Understanding and Predicting Cancer Cell Aggressiveness from Their Migratory Phenotypes • Advisor: Konstantinos Konstantopoulos
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Podocalyxin Is Required for Maintaining Blood–Brain Barrier Function During Acute Inflammation
Podocalyxin is required for maintaining blood–brain barrier function during acute inflammation Jessica Caita, Michael R. Hughesa,1, Matthew R. Zeglinskib,c,d, Allen W. Chane,f,g,h,i, Sabrina Osterhofa, R. Wilder Scotta,j, Diana Canals Hernaeza, Alissa Caita, A. Wayne Voglj,k, Pascal Bernatchezd,l, T. Michael Underhilla,j, David J. Granvilleb,c,d, Timothy H. Murphye,f,g, Calvin D. Roskelleyj,k, and Kelly M. McNagnya,1 aBiomedical Research Centre, University of British Columbia, Vancouver, BC, Canada V6T 1Z3; bICORD Centre, University of British Columbia, Vancouver, BC, Canada V5Z 1M9; cDepartment of Pathology and Laboratory Medicine, University of British Columbia, Vancouver, BC, Canada V6T 2B5; dCentre for Heart and Lung Innovation, St Paul’s Hospital, Vancouver, BC, Canada V6Z 1Y6; eDepartment of Psychiatry, University of British Columbia, Vancouver, BC, Canada V6T 2A1; fKinsmen Laboratory of Neurological Research, University of British Columbia, Vancouver, BC, Canada V6T 1Z4; gDjavad Mowafaghian Center for Brain Health, University of British Columbia, Vancouver, BC, Canada V6T 1Z3; hNeuroscience and Mental Health Institute, University of Alberta, Edmonton, AB, Canada T6G 2R3; iNeurochemical Research Unit, Department of Psychiatry, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, AB, Canada T6G 2R3; jDepartment of Cellular and Physiological Sciences, University of British Columbia, Vancouver, BC, Canada V6T 1Z4; kLife Sciences Institute, University of British Columbia, Vancouver, BC, Canada V6T 1Z4; and lDepartment of Anaesthesiology, Pharmacology & Therapeutics, University of British Columbia, Vancouver, BC, Canada V6T 1Z3 Edited by Lawrence Steinman, Stanford University School of Medicine, Stanford, CA, and approved January 15, 2019 (received for review September 6, 2018) Podocalyxin (Podxl) is broadly expressed on the luminal face of and plasma factors to effect repair. -

Exome Sequencing and in Vitro Studies Identified Podocalyxin As a Candidate Gene for Focal and Segmental Glomerulosclerosis
Exome sequencing and in vitro studies identified podocalyxin as a candidate gene for focal and segmental glomerulosclerosis The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Barua, Moumita, Eric Shieh, Johannes Schlondorff, Giulio Genovese, Bernard S Kaplan, and Martin R Pollak. 2013. “Exome sequencing and in vitro studies identified podocalyxin as a candidate gene for focal and segmental glomerulosclerosis.” Kidney international 85 (1): 124-133. doi:10.1038/ki.2013.354. http://dx.doi.org/10.1038/ ki.2013.354. Published Version doi:10.1038/ki.2013.354 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:12717580 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA NIH Public Access Author Manuscript Kidney Int. Author manuscript; available in PMC 2014 July 01. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Kidney Int. 2014 January ; 85(1): 124–133. doi:10.1038/ki.2013.354. Exome sequencing and in vitro studies identified podocalyxin as a candidate gene for focal and segmental glomerulosclerosis Moumita Barua1,2,+, Eric Shieh2,+, Johannes Schlondorff1,2, Giulio Genovese3,4,5, Bernard S Kaplan6, and Martin R Pollak1,2 1Division of Nephrology, Dept. of Medicine, Beth Israel Deaconess -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Identification of Cell-Surface Proteins Endocytosed by Human Brain
