A Case of Shock Due to Compression of the Right Atrium by the Liver After Postoperative Bleeding
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fluid Resuscitation Therapy for Hemorrhagic Shock
CLINICAL CARE Fluid Resuscitation Therapy for Hemorrhagic Shock Joseph R. Spaniol vides a review of the 4 types of shock, the 4 classes of Amanda R. Knight, BA hemorrhagic shock, and the latest research on resuscita- tive fluid. The 4 types of shock are categorized into dis- Jessica L. Zebley, MS, RN tributive, obstructive, cardiogenic, and hemorrhagic Dawn Anderson, MS, RN shock. Hemorrhagic shock has been categorized into 4 Janet D. Pierce, DSN, ARNP, CCRN classes, and based on these classes, appropriate treatment can be planned. Crystalloids, colloids, dopamine, and blood products are all considered resuscitative fluid treat- ment options. Each individual case requires various resus- ■ ABSTRACT citative actions with different fluids. Healthcare Hemorrhagic shock is a severe life-threatening emergency professionals who are knowledgeable of the information affecting all organ systems of the body by depriving tissue in this review would be better prepared for patients who of sufficient oxygen and nutrients by decreasing cardiac are admitted with hemorrhagic shock, thus providing output. This article is a short review of the different types optimal care. of shock, followed by information specifically referring to hemorrhagic shock. The American College of Surgeons ■ DISTRIBUTIVE SHOCK categorized shock into 4 classes: (1) distributive; (2) Distributive shock is composed of 3 separate categories obstructive; (3) cardiogenic; and (4) hemorrhagic. based on their clinical outcome. Distributive shock can be Similarly, the classes of hemorrhagic shock are grouped categorized into (1) septic; (2) anaphylactic; and (3) neu- by signs and symptoms, amount of blood loss, and the rogenic shock. type of fluid replacement. This updated review is helpful to trauma nurses in understanding the various clinical Septic shock aspects of shock and the current recommendations for In accordance with the American College of Chest fluid resuscitation therapy following hemorrhagic shock. -

Hemodynamic Profiles Related to Circulatory Shock in Cardiac Care Units
REVIEW ARTICLE Hemodynamic profiles related to circulatory shock in cardiac care units Perfiles hemodinámicos relacionados con el choque circulatorio en unidades de cuidados cardiacos Jesus A. Gonzalez-Hermosillo1, Ricardo Palma-Carbajal1*, Gustavo Rojas-Velasco2, Ricardo Cabrera-Jardines3, Luis M. Gonzalez-Galvan4, Daniel Manzur-Sandoval2, Gian M. Jiménez-Rodriguez5, and Willian A. Ortiz-Solis1 1Department of Cardiology; 2Intensive Cardiovascular Care Unit, Instituto Nacional de Cardiología Ignacio Chávez; 3Inernal Medicine, Hospital Ángeles del Pedregal; 4Posgraduate School of Naval Healthcare, Universidad Naval; 5Interventional Cardiology, Instituto Nacional de Cardiología Ignacio Chávez. Mexico City, Mexico Abstract One-third of the population in intensive care units is in a state of circulatory shock, whose rapid recognition and mechanism differentiation are of great importance. The clinical context and physical examination are of great value, but in complex situa- tions as in cardiac care units, it is mandatory the use of advanced hemodynamic monitorization devices, both to determine the main mechanism of shock, as to decide management and guide response to treatment, these devices include pulmonary flotation catheter as the gold standard, as well as more recent techniques including echocardiography and pulmonary ultra- sound, among others. This article emphasizes the different shock mechanisms observed in the cardiac care units, with a proposal for approach and treatment. Key words: Circulatory shock. Hemodynamic monitorization. -

Cardiac Arrest Due to Tension Pneumoperitoneum Caused by Esophagogastric Perforation and Pyloric Stenosis : a Case Report
