Acute Stress Disorder Presenting with Delusional Misidentification Syndromes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paranoid – Suspicious; Argumentative; Paranoid; Continually on The
Disorder Gathering 34, 36, 49 Answer Keys A N S W E R K E Y, Disorder Gathering 34 1. Avital Agoraphobia – 2. Ewelina Alcoholism – 3. Martyna Anorexia – 4. Clarissa Bipolar Personality Disorder –. 5. Lysette Bulimia – 6. Kev, Annabelle Co-Dependant Relationship – 7. Archer Cognitive Distortions / all-of-nothing thinking (Splitting) – 8. Josephine Cognitive Distortions / Mental Filter – 9. Mendel Cognitive Distortions / Disqualifying the Positive – 10. Melvira Cognitive Disorder / Labeling and Mislabeling – 11. Liat Cognitive Disorder / Personalization – 12. Noa Cognitive Disorder / Narcissistic Rage – 13. Regev Delusional Disorder – 14. Connor Dependant Relationship – 15. Moira Dissociative Amnesia / Psychogenic Amnesia – (*Jason Bourne character) 16. Eylam Dissociative Fugue / Psychogenic Fugue – 17. Amit Dissociative Identity Disorder / Multiple Personality Disorder – 18. Liam Echolalia – 19. Dax Factitous Disorder – 20. Lorna Neurotic Fear of the Future – 21. Ciaran Ganser Syndrome – 22. Jean-Pierre Korsakoff’s Syndrome – 23. Ivor Neurotic Paranoia – 24. Tucker Persecutory Delusions / Querulant Delusions – 25. Lewis Post-Traumatic Stress Disorder – 26. Abdul Proprioception – 27. Alisa Repressed Memories – 28. Kirk Schizophrenia – 29. Trevor Self-Victimization – 30. Jerome Shame-based Personality – 31. Aimee Stockholm Syndrome – 32. Delphine Taijin kyofusho (Japanese culture-specific syndrome) – 33. Lyndon Tourette’s Syndrome – 34. Adar Social phobias – A N S W E R K E Y, Disorder Gathering 36 Adjustment Disorder – BERKELEY Apotemnophilia -

The Comorbidity of Reduplicative Paramnesia, Intermetamorphosis
Hindawi Publishing Corporation Case Reports in Psychiatry Volume 2014, Article ID 360480, 3 pages http://dx.doi.org/10.1155/2014/360480 Case Report The Comorbidity of Reduplicative Paramnesia, Intermetamorphosis, Reverse-Intermetamorphosis, Misidentification of Reflection, and Capgras Syndrome in an Adolescent Patient Ozden ArJsoy,1 A. Evren Tufan,2 Rabia Bilici,3 Sarper Taskiran,4 Zehra Topal,2 Nuran Demir,2 andM.AkifCansJz2 1 Department of Psychiatry, Abant Izzet Baysal University Medical Faculty, 14280 Bolu, Turkey 2 Department of Child and Adolescent Psychiatry, Abant Izzet Baysal University Medical Faculty, 14280 Bolu, Turkey 3 Erenkoy Hospital for Mental Disorders, 34738 Istanbul, Turkey 4 Department of Psychiatry, Koc University Medical Faculty, 34738 Istanbul, Turkey Correspondence should be addressed to A. Evren Tufan; [email protected] Received 17 July 2014; Accepted 7 September 2014; Published 23 September 2014 Academic Editor: Jaspreet S. Brar Copyright © 2014 Ozden Arısoy et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Delusional misidentification syndromes may be superimposed on neurological or psychiatric disorders and include delusional beliefs that the people, objects, or places around the patient change or are made to change with one another. In this paper, an adolescent patient displaying Capgras syndrome, metamorphosis, reverse-intermetamorphosis, misidentification of reflection, and reduplicative paramnesia was presented. The findings that our patient struggled with visuospatial tests applied in the acute phase as well as the observation that she refused to meet her family face-to-face while accepting to speak on the phone may support the role of right hemisphere and visuospatial functions in the development of those syndromes. -