pharmaceutics Article Identification of Cell-Surface Proteins Endocytosed by Human Brain Microvascular Endothelial Cells In Vitro Shingo Ito 1,2,3, Mariko Oishi 2, Seiryo Ogata 3, Tatsuki Uemura 3, Pierre-Olivier Couraud 4, Takeshi Masuda 1,2,3 and Sumio Ohtsuki 1,2,3,* 1 Department of Pharmaceutical Microbiology, Faculty of Life Sciences, Kumamoto University, 5-1 Oe-honmachi, Chuo-ku, Kumamoto 862-0973, Japan; [email protected] (S.I.); [email protected] (T.M.) 2 Department of Pharmaceutical Microbiology, School of Pharmacy, Kumamoto University, 5-1 Oe-honmachi, Chuo-ku, Kumamoto 862-0973, Japan; [email protected] 3 Department of Pharmaceutical Microbiology, Graduate School of Pharmaceutical Sciences, Kumamoto University, 5-1 Oe-honmachi, Chuo-ku, Kumamoto 862-0973, Japan; [email protected] (S.O.); [email protected] (T.U.) 4 Institut Cochin, Universite de Paris, Inserm U1016, CNRS UMR8104, 22 rue Méchain, 75014 Paris, France; [email protected] * Correspondence: [email protected]; Tel.: +81-96-371-4323 Received: 30 April 2020; Accepted: 18 June 2020; Published: 23 June 2020 Abstract: Cell-surface proteins that can endocytose into brain microvascular endothelial cells serve as promising candidates for receptor-mediated transcytosis across the blood–brain barrier (BBB). Here, we comprehensively screened endocytic cell-surface proteins in hCMEC/D3 cells, a model of human brain microvascular endothelial cells, using surface biotinylation methodology and sequential window acquisition of all theoretical fragment-ion spectra-mass spectrometry (SWATH-MS)-based quantitative proteomics. Using this method, we identified 125 endocytic cell-surface proteins from hCMEC/D3 cells. -

PODXL Antibody
Efficient Professional Protein and Antibody Platforms PODXL Antibody Basic information: Catalog No.: UMA60669 Source: Mouse Size: 50ul/100ul Clonality: Monoclonal Concentration: 1mg/ml Isotype: Mouse IgG1 Purification: Protein G affinity purified Useful Information: Applications: ICC:1:200-1:500 Reactivity: Human Specificity: This antibody recognizes PODXL protein. Immunogen: recombinant protein Podocalyxin, a sialoglycoprotein, is thought to be the major constituent of the glycocalyx of podocytes. It is a member of the CD34 family of trans- membrane sialomucins. It is involved in the regulation of both adhesion and cell morphology and cancer progression. It functions as an anti-adhesive molecule that maintains an open filtration pathway between neighboring foot processes in the podocyte by charge repulsion. Podocalyxin acts as a Description: pro-adhesive molecule, enhancing the adherence of cells to immobilized ligands, increasing the rate of migration and cell-cell contacts in an integ- rin-dependent manner. Sialylated, O-glycosylated glycoforms of podocalyxin expressed by colon carcinoma cells possess L-selectin and E-selectin binding activity, and may be pivotal to the metastatic spread of colon carcinoma cells. Uniprot: O00592 BiowMW: 58kDa Buffer: 1*TBS (pH7.4), 1%BSA, 40%Glycerol. Preservative: 0.05% Sodium Azide. Storage: Store at 4°C short term and -20°C long term. Avoid freeze-thaw cycles. Note: For research use only, not for use in diagnostic procedure. Data: ICC staining PODXL in HCT116 cells (red). Cells were fixed in paraformaldehyde, permeabilised with 0.25% Triton X100/PBS. Gene Universal Technology Co. Ltd www.universalbiol.com Tel: 0550-3121009 E-mail: [email protected] Efficient Professional Protein and Antibody Platforms Gene Universal Technology Co. -

A Single-Cell Transcriptome Atlas of the Mouse Glomerulus
RAPID COMMUNICATION www.jasn.org A Single-Cell Transcriptome Atlas of the Mouse Glomerulus Nikos Karaiskos,1 Mahdieh Rahmatollahi,2 Anastasiya Boltengagen,1 Haiyue Liu,1 Martin Hoehne ,2 Markus Rinschen,2,3 Bernhard Schermer,2,4,5 Thomas Benzing,2,4,5 Nikolaus Rajewsky,1 Christine Kocks ,1 Martin Kann,2 and Roman-Ulrich Müller 2,4,5 Due to the number of contributing authors, the affiliations are listed at the end of this article. ABSTRACT Background Three different cell types constitute the glomerular filter: mesangial depending on cell location relative to the cells, endothelial cells, and podocytes. However, to what extent cellular heteroge- glomerular vascular pole.3 Because BP ad- neity exists within healthy glomerular cell populations remains unknown. aptation and mechanoadaptation of glo- merular cells are key determinants of kidney Methods We used nanodroplet-based highly parallel transcriptional profiling to function and dysregulated in kidney