price, MD
Curriculum Vitae Lloyd Franklin Price, M.D. Citizenship: United States Education: Boston University, Boston, Massachusetts B.A., Magna Cum Laude, June 1968 Boston University Medical School M.D., Cum Laude, June 1968 Honors: Scholastic Achievement Award: 1966, Boston University Medical School Malamud Prize in Psychiatry: 1968, Boston University Medical School American Medical Association: Physician Recognition Award for Continuing Education: 1971, 1974, 1979, 1982, 1985 Mental Health Recognition Award - Harvard Pilgrim Health Care: 1995 Honorary Societies: Phi Beta Kappa, Boston University, 1968 Alpha Omega Alpha, Boston University Medical School, 1968 Begg Honor Society, Boston University Medical School, 1968 Teaching: Clinical Fellow in Psychiatry, July 1968- June 1974, Harvard Medical School Clinical Assistant in Psychiatry, July 1974- July 1982, Harvard Medical School Clinical Instructor in Psychiatry, Harvard Medical School, 1982-present Licensure: Diplomate: National Board of Medical Examiners Diplomate: American Board of Psychiatry and Neurology: Psychiatry 1977 Child Psychiatry 1979 Forensic Psychiatry 1999: [Recertified in 2009] Massachusetts Medical License New Hampshire Medical License Hospital Affiliations: Assistant Attending Child Psychiatrist: McLean Hospital, Belmont, Mass., July 1974-June 1984 Assistant Attending Psychiatrist: McLean Hospital, Belmont, MA, July 1979- July 1981 Consultant in Child and Adolescent Psychiatry: Human Resource Institute, Brookline, Mass., July 1974- June 1986 Associate Attending Psychiatrist: -
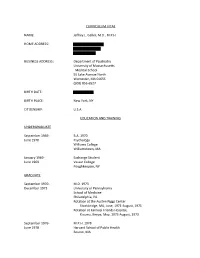
Jeffrey L. Geller, MD, MPH HOME ADDRESS
CURRICULUM VITAE NAME: Jeffrey L. Geller, M.D., M.P.H. HOME ADDRESS: BUSINESS ADDRESS: Department of Psychiatry University of Massachusetts Medical School 55 Lake Avenue North Worcester, MA 01655 (508) 856-6527 BIRTH DATE: BIRTH PLACE: New York, NY CITIZENSHIP: U.S.A. EDUCATION AND TRAINING UNDERGRADUATE September 1966- B.A. 1970 June 1970 Psychology Williams College Williamstown, MA January 1969- Exchange Student June 1969 Vassar College Poughkeepsie, NY GRADUATE September 1970- M.D. 1973 December 1973 University of Pennsylvania School of Medicine Philadelphia, PA Rotation at the Austen Riggs Center Stockbridge, MA, June, 1971-August, 1971 Rotation at Kaimosi Friends Hospital, Kisumu, Kenya, May, 1973-August, 1973 September 1976- M.P.H. 1978 June 1978 Harvard School of Public Health Boston, MA POST GRADUATE January 1974- Internship June 1974 Philadelphia General Hospital Philadelphia, PA July 1974- Psychiatric Residency June 1977 Beth Israel Hospital Boston, MA July 1977- N.I.M.H. Fellowship June 1978 Psychiatry in Primary Care Medicine Beth Israel Hospital Boston, MA APPOINTMENTS AND POSITIONS ACADEMIC APPOINTMENTS 1974-1978 Fellow Harvard Medical School Boston, MA 1979-1983 Assistant Professor University of Massachusetts Medical School Worcester, MA 1982-1984 Clinical Assistant Professor Smith School for Social Work Northampton, MA 1983-1984 Assistant Professor Harvard Medical School Cambridge, MA 1984, 1987, 1989 Adjunct Winter Study Faculty Williams College Williamstown, MA 1984-1986 Assistant Professor University of Pittsburgh, -

The Patients of the Bristol Lunatic Asylum in the Nineteenth Century 1861-1900