Shinshu Med J, 67⑵:113~119, 2019 Cardiac Arrest Due to Tension Pneumoperitoneum Caused by Esophagogastric Perforation and Pyloric Stenosis : A Case Report 1 )* 1) 1) Hiroshi Miyama , Mayumi Okada , Hiroshi Takayama 1) 2) Hiroshi Imamura and Futoshi Muranaka 1) Department of Emergency and Critical Care Medicine, Shinshu University School of Medicine 2) Department of Surgery, Shinshu University School of Medicine Tension pneumothorax is one of the causes of sudden cardiac arrest with evidence of obstructive shock and subcutaneous emphysema. Emergency chest decompression is a treatment of choice in such a situation. Herein, we report a case of an out-of-hospital cardiac arrest due to tension pneumoperitoneum caused by esophagogas- tric perforation. A 40-year-old man with a history of duodenal ulcer and pyloric stenosis complained of sudden- onset abdominal pain and developed cardiac arrest during transportation to our hospital. He had jugular venous distention ; subcutaneous emphysema in the upper body trunk, arms, and neck ; and a markedly distended abdomen. Immediate needle-chest decompression was not effective, but after volume resuscitation, adrenaline administration, and abdominal decompression by nasogastric tube, spontaneous circulation was resumed. Radiological findings revealed tension pneumoperitoneum due to esophagogastric perforation. Emergency laparotomy was performed, and the perforation of the esophagogastric junction was detected. The patient was discharged from the hospital without any disability. Notably, in the treatment of a patient with cardiac arrest having subcutaneous emphysema, the cause of obstructive shock could exist not only in the chest, but also in the abdomen. Shinshu Med J 67 : 113―119, 2019 (Received for publication November 12, 2018 ; accepted in revised January 4, 2019) Key words : cardiac arrest, esophagogastric perforation, tension pneumoperitoneum decompression, successfully improved his circulation. -
Septic, Hypovolemic, Obstructive and Cardiogenic Killers
S.H.O.C.K Septic, Hypovolemic, Obstructive and Cardiogenic Killers Jason Ferguson, BPA, NRP Public Safety Programs Head, CVCC Amherst County DPS, Paramedic Centra One, Flight Paramedic Objectives • Define Shock • Review patho and basic components of life • Identify the types of shock • Identify treatments Shock Defined • “Rude unhinging of the machinery of life”- Samuel Gross, U.S. Trauma Surgeon, 1962 • “A momentary pause in the act of death”- John Warren, U.S. Surgeon, 1895 • Inadequate tissue perfusion Components of Life Blood Flow Right Lungs Heart Left Body Heart Patho Review • Preload • Afterload • Baroreceptors Perfusion Preservation Basic rules of shock management: • Maintain airway • Maintain oxygenation and ventilation • Control bleeding where possible • Maintain circulation • Adequate heart rate and intravascular volume ITLS Cases Case 1 • 11 month old female “not acting right” • Found in crib this am lethargic • Airway patent • Breathing is increased; LS clr • Circulation- weak distal pulses; pale and cool Case 1 • VS: RR 48, HR 140, O2 98%, Cap refill >2 secs • Foul smelling diapers x 1 day • “I must have changed her two dozen times yesterday” • Not eating or drinking much Case 1 • IV established after 4 attempts • Fluid bolus initiated • Transported to ED • Received 2 liters of fluid over next 24 hours Hypovolemic Shock Hemorrhage Diarrhea/Vomiting Hypovolemia Burns Peritonitis Shock Progression Compensated to decompensated • Initial rise in blood pressure due to shunting • Initial narrowing of pulse pressure • Diastolic raised -
Recognizing and Treating Shock in the Prehospital Setting
9/3/2020 Recognizing and Treating Shock in the Prehospital Setting 1 9/3/2020 Special Thanks to Our Sponsor 2 9/3/2020 Your Presenters Dr. Raymond L. Fowler, Dr. Melanie J. Lippmann, MD, FACEP, FAEMS MD FACEP James M. Atkins MD Distinguished Professor Associate Professor of Emergency Medicine of Emergency Medical Services, Brown University Chief of the Division of EMS Alpert Medical School Department of Emergency Medicine Attending Physician University of Texas Rhode Island Hospital and The Miriam Hospital Southwestern Medical Center Providence, RI Dallas, TX 3 9/3/2020 Scenario SHOCK INDEX?? Pulse ÷ Systolic 4 9/3/2020 What is Shock? Shock is a progressive state of cellular hypoperfusion in which insufficient oxygen is available to meet tissue demands It is key to understand that when shock occurs, the body is in distress. The shock response is mounted by the body to attempt to maintain systolic blood pressure and brain perfusion during times of physiologic distress. This shock response can accompany a broad spectrum of clinical conditions that stress the body, ranging from heart attacks, to major infections, to allergic reactions. 