disease, characterize the cellular content of purified wild-type mouse glomeruli. we tested whether glomerular cell type sub- Results Unsupervised clustering of nearly 13,000 single-cell transcriptomes identi- sets can be identified by single-cell RNA fied the three known glomerular cell types. We provide a comprehensive online sequencing in wild-type glomeruli. This atlas of gene expression in glomerular cells that can be queried and visualized using technique allows for high-throughput tran- an interactive and freely available database. Novel marker genes for all glomerular scriptome profiling of individual cells and is cell types were identified and supported by immunohistochemistry images particularly suitable for identifying novel obtained from the Human Protein Atlas. -

Anti-PODXL Antibody (ARG41386)
Product datasheet [email protected] ARG41386 Package: 100 μl anti-PODXL antibody Store at: -20°C Summary Product Description Rabbit Polyclonal antibody recognizes PODXL Tested Reactivity Hu Tested Application FACS, ICC/IF, IHC-P, WB Host Rabbit Clonality Polyclonal Isotype IgG Target Name PODXL Antigen Species Human Immunogen Synthetic peptide derived from Human PODXL. Conjugation Un-conjugated Alternate Names Gp200; GCTM-2 antigen; PCLP; Podocalyxin; PC; PCLP-1; Podocalyxin-like protein 1 Application Instructions Application table Application Dilution FACS 1:100 ICC/IF 1:100 - 1:500 IHC-P 1:50 - 1:200 WB 1:500 - 1:2000 Application Note * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Calculated Mw 59 kDa Properties Form Liquid Purification Affinity purified. Buffer PBS (pH 7.4), 150 mM NaCl, 0.02% Sodium azide and 50% Glycerol. Preservative 0.02% Sodium azide Stabilizer 50% Glycerol Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed before use. www.arigobio.com 1/2 Note For laboratory research only, not for drug, diagnostic or other use. Bioinformation Gene Symbol PODXL Gene Full Name podocalyxin-like Background This gene encodes a member of the sialomucin protein family. The encoded protein was originally identified as an important component of glomerular podocytes. Podocytes are highly differentiated epithelial cells with interdigitating foot processes covering the outer aspect of the glomerular basement membrane. -

A Direct Podocalyxin-Dynamin-2 Interaction Regulates Cytoskeletal Dynamics to Promote Migration and Metastasis in Pancreatic Cancer Cells
Author Manuscript Published OnlineFirst on April 11, 2019; DOI: 10.1158/0008-5472.CAN-18-3369 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Title A Direct Podocalyxin-Dynamin-2 Interaction Regulates Cytoskeletal Dynamics to Promote Migration and Metastasis in Pancreatic Cancer Cells Authors Bin Sheng Wong1,2, Daniel J. Shea1, Panagiotis Mistriotis1,2, Soontorn Tuntithavornwat1, Robert A. Law1, Jake M. Bieber1, Lei Zheng5, Konstantinos Konstantopoulos1,2,3,4,5,* Affiliations 1Department of Chemical and Biomolecular Engineering, The Johns Hopkins University, Baltimore, MD 21218, USA. 2Institute for NanoBioTechnology, The Johns Hopkins University, Baltimore, MD 21218, USA. 3Johns Hopkins Physical Sciences-Oncology Center, The Johns Hopkins University, Baltimore, MD 21218, USA. 4Department of Biomedical Engineering, The Johns Hopkins University, Baltimore MD, 21218, USA. 5Department of Oncology, The Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA. *Correspondence: [email protected] (Konstantinos Konstantopoulos, 410-516-6290, The Johns Hopkins University, 3400 N. Charles Street, 114 Croft Hall, Baltimore, MD 21218) Running Title Podocalyxin-dynamin-2 interaction promotes cancer migration Keywords Podocalyxin, Dynamin-2, Pancreatic Cancer, Cell Migration, Metastasis Additional Information The authors acknowledge funding support from the US National Institutes of Health (Grant R01CA186286). The authors declare no potential conflicts of interest. 1 Downloaded from cancerres.aacrjournals.org on September 24, 2021. © 2019 American Association for Cancer Research. Author Manuscript Published OnlineFirst on April 11, 2019; DOI: 10.1158/0008-5472.CAN-18-3369 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Abstract The sialoglycoprotein podocalyxin is absent in normal pancreas but is overexpressed in pancreatic cancer and is associated with poor clinical outcome. -