A Case of Steroid Induced Mania
Case Report International Journal of Psychiatry A Case of Steroid Induced Mania 1* 1 Maryam M Alnasser , Yasser M Alanzi and Amena H * 2 Corresponding author Alhemyari Maryam M Alnasse, MBBS from University of Dammam, Saudi Arabia, E-mail: [email protected]. 1 MBBS from University of Dammam, Saudi Arabia. Submitted: 14 Dec 2016; Accepted: 26 Dec 2016; Published: 30 Dec 2016 2MBBS from King Faisal University, Saudi Arabia. Abstract Background: Steroids have been widely used and prescribed for a variety of systemic diseases. Although they prove to be highly effective, they have many physical and psychiatric adverse effects. The systemic side effects of these medications are well known and well studied, in contrast to the psychiatric adverse effects which its phenomenology needs to be the focus of more clinical studies. However, the incidence of diagnosable psychiatric disorders due to steroid therapy is reported to be 3-6%. Affective reactions such as depression, mania, and hypomania are the most common adverse effects, along with psychosis, anxiety and delirium. Aim: We describe a case of corticosteroid induced mania, its unusual clinical picture, its course and management. Case description: A 14-year-old female intermediate school student, with a recent diagnosis of Chron’s disease was brought to A&E department due to acute behavioral disturbance in form of confusion, visual hallucinations, psychomotor agitation, irritability, hyperactivity, talkativeness, lack of sleep, and physical aggression. Those symptoms have started few days following corticosteroid therapy which was Prednisolone 40mg PO OD. And she was diagnosed with steroid induced mania. Discussion: This case illustrates the need for more understanding of the phenomenology and diversity of corticosteroids induced psychiatric syndromes. -

The ICD-10 Classification of Mental and Behavioural Disorders : Clinical Descriptions and Diagnostic Guidelines
ICD-10 ThelCD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines | World Health Organization I Geneva I 1992 Reprinted 1993, 1994, 1995, 1998, 2000, 2002, 2004 WHO Library Cataloguing in Publication Data The ICD-10 classification of mental and behavioural disorders : clinical descriptions and diagnostic guidelines. 1.Mental disorders — classification 2.Mental disorders — diagnosis ISBN 92 4 154422 8 (NLM Classification: WM 15) © World Health Organization 1992 All rights reserved. Publications of the World Health Organization can be obtained from Marketing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications — whether for sale or for noncommercial distribution — should be addressed to Publications, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers' products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

28 Delusional Misidentification Syndromes In
DMS in OCD 1 Number of words: 1497 Number of tables: None Number of references: 28 Delusional misidentification syndromes in obsessive-compulsive disorder Isabela Melca, M.D., 1 Clarissa L. Rodrigues, M.D., 1 Maria A. Serra-Pinheiro, M.D., Ph.D. 1 Christos Pantelis, M.D., 2 Dennis Velakoulis, M.D., 2 Mauro V. Mendlowicz, M.D., PhD., 3 Leonardo F. Fontenelle, M.D., Ph.D. 1, 3-4 Running head: DMS in OCD _____________________________________________________________________________________________ 1 Anxiety and Depression Research Program, Institute of Psychiatry, Federal University of Rio de Janeiro, Brazil; 2 Melbourne Neuropsychiatry Centre, University of Melbourne, Australia 3 Department of Psychiatry and Mental Health, Institute of Community Health, Fluminense Federal University, Brazil; 4 D'Or Institute for Research and Education (IDOR), Rio de Janeiro, Brazil. Conflict of interest: All authors, with exception of Dr. Serra-Pinheiro, declare that they have no conflict of interest. Dr. Serra-Pinheiro has served as consultant for SIRE and received academic support for medical meetings from SIRE, Eli-lilly, Novartis and Janssen. Acknowledgements: Prof. Leonardo Fontenelle was supported by grants from Fundação de Apoio a Pesquisa do Estado do Rio de Janeiro (FAPERJ and Conselho Nacional de Desenvolvimento Científico e Tecnoógico (CNPq). Prof. Christos Pantelis was supported by a National Health and Medical Research Council (NHMRC) Senior Principal Research Fellowship and NHMRC Program Grants. Corresponding author: Leonardo F. Fontenelle, M.D., Ph.D. Rua Visconde de Pirajá, 547, Sala 719, Ipanema, Rio de Janeiro, CEP: 22410-003, Tel and Fax: +55- 21-2239-4919, E-mail: [email protected] Key words: Obsessive-Compulsive Disorder; Delusions; Capgras Syndrome; Psychopathology DMS in OCD 2 Abstract Delusional misidentification syndromes (DMS) have been rarely reported in patients with conditions other than schizophrenia-related disorders, diffuse brain disease (dementia) and focal neurological illness. -