5 9/3/2020 Causes of Shock Shock may be caused when oxygen intake, absorption, or delivery fails, or when the cells are unable to take up and use the delivered oxygen to generate sufficient energy to carry out cellular functions. 6 9/3/2020 Causes of Shock Hypovolemic Shock Distributive Shock Inadequate circulating fluid leads A precipitous increase in vascular to a diminished cardiac output, capacity as blood vessels dilate and which results in an inadequate the capillaries leak fluid, translates into delivery of oxygen to the too little peripheral vascular resistance tissues and cells and a decrease in preload, which in turn reduces cardiac output 7 9/3/2020 Causes of Shock Cardiogenic Shock Obstructive Shock The heart is unable to circulate Obstruction to the forward flow of sufficient blood to meet the blood exists in the great vessels metabolic needs of the body. -
Shock and Awe: a Dynamic Approach to Resuscitation
Shock and Awe: A dynamic approach to resuscitation Critical Care Symposium October 28, 2017 Anna Perrello, RPA-C, MPAS Brian Kersten, PharmD, BCCCP, BCPS Disclosures • Brian Kersten o Nothing to disclose • Anna Perrello o Nothing to disclose Objectives • Identify and explain the physiology of various shock states including distributive, cardiogenic, obstructive and hypovolemic. • Discuss advantages and limitations to static and dynamic predictors of volume responsiveness. • Recognize techniques related to visualization of basic structures and medium identification during bedside ultrasonography. • Evaluate treatment options for shock states using dynamic measures for fluid resuscitation Shock • A heterogenous syndrome best defined as circulatory failure o Originates from mismatch between oxygen delivery (DO2) and oxygen consumption (VO2) • Often becomes apparent in setting of arterial hypotension Differentiating Shock Systemic Mixed Wedge Cardiac vascular venous pressure output resistance oxygen Hypovolemic - Hemorrhage ↓ ↓ ↑ ↓ - Dehydration Cardiogenic - Myocardial infarction ↑ ↓ ↑ ↓ - Arrhythmia - Cardiomyopathy Obstructive - Pulmonary embolism ↑↔ ↓ ↑ ↓ - Tension pneumothorax - Cardiac tamponade Distributive - Septic shock - Anaphylaxis ↑↔ ↑ ↓ ↑ - Neurogenic - Myxedema coma - Post-cardiopulmonary bypass Goals of Therapy in Shock • Restore effective tissue perfusion and normalize cellular metabolism by ensuring systemic oxygen delivery by 1. Aggressive and appropriate fluid resuscitation 2. Supporting CO and MAP • Above are titrated to -
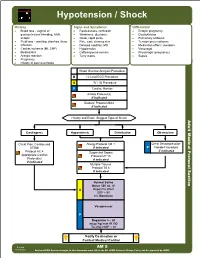
AM 05 Hypotension Shock Protocol Final 2017 Editable.Pdf
Hypotension / Shock History Signs and Symptoms Differential • Blood loss - vaginal or • Restlessness, confusion • Ectopic pregnancy gastrointestinal bleeding, AAA, • Weakness, dizziness • Dysrhythmias ectopic • Weak, rapid pulse • Pulmonary embolus • Fluid loss - vomiting, diarrhea, fever • Pale, cool, clammy skin • Tension pneumothorax • Infection • Delayed capillary refill • Medication effect / overdose • Cardiac ischemia (MI, CHF) • Hypotension • Vasovagal • Medications • Coffee-ground emesis • Physiologic (pregnancy) • Allergic reaction • Tarry stools • Sepsis • Pregnancy • History of poor oral intake Blood Glucose Analysis Procedure B 12 Lead ECG Procedure A IV / IO Procedure P Cardiac Monitor Airway Protocol(s) if indicated Diabetic Protocol AM 2 if indicated History and Exam Suggest Type of Shock Adult Medical Protocol Section Protocol Adult Medical Cardiogenic Hypovolemic Distributive Obstructive Chest Pain: Cardiac and Allergy Protocol AM 1 Chest Decompression- STEMI if indicated P Needle Procedure if indicated Protocol AC 4 Suspected Sepsis Appropriate Cardiac Protocol UP 15 Protocol(s) if indicated if indicated Multiple Trauma Protocol TB 6 if indicated A P Notify Destination or Contact Medical Control Revised AM 5 02/18/2019 Any local EMS System changes to this document must follow the NC OEMS Protocol Change Policy and be approved by OEMS Hypotension / Shock Adult Medical Protocol Section Protocol Adult Medical Pearls • Recommended Exam: Mental Status, Skin, Heart, Lungs, Abdomen, Back, Extremities, Neuro • Hypotension can be defined as a systolic blood pressure of less than 90. This is not always reliable and should be interpreted in context and patients typical BP if known. Shock may be present with a normal blood pressure initially. • Shock often is present with normal vital signs and may develop insidiously. -