Human Transcription Factors Responsive to Initial Reprogramming Predominantly Undergo Legitimate Reprogramming During Fbroblast Conversion to Ipscs Ricardo R
www.nature.com/scientificreports OPEN Human transcription factors responsive to initial reprogramming predominantly undergo legitimate reprogramming during fbroblast conversion to iPSCs Ricardo R. Cevallos1, Yvonne J. K. Edwards1,2, John M. Parant3, Bradley K. Yoder2 & Kejin Hu1* The four transcription factors OCT4, SOX2, KLF4, and MYC (OSKM) together can convert human fbroblasts to induced pluripotent stem cells (iPSCs). It is, however, perplexing that they can do so only for a rare population of the starting cells with a long latency. Transcription factors (TFs) defne identities of both the starting fbroblasts and the end product, iPSCs, and are also of paramount importance for the reprogramming process. It is critical to upregulate or activate the iPSC-enriched TFs while downregulate or silence the fbroblast-enriched TFs. This report explores the initial TF responses to OSKM as the molecular underpinnings for both the potency aspects and the limitation sides of the OSKM reprogramming. The authors frst defned the TF reprogramome, i.e., the full complement of TFs to be reprogrammed. Most TFs were resistant to OSKM reprogramming at the initial stages, an observation consistent with the inefciency and long latency of iPSC reprogramming. Surprisingly, the current analyses also revealed that most of the TFs (at least 83 genes) that did respond to OSKM induction underwent legitimate reprogramming. The initial legitimate transcriptional responses of TFs to OSKM reprogramming were also observed in the reprogramming fbroblasts from a diferent individual. Such early biased legitimate reprogramming of the responsive TFs aligns well with the robustness aspect of the otherwise inefcient and stochastic OSKM reprogramming. OCT4, SOX2, KLF4, and MYC (collectively OSKM) can convert human fbroblasts into induced pluripotent stem cells (iPSCs), which are the man-made version of embryonic stem cells (ESCs)1–3. -

A Grainyhead-Like 2/Ovo-Like 2 Pathway Regulates Renal Epithelial Barrier Function and Lumen Expansion
BASIC RESEARCH www.jasn.org A Grainyhead-Like 2/Ovo-Like 2 Pathway Regulates Renal Epithelial Barrier Function and Lumen Expansion † ‡ | Annekatrin Aue,* Christian Hinze,* Katharina Walentin,* Janett Ruffert,* Yesim Yurtdas,*§ | Max Werth,* Wei Chen,* Anja Rabien,§ Ergin Kilic,¶ Jörg-Dieter Schulzke,** †‡ Michael Schumann,** and Kai M. Schmidt-Ott* *Max Delbrueck Center for Molecular Medicine, Berlin, Germany; †Experimental and Clinical Research Center, and Departments of ‡Nephrology, §Urology, ¶Pathology, and **Gastroenterology, Charité Medical University, Berlin, Germany; and |Berlin Institute of Urologic Research, Berlin, Germany ABSTRACT Grainyhead transcription factors control epithelial barriers, tissue morphogenesis, and differentiation, but their role in the kidney is poorly understood. Here, we report that nephric duct, ureteric bud, and collecting duct epithelia express high levels of grainyhead-like homolog 2 (Grhl2) and that nephric duct lumen expansion is defective in Grhl2-deficient mice. In collecting duct epithelial cells, Grhl2 inactivation impaired epithelial barrier formation and inhibited lumen expansion. Molecular analyses showed that GRHL2 acts as a transcrip- tional activator and strongly associates with histone H3 lysine 4 trimethylation. Integrating genome-wide GRHL2 binding as well as H3 lysine 4 trimethylation chromatin immunoprecipitation sequencing and gene expression data allowed us to derive a high-confidence GRHL2 target set. GRHL2 transactivated a group of genes including Ovol2, encoding the ovo-like 2 zinc finger transcription factor, as well as E-cadherin, claudin 4 (Cldn4), and the small GTPase Rab25. Ovol2 induction alone was sufficient to bypass the requirement of Grhl2 for E-cadherin, Cldn4,andRab25 expression. Re-expression of either Ovol2 or a combination of Cldn4 and Rab25 was sufficient to rescue lumen expansion and barrier formation in Grhl2-deficient collecting duct cells. -