THE PATIENTS OF THE BRISTOL LUNATIC ASYLUM IN THE NINETEENTH CENTURY 1861-1900 PAUL TOBIA A thesis submitted in partial fulfilment of the requirements of the University of the West of England, Bristol for the degree of Doctor of Philosophy Faculty of Arts, Creative Industries and Education March 2017 Word Count 76,717 1 Abstract There is a wide and impressive historiography about the British lunatic asylums in the nineteenth century, the vast majority of which are concerned with their nature and significance. This study does not ignore such subjects but is primarily concerned with the patients of the Bristol Asylum. Who were they, what were their stories and how did they fare in the Asylum and how did that change over our period. It uses a distinct and varied methodology including a comprehensive database, compiled from the asylum records, of all the patients admitted in the nineteenth century. Using pivot tables to analyse the data we were able to produce reliable assessments of the range and nature of the patients admitted; dispelling some of the suggestions that they represented an underclass. We were also able to determine in what way the asylum changed and how the different medical superintendents altered the nature and ethos of the asylum. One of these results showed how the different superintendents had massively different diagnostic criteria. This effected the lives of the patients and illustrates the somewhat random nature of Victorian psychiatric diagnostics. The database was also the starting point for our research into the patients as individuals. Many aspects of life in the asylum can best be understood by looking at individual cases. -
Annual Report of the Trustees of the Danvers State Hospital
Digitized by the Internet Archive in 2010 with funding from Boston Library Consortium Member Libraries http://www.archive.org/details/annualreportoftr1224danv Public Document No. 20 THIRTY-FIFTH ANNUAL REPORT THE TRUSTEES Danvers State Hospital, DANVERS, MASS. i (POST-OFFICE, HATHORNE), Year ending November 30, 1912. BOSTON: WRIGHT & POTTER PRINTING CO., STATE PRINTEES, 18 Post Office Square. 1913. Approved by The State Board of Publication. CONTENTS. PAGE Report of Trustees, 9 Report of Superintendent, 12 Report of Treasurer, 29 Statistics, 35 OFFICERS OF THE DANVERS STATE HOSPITAL. Nov. 30, 1912. TRUSTEES. Mr. Samuel Cole, Corresponding Secretary, . Beverly. Mr. Horace H. Atherton, ..... Saugus. Miss Mary Ward Nichols, Recording Secretary, . Danvers. Mr. S. Herbert Wilkins, Chairman, . Salem. Mr. Seward W. Jones, ...... Newton Highlands. Mr. Ernest B. Dane, ...... Boston. Miss Annie M. Kilham, Beverly. RESIDENT OFFICERS. George M. Kline, M.D., Physician and Superintendent. John B. Macdonald, M.D., Senior Assistant Physician. Wm. B. Cornell, M.D., Assistant Physician. Harlan L. Paine, M.D., . Assistant Physician. Anna H. Peabody, M.D., . Assistant Physician. Nelson G. Trtjeman, M.D., . Assistant Physician. Burton D. Thorpe, M.D., Assistant Physician. F. D. Streeter, M.D., . Assistant Physician. Mr. Edward S. Groves, Steward. NON-RESIDENT OFFICERS. Earl D. Bond, M.D., Assistant Physician and Pathologist. Mr. Scott Whitcher, Treasurer and Clerk. HEADS OF DEPARTMENTS. Mr. Adam D. Smith, Supervisor Male Department. Miss Eunice A. Fisk, Superintendent of Nurses and Prin- cipal of Training School. Mrs. Harriet A. Read, . Supervisor Female Department. Mr. Charles Lindgren, . Engineer. Mr. Junius C. Wing, Farmer. Mr. George W. Gardner, Carpenter. CONSULTING BOARD OF PHYSICIANS. -

Of 379 Institutons Receiving a Questionnaire on Their Paramedical