Distributive Shock
ASK THE EXPERT h EMERGENCY MEDICINE/CRITICAL CARE h PEER REVIEWED Distributive Shock Garret E. Pachtinger, VMD, DACVECC VETgirl; Veterinary Specialty and Emergency Center Levittown, Pennsylvania Clinical Clues YOU HAVE ASKED ... Distributive shock is generally associ- What is distributive shock, and ated with altered vasomotor tone— notably inappropriate vasodilation (eg, how do I treat it? sepsis, systemic inflammatory response syndrome), excessive vasoconstriction THE EXPERT SAYS ... (eg, following trauma or anaphylaxis), or abnormalities in normal blood flow Shock (ie, inadequate cellular energy (eg, obstructive diseases such as gastric production or the body’s inability to dilatation-volvulus [GDV] or pericardial supply cells and tissues with oxygen and effusion)—resulting in maldistribution nutrients and remove waste products1-3) of blood flow. can cause quick clinical deterioration and requires rapid identification and Patients with septic distributive shock treatment. Distributive shock is a gen- often have hyperemic mucous mem- eral classification for syndromes that branes caused by uncontrolled vasodila- cause massive maldistribution of blood tion from inflammatory mediators and flow (seeReferences , page 96). Anaphy- cytokine release (see References, page lactic, obstructive, and septic shock are 96). Patients with anaphylactic or GDV = gastric dilatation- common forms of distributive shock. obstructive distributive shock show volvulus October 2016 cliniciansbrief.com 93 ASK THE EXPERT h EMERGENCY MEDICINE/CRITICAL CARE h PEER -

Hypovolemic Shock - a Review J
Review Article Hypovolemic shock - A review J. A.Shagana1, M. Dhanraj1, Ashish R. Jain1*, T. Nir osa2 ABSTRACT Shock is described traditionally as tissue hypoxia due to inadequate perfusion which is classified as hypovolemic, cardiogenic, obstructive, and distributive. Hypovolemic shock is an important life-threatening emergency. In hypovolemic shock, there is decreased circulating blood volume due to the loss of intravascular fluid. Hemorrhagic shock is the most common form of hypovolemic shock and must be recognized early which prevent progression, morbidity, and mortality. Hence, this article will discuss about the causes, clinical features, diagnosis, and treatment of hypovolemic shock. KEY WORDS: Blood pressure, Cardiac output, Circulating blood volume, Hypovolemic shock and organ dysfunction INTRODUCTION The systemic vascular resistance (SVR) is typically increased in an effort to compensate for the diminished Shock is defined as the state in which profound and CO and maintain perfusion to vital organs. The early widespread reduction of effective tissue perfusion stage of recognition and intervention will help to leads first to reversible, and then if prolonged, prevent death.[4] to irreversible cellular injury. It is classified as hypovolemic/hemorrhagic shock, cardiogenic ETIOLOGY shock, obstructive shock, and distributive shock.[1]. Hypovolemic shock is defined as the rapid fluid loss or Hypovolemic shock is caused by sudden blood or fluid blood loss which results in multiple organ dysfunction losses within your body. The most common clinical due to inadequate circulating blood volume and causes of hypovolemic shock are hemorrhage, vomiting, perfusion. It is caused by a loss of intravascular diarrhea, severe burns, and excessive sweating.[5] Since fluid which is usually whole blood or plasma. -

Chapter 1 Physiology of Injury and Early Management of Combat Casualties
Physiology of Injury and Early Management of Combat Casualties Chapter 1 PHYSIOLOGY OF INJURY AND EARLY MANAGEMENT OF COMBAT CASUALTIES † ‡ DIEGO VICENTE, MD*; BENJAMIN K. POTTER, MD ; AND ALEXANDER Stojadinovic INTRODUCTION GOLDEN HOUR MANAGEMENT OF COMBAT CASUALTIES AT ROLE 2 AND 3 FACILITIES CARDIOVASCULAR INJURY PULMONARY INJURY NEUROLOGIC INJURY RENAL INJURY HEPATIC INJURY HEMATOLOGIC INJURY ANESTHESIA SUMMARY *Lieutenant, Medical Corps, US Navy; Department of General Surgery; Walter Reed National Military Medical Center, 8901 Wisconsin Avenue, Bethesda, Maryland 20889-5600 †Major, Medical Corps, US Army; Department of Orthopaedic Surgery, Walter Reed National Military Medical Center, 8901 Wisconsin Avenue, Bethesda, Maryland 20889-5600 ‡Colonel, Medical Corps, US