On the Edge of Capgras' Syndrome
JOURNAL OF PSYCHOPATHOLOGY Online First Case report 2021;Mar 20. doi: 10.36148/2284-0249-386 On the edge of Capgras’ syndrome Andrea Turano1, Cecilia Caravaggi2, Giuseppe Ducci2, Silvia Bernardini2, Pier Luca Bandinelli2 1 Department of Pyschiatry, Sapienza University of Rome, Sant’Andrea Hospital, Rome, Italy; 2 Department of Mental Health ASL Roma 1, Rome, Italy SUMMARY Capgras’ syndrome, the delusional belief in the existence of doubles of others or of one- self, belongs to the delusional misidentification syndromes (DMSs), a group of syndromes characterized by delusional misidentification of oneself and/or of other people. These syn- dromes are not codified as diagnoses per se on the DSM-5 or on the ICD-11, and are usually seen as specific presentations of broader psychiatric disorders. Capgras’ syndrome has been shown on both psychiatric and non-psychiatric disorders, thus not being a manageable tool in helping clinicians to define a diagnosis. Presenting what we believe is a special case of Capgras’ syndrome, we aim to propose a characterization of such syndrome very specific of schizophrenic – and thus psychiatric – conditions, which may turn especially useful in clinical pictures where no other psychiatric or medical symptoms are found and can help defining a diagnosis. Key words: Capgras’ syndrome, delusional misidentification syndromes, differential diagnosis Non c’è uomo che a forza di portare una maschera, non finisca per assimilare a questa anche il suo vero volto. Received: April 30, 2020 Accepted: December 10, 2020 (Nathaniel Hawthorne; La lettera scarlatta) Correspondence Pier Luca Bandinelli Introduction Department of Psychiatry, SPDC San Filippo In classic psychopathology there was a tendency toward giving names Neri, via G. -

The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic Criteria for Research
The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic criteria for research World Health Organization Geneva The World Health Organization is a specialized agency of the United Nations with primary responsibility for international health matters and public health. Through this organization, which was created in 1948, the health professions of some 180 countries exchange their knowledge and experience with the aim of making possible the attainment by all citizens of the world by the year 2000 of a level of health that will permit them to lead a socially and economically productive life. By means of direct technical cooperation with its Member States, and by stimulating such cooperation among them, WHO promotes the development of comprehensive health services, the prevention and control of diseases, the improvement of environmental conditions, the development of human resources for health, the coordination and development of biomedical and health services research, and the planning and implementation of health programmes. These broad fields of endeavour encompass a wide variety of activities, such as developing systems of primary health care that reach the whole population of Member countries; promoting the health of mothers and children; combating malnutrition; controlling malaria and other communicable diseases including tuberculosis and leprosy; coordinating the global strategy for the prevention and control of AIDS; having achieved the eradication of smallpox, promoting mass immunization against a number of other -
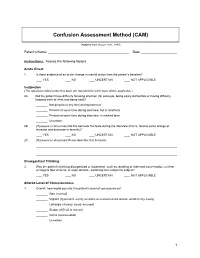
Confusion Assessment Method (CAM)
Confusion Assessment Method (CAM) (Adapted from Inouye et al., 1990) Patient’s Name: Date: Instructions: Assess the following factors. Acute Onset 1. Is there evidence of an acute change in mental status from the patient’s baseline? YES NO UNCERTAIN NOT APPLICABLE Inattention (The questions listed under this topic are repeated for each topic where applicable.) 2A. Did the patient have difficulty focusing attention (for example, being easily distractible or having difficulty keeping track of what was being said)? Not present at any time during interview Present at some time during interview, but in mild form Present at some time during interview, in marked form Uncertain 2B. (If present or abnormal) Did this behavior fluctuate during the interview (that is, tend to come and go or increase and decrease in severity)? YES NO UNCERTAIN NOT APPLICABLE 2C. (If present or abnormal) Please describe this behavior. Disorganized Thinking 3. Was the patient’s thinking disorganized or incoherent, such as rambling or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable, switching from subject to subject? YES NO UNCERTAIN NOT APPLICABLE Altered Level of Consciousness 4. Overall, how would you rate this patient’s level of consciousness? Alert (normal) Vigilant (hyperalert, overly sensitive to environmental stimuli, startled very easily) Lethargic (drowsy, easily aroused) Stupor (difficult to arouse) Coma (unarousable) Uncertain 1 Disorientation 5. Was the patient disoriented at any time during the interview, such as thinking that he or she was somewhere other than the hospital, using the wrong bed, or misjudging the time of day? YES NO UNCERTAIN NOT APPLICABLE Memory Impairment 6. -