DOCUMENT RESUME ED 022 442 JC 680 311 INVENTORY 1967: MASSACHUSETTS HEALTH MANPOWER TRAINING AT LESS THAN A BACCALAUREATE LEVEL. PART I. Training Center for Comprehensive Care, Jamaica Plain, Mass. Pula Date 67 Note-96p. EDRS Price MF-S0.50 HC-$3.92 Descriptors-*HEALTH OCCUPATIONS, *JUNIOR COLLEGES, *MANPOWER DEVELOPMENT, MEDICAL RECORD TECHNICIANS, fvEDICAL SERVICES, NURSES, NURSES AIDES, *PARAMEDICAL OCCUPATIONS, *SUBPROFESSIONALS, THERAPISTS, VOCATIONAL EDUCATION Identifiers *Massachusetts Of 379 institutonsreceiving a questionnaire on their paramedical training programs, 369 replied. They supplied data on 465 courses in 56 job categories. Those conducting the courses include hospitals, nursing homes, highschools, colleges, universities, technical schools, community service agencies, the State Department of Public Health, and an industrial plant. For each job category are given (1) a definition, (2) a detailed description of the curriculum, (3) the teaching staff, (4) a hst of the places offering the course, (5) the cost of the course, (6) in-training payment, if any, for taking the course, (7) length of time required for the course, and (8) ehgibility requirements for the trainee. (HH) U.S.melitillMMIN DEPARIMENTOFFICE OF HEALTH, OF EDUCATION EDUCATION &WELFARE THIS DOCUMENT HAS BEEN REPRODUCEDEXACTLY AS RECEIVED FROM THE PERSONPOSITIONSTATEDMASSACHUSETTS DO OR OR NOT ORGANIZATION POLICY. NECESSARILY ORIGINATING REPRESENT IT.OFFICIALPOINTS OFFICE OF VIEW OF EDUCATION OR OPINIONS ATHEALTH LESS THANMANPOWERAINVENTORY BACCALAUREATETRAITLEVEL ING fteb 1967 Training Center170 Mortonfor Comprehensive Street Care i Jamaica PARTPlain, ONEMass. 02130 1 MASSACHUSETTS IHEALTH N V E N T O RMANPOWER Y 19 6 7 TRAINING 1 AT LESS THAN ACONTENTS BACCALAUREATELEVEL IntroductionSponsorship of the survey Pages1-2 TheMethodDefinition Situation used ofin trainingconducting the survey 3-5 Location.JobNumberrequirements. -

Localizing the History of Mental Health Institutions, a Study of the Vermont State Asylum for the Insane, 1891-1912
University of New Hampshire University of New Hampshire Scholars' Repository Master's Theses and Capstones Student Scholarship Winter 2019 “Taken to Vt. State Hospital”: Localizing the History of Mental Health Institutions, A Study of the Vermont State Asylum for the Insane, 1891-1912 Alecia Bassett University of New Hampshire, Durham Follow this and additional works at: https://scholars.unh.edu/thesis Recommended Citation Bassett, Alecia, "“Taken to Vt. State Hospital”: Localizing the History of Mental Health Institutions, A Study of the Vermont State Asylum for the Insane, 1891-1912" (2019). Master's Theses and Capstones. 1318. https://scholars.unh.edu/thesis/1318 This Thesis is brought to you for free and open access by the Student Scholarship at University of New Hampshire Scholars' Repository. It has been accepted for inclusion in Master's Theses and Capstones by an authorized administrator of University of New Hampshire Scholars' Repository. For more information, please contact [email protected]. “TAKEN TO VT. STATE HOSPITAL”: LOCALIZING THE HISTORY OF MENTAL HEALTH INSTITUTIONS, A STUDY OF THE VERMONT STATE ASYLUM FOR THE INSANE, 1891-1912 BY ALECIA BASSETT BA History & Anthropology, University of New Hampshire, 2014 THESIS Submitted to the University of New Hampshire in Partial Fulfillment of the Requirements for the Degree of Master of Arts in History December 2019 ALL RIGHTS RESERVED © 2019 Alecia Bassett ii This thesis was examined and approved in partial fulfillment of the requirements for the degree of Master of Arts in History by: Thesis Director, Elizabeth Mellyn, Associate Professor of History Marion Girard Dorsey, Associate Professor of History Nikhil Tomar, Assistant Professor of Occupational Therapy Approval signatures are on file with the University of New Hampshire Graduate School.