Peripheral Nerve Single-Cell Analysis Identifies Mesenchymal Ligands That Promote Axonal Growth
Research Article: New Research Development Peripheral Nerve Single-Cell Analysis Identifies Mesenchymal Ligands that Promote Axonal Growth Jeremy S. Toma,1 Konstantina Karamboulas,1,ª Matthew J. Carr,1,2,ª Adelaida Kolaj,1,3 Scott A. Yuzwa,1 Neemat Mahmud,1,3 Mekayla A. Storer,1 David R. Kaplan,1,2,4 and Freda D. Miller1,2,3,4 https://doi.org/10.1523/ENEURO.0066-20.2020 1Program in Neurosciences and Mental Health, Hospital for Sick Children, 555 University Avenue, Toronto, Ontario M5G 1X8, Canada, 2Institute of Medical Sciences University of Toronto, Toronto, Ontario M5G 1A8, Canada, 3Department of Physiology, University of Toronto, Toronto, Ontario M5G 1A8, Canada, and 4Department of Molecular Genetics, University of Toronto, Toronto, Ontario M5G 1A8, Canada Abstract Peripheral nerves provide a supportive growth environment for developing and regenerating axons and are es- sential for maintenance and repair of many non-neural tissues. This capacity has largely been ascribed to paracrine factors secreted by nerve-resident Schwann cells. Here, we used single-cell transcriptional profiling to identify ligands made by different injured rodent nerve cell types and have combined this with cell-surface mass spectrometry to computationally model potential paracrine interactions with peripheral neurons. These analyses show that peripheral nerves make many ligands predicted to act on peripheral and CNS neurons, in- cluding known and previously uncharacterized ligands. While Schwann cells are an important ligand source within injured nerves, more than half of the predicted ligands are made by nerve-resident mesenchymal cells, including the endoneurial cells most closely associated with peripheral axons. At least three of these mesen- chymal ligands, ANGPT1, CCL11, and VEGFC, promote growth when locally applied on sympathetic axons. -
Inline-Supplementary-Material-6.Pdf
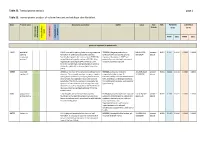
Table S3. Transcriptome analysis page 1 Table S3. Transcriptomic analysis of cultured mutant and wildtype skin fibroblast. Gene Protein name GeneCards annotation OMIM Locus Fold FDR PATIENTS CONTROLS - change (n=2) (n=4) ment apoptosis apoptosis Keratinocyte Keratinocyte inflammation differentiation Neurodevelop cell growth and growth cell FPKM [SD] FPKM [SD] genes up-regulated in patient cells ESRP1 epithelial ESRP1 is an mRNA splicing factor that regulates the *612959, the gene product is an 8:95653301 - present - 0.011 0.3547 0.0038 0.0000 0.0000 splicing formation of epithelial cell-specific isoforms. epithelial cell-type-specific splicing 95719694 absent regulatory Specifically regulates the expression of FGFR2-IIIb, regulator. Mutations in ESRP1 are protein 1 an epithelial cell-specific isoform of FGFR2. Also potentially associated with autosomal regulates the splicing of CD44, CTNND1, ENAH, recessive deafness type 109. three transcripts that undergo changes in splicing during the epithelial-to-mesenchymal transition (EMT). CERS3 ceramide CERS3 is a member of the ceramide synthase family #615023, autosomal recessive 15:100913143 - present - 0.011 0.1844 0.0118 0.0000 0.0000 synthase 3 of genes. The ceramide synthase enzymes regulate congenital ichthyosis type 9, 101085200 absent sphingolipid synthesis by catalyzing the formation characterized by collodian membrane at of ceramides from sphingoid base and acyl-CoA birth, acanthosis, orthohyperkeratosis, substrates. This family member is involved in the fine erythrodermic scales, palmoplantar synthesis of ceramides with ultra-long-chain acyl- hyperlinearity. moieties (ULC-Cers), important to the epidermis in its role in creating a protective barrier from the environment. GJB6 gap junction GJB6 encodes one of the connexin proteins.