Army, Department of General Surgery, Walter Reed National Military Medical Center, 8901 Wisconsin Avenue, Bethesda, Maryland 20889-5600 3 Combat Anesthesia: The First 24 Hours INTRODUCTION The recent conflicts in Iraq and Afghanistan have initiation of emergency medical care in accordance resulted in a marked change in both the injury patterns with Tactical Combat Casualty Care (TCCC) guidelines sustained by wounded personnel and the subsequent in proximity to point of wounding,2,3 tactical damage management of these injuries. Survival of combat control surgery and resuscitation, and rapid transport casualties (CCs) despite severe polytrauma is largely to escalating levels of care with “critical care in the air” attributable to improvements in body armor,1 prompt intensive -
Chapter 32 Diagnosis and Management of Hypotension and Shock in the Intensive Care Unit
Diagnosis and Management of Hypotension and Shock in the Intensive Care Unit Chapter 32 DIAGNOSIS AND MANAGEMENT OF HYPOTENSION AND SHOCK IN THE INTENSIVE CARE UNIT JESSICA BUNIN, MD* INTRODUCTION PATHOPHYSIOLOGY AND CLINICAL PRESENTATION CATEGORIES OF SHOCK GENERAL DIAGNOSTIC APPROACH FOR HYPOTENSION GENERAL PRINCIPLES OF MANAGEMENT OF THE HYPOTENSIVE INTENSIVE CARE UNIT PATIENT MANAGEMENT OF SPECIFIC TYPES OF SHOCK Hypovolemic Shock Cardiogenic Shock Distributive Shock Obstructive Shock SUMMARY *Lieutenant Colonel, Medical Corps, US Army; Chief of the Critical Care Medicine Service, Department of Medicine, Walter Reed National Military Medical Center, 8901 Wisconsin Avenue, Bethesda, Maryland 20889 327 Combat Anesthesia: The First 24 Hours INTRODUCTION Shock is a state of impaired tissue oxygenation and than 30% of blood volume has been lost. Although perfusion that can be caused by decreased oxygen hypotension and shock are not synonymous, the goals delivery, poor tissue perfusion, or impaired oxygen of treatment are the same: to restore the body’s oxygen utilization. Hypotension is a sign of shock and an indi- balance and correct hypoperfusion. This chapter will cator of advanced derangement, requiring immediate address the categories of shock, initial evaluation of a evaluation and management. For example, in hemor- hypotensive patient, general principles of shock man- rhagic shock, hypotension is not present until greater agement, and management for specific causes of shock. PATHOPHYSIOLOGY AND CLINICAL PRESENTATION Shock represents a state of hypoperfusion that vital of organs—the heart and the brain—because of can be the final pathway for a number of conditions. the opening of arteriovenous connections to bypass Hypoperfusion from any cause results in an inflamma- capillary flow.2 tory response. -
Obstructive Shock, P
CHAPTER 10 SHOCK OBJECTIVES KEY TERMS Upon completion of this chapter, the OEC Anaphylactic shock, p. 228 technician will be able to: Anticoagulants, p. 231 10-1 Define shock. Cardiogenic shock, p. 228 10-2 Describe the three primary causes of Distributive shock, p. 228 shock. Fainting, p. 230 10-3 Describe how the body compensates Hypovolemic shock, p. 227 for shock. Neurogenic shock, p. 229 10-4 Define the two stages of shock. Obstructive shock, p. 229 10-5 List the four major types of shock. Perfusion, p. 224 10-6 List the classic signs and symptoms of Peripheral vascular resistance, p. 226 shock. Pulmonary embolism, p. 230 10-7 Describe and demonstrate the Sepsis, p. 228 management of shock. Septic shock, p. 228 Shock, p. 224 Stroke volume, p. 226 Tachycardia, p. 226 Tachypnea, p. 226 HISTORICAL TIMELINE 1964. The NSP adopts the gold cross as its official emblem. © Jones & Bartlett Learning LLC, an Ascend Learning Company. NOT FOR SALE OR DISTRIBUTION. 9781284189599_CH10_223_238.indd 223 4/14/2020 4:37:33 PM 224 Outdoor Emergency Care, Sixth Edition CHAPTER OVERVIEW One of the most serious threats to life is the condition known as shock. Shock is defined as inadequate perfusion or flow of blood to the cells, causing cellular and tissue hypoxia due to reduced oxygen delivery. Perfusion is the circu- lation of blood within an organ or tissue in ade- quate amounts to meet the cells’ current needs for oxygen, nutrients, and waste removal. The body is perfused via the cardiovascular (circulatory) system. Although the potential causes of shock are numerous, shock occurs when one or more com- ponents of the cardiovascular system fail.