Lamotrigine As a Treatment of Agitation in Dementia F
Lamotrigine as a treatment of agitation in Dementia F. Godinho1, A. Valverde2. 1Hospital Espirito Santo de Évora, Department of Psychiatry and Mental Health, Évora, Portugal. 2Hospital Professor Doutor Fernando da Fonseca, Neurology Service, Amadora, Portugal. Background: • Psychomotor agitation is common in patients with dementia but there are no well-established or evidenced-based effective treatments. • Non-pharmacological interventions remain the mainstay of treatment but are not always feasible or sufficient. • Antipsychotic are the most commonly used drugs but concerns regarding tolerability limit their use. • Anticonvulsants are receiving growing attention due to their better safety profile. Objective: Methods: We report a case of a patient with dementia and behavioral disturbance Retrospective review of the clinical chart and literature review on the treated with lamotrigine, and make a brief review of the literature of topic. anticonvulsants use in the treatment of agitation and aggression in dementia. RESULTS Clinical case • A 69 years-old woman with behavioral variant Frontotemporal Dementia, severe stage, totally dependent on activities of daily living and with severe speech difficulties, developed progressive aggressive behavior. • In the following 6 months, quetiapine until 200mg/daily and then risperidone until 1mg/daily was tried, with no success. • Lamotrigine was then introduced and titrated until 100mg/daily. • Since this dosage and in the 2 next consultations, no more aggressive behavior were observed Literature Review -

7 Leis Layout 1
ACTAVol. 17, No. 4, 2019, 455-467 REVIEW ARTICLE NEUROPSYCHOLOGICA Received: 22.02.2019 Accepted: 22.12.2019 DELUSIONAL MISIDENTIFICATION A – Study Design SYNDROME: DISSOCIATION BETWEEN B – Data Collection C – Statistical Analysis RECOGNITION AND IDENTIFICATION D – Data Interpretation E – Manuscript Preparation F – Literature Search PROCESSES G – Funds Collection Authors: Kamil Leis1(A,B,D,E,F,G), Ewelina Mazur1(A,B,D,E,F), Mariusz Racinowski1(A,B,D,E,F), Tomasz Jamrożek1(A,B,D,E), Jakub Gołębiewski1(A,B,D,F), Przemysław Gałązka2(A,B,E,F), Maria Pąchalska3(A,B,D,E,G) 1 Faculty of Medicine, Ludwik Rydygier Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Toruń, Bydgoszcz, Poland 2 Department of General and Oncological Surgery for Children and Adolescents, Antoni Jurasz University Hospital No. 1 in Bydgoszcz, Ludwik Rydygier Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Toruń, Bydgoszcz, Poland 3 Chair of Neuropsychology and Neurorehabilitation, Cracow University, Cracow, Poland SUMMARY Delusional misidentification syndrome (DMS) is an umbrella term for syndromes of intermetamorphosis, Fregoli, and Capgras. DMS) is thought to be related to dissociation between recognition and identification processes. DMS was described for the first time in 1932 as a variant of the Capgras syndrome and is currently on the DSM-V list of diseases as an independent disease entity. Patients affected by DMS believed that people around them, most often family, have changed physically (appearance) and mentally (char- acter). Other symptoms include confabulation, derealization or de- personalization. In patients, aggressive behavior is often observed, aimed at alleged doppelgangers resulting from the sense of being cheated and manipulated. -

Does Psychomotor Agitation in Major Depressive Episodes Indicate Bipolarity? Evidence from the Zurich Study
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by RERO DOC Digital Library Eur Arch Psychiatry Clin Neurosci (2009) 259:55–63 DOI 10.1007/s00406-008-0834-7 ORIGINAL PAPER Jules Angst Æ Alex Gamma Æ Franco Benazzi Æ Vladeta Ajdacic Æ Wulf Ro¨ssler Does psychomotor agitation in major depressive episodes indicate bipolarity? Evidence from the Zurich Study Received: 4 September 2007 / Accepted: 5 June 2008 / Published online: 19 September 2008 j Abstract Background Kraepelin’s partial interpre- were equally associated with the indicators of bipolarity tation of agitated depression as a mixed state of and with anxiety. Longitudinally, agitation and retar- ‘‘manic-depressive insanity’’ (including the current dation were significantly associated with each other concept of bipolar disorder) has recently been the focus (OR = 1.8, 95% CI = 1.0–3.2), and this combined of much research. This paper tested whether, how, and group of major depressives showed stronger associa- to what extent both psychomotor symptoms, agitation tions with bipolarity, with both hypomanic/cyclothy- and retardation in depression are related to bipolarity mic and depressive temperamental traits, and with and anxiety. Method The prospective Zurich Study anxiety. Among agitated, non-retarded depressives, assessed psychiatric and somatic syndromes in a unipolar mood disorder was even twice as common as community sample of young adults (N = 591) (aged bipolar mood disorder. Conclusion Combined agitated 20 at first interview) by six interviews over 20 years and retarded major depressive states are more often (1979–1999). Psychomotor symptoms of agitation and bipolar than unipolar, but, in general, agitated retardation were assessed by professional interviewers depression (with or without retardation) is not more from age 22 to 40 (five interviews) on the basis of the frequently bipolar than retarded depression (with or observed and reported behaviour within the interview without agitation), and pure agitated depression is even section on depression. -

Identifying and Treating Postpartum Depression June Andrews Horowitz and Janice H
CLINICAL ISSUES Identifying and Treating Postpartum Depression June Andrews Horowitz and Janice H. Goodman Postpartum depression affects 10% to 20% of Despite adverse health consequences, systematic women in the United States and negatively influences PPD screening is not standard clinical practice in the maternal, infant, and family health. Assessment of risk United States. Limited availability of psychiatric factors and depression symptoms is needed to identi- services impedes referral for evaluation and treat- fy women at risk for postpartum depression for early ment. Nurses require knowledge about the nature referral and treatment. Individual and group psy- and efficacy of PPD treatments to refer their clients chotherapy have demonstrated efficacy as treatments, and recommend psychiatric services with confi- and some complementary/alternative therapies show dence. To inform nursing practice, this article promise. Treatment considerations include severity of describes PPD, examines screening approaches, and depression, whether a mother is breastfeeding, and synthesizes the literature concerning evidence-based mother’s preference. Nurses who work with childbear- treatments for PPD. ing women can advise depressed mothers regarding treatment options, make appropriate recommenda- Overview of Postpartum Depression tions, provide timely and accessible referrals, and encourage engagement in treatment. JOGNN, 34, 264–273; 2005. DOI: 10.1177/0884217505274583 Description, Prevalence, and Course Keywords: Mental health—Postpartum depres- Symptoms