Classification and Terminology to Organise Seizures and Epilepsies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Status Epilepticus Clinical Pathway
JOHNS HOPKINS ALL CHILDREN’S HOSPITAL Status Epilepticus Clinical Pathway 1 Johns Hopkins All Children's Hospital Status Epilepticus Clinical Pathway Table of Contents 1. Rationale 2. Background 3. Diagnosis 4. Labs 5. Radiologic Studies 6. General Management 7. Status Epilepticus Pathway 8. Pharmacologic Management 9. Therapeutic Drug Monitoring 10. Inpatient Status Admission Criteria a. Admission Pathway 11. Outcome Measures 12. References Last updated: July 7, 2019 Owners: Danielle Hirsch, MD, Emergency Medicine; Jennifer Avallone, DO, Neurology This pathway is intended as a guide for physicians, physician assistants, nurse practitioners and other healthcare providers. It should be adapted to the care of specific patient based on the patient’s individualized circumstances and the practitioner’s professional judgment. 2 Johns Hopkins All Children's Hospital Status Epilepticus Clinical Pathway Rationale This clinical pathway was developed by a consensus group of JHACH neurologists/epileptologists, emergency physicians, advanced practice providers, hospitalists, intensivists, nurses, and pharmacists to standardize the management of children treated for status epilepticus. The following clinical issues are addressed: ● When to evaluate for status epilepticus ● When to consider admission for further evaluation and treatment of status epilepticus ● When to consult Neurology, Hospitalists, or Critical Care Team for further management of status epilepticus ● When to obtain further neuroimaging for status epilepticus ● What ongoing therapy patients should receive for status epilepticus Background: Status epilepticus (SE) is the most common neurological emergency in children1 and has the potential to cause substantial morbidity and mortality. Incidence among children ranges from 17 to 23 per 100,000 annually.2 Prevalence is highest in pediatric patients from zero to four years of age.3 Ng3 acknowledges the most current definition of SE as a continuous seizure lasting more than five minutes or two or more distinct seizures without regaining awareness in between. -

Cognitive Impairment: Causes, Diagnosis and Treatment
NEUROLOGY - LABORATORY AND CLINICAL RESEARCH DEVELOPMENTS COGNITIVE IMPAIRMENT: CAUSES, DIAGNOSIS AND TREATMENT No part of this digital document may be reproduced, stored in a retrieval system or transmitted in any form or by any means. The publisher has taken reasonable care in the preparation of this digital document, but makes no expressed or implied warranty of any kind and assumes no responsibility for any errors or omissions. No liability is assumed for incidental or consequential damages in connection with or arising out of information contained herein. This digital document is sold with the clear understanding that the publisher is not engaged in rendering legal, medical or any other professional services. NEUROLOGY – LABORATORY AND CLINICAL RESEARCH DEVELOPMENTS SERIES Intracranial Hypertension Stefan Mircea Iencean and Alexandru Vladimir Ciurea 2009 ISBN: 978-1-60741-862-7 (Hardcover Book) Intracranial Hypertension Stefan Mircea Iencean and Alexandru Vladimir Ciurea 2009 ISBN: 978-1-60876-549-2 (Online Book) Cerebral Blood Flow Regulation Nodar P. Mitagvaria and Haim (James) I. Bicher 2009 ISBN: 978-1-60692-163-0 Cerebral Ischemia in Young Adults: Pathogenic and Clinical Perspectives Alessandro Pezzini and Alessandro Padovani (Editors) 2009 ISBN: 978-1-60741-627-2 Dizziness: Vertigo, Disequilibrium and Lightheadedness Agnes Lindqvist and Gjord Nyman (Editors) 2009: ISBN 978-1-60741-847-4 Somatosensory Cortex: Roles, Interventions and Traumas Niels Johnsen and Rolf Agerskov (Editors) 2009. ISBN: 978-1-60741-876-4 Cognitive Impairment: Causes, Diagnosis and Treatment Melanie L. Landow (Editor) 2009. ISBN: 978-1-60876-205-7 NEUROLOGY - LABORATORY AND CLINICAL RESEARCH DEVELOPMENTS COGNITIVE IMPAIRMENT: CAUSES, DIAGNOSIS AND TREATMENT MELANIE L. -

The Effect of Temporal Lobectomy Upon Two Cases of an Unusual Form of Mental Deficiency by D
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.17.4.267 on 1 November 1954. Downloaded from J. Neurol. Neurosurg. Psychiat., 1954, 17, 267. THE EFFECT OF TEMPORAL LOBECTOMY UPON TWO CASES OF AN UNUSUAL FORM OF MENTAL DEFICIENCY BY D. W. LIDDELL and D. W. C. NORTHFIELD From Runwtvell Hospital, Wickford, Essex In 1898, when giving the final particulars and the Case Histories necropsy findings of a case of epilepsy which fully Case l.-M. G., aged 18 years, was referred to exemplified dreamy states and automatisms, Hugh- Runwell Hospital from the Royal Eastern Counties lings Jackson (1931a) wrote that there were post- Hospital because of bouts of violent uncontrollable epileptic actions " of a kind which in a man fully behaviour and repeated attempts to abscond. He was himself would be criminal ". But another 25 years the seventh child of healthy working-class parents. were to elapse before Penfield began his studies on There is no family history of epilepsy. His birth was brain-scars (Penfield and Erickson, 1941) which were normal and he was breast fed for nine months. He guest. Protected by copyright. eventually to secure for surgery a began to walk and talk at about 14 months. As a child place in the be was placid but active, easily managed, and there were treatment of epilepsy. At first the operations were no difficulties in toilet training. restricted to those patients resistant to medical At the age of 7 years he fell out of a tree and was treatment in whom there was conclusive evidence of momentarily unconscious. -

Therapeutic Class Overview Anticonvulsants
Therapeutic Class Overview Anticonvulsants INTRODUCTION Epilepsy is a disease of the brain defined by any of the following (Fisher et al 2014): ○ At least 2 unprovoked (or reflex) seizures occurring > 24 hours apart; ○ 1 unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after 2 unprovoked seizures, occurring over the next 10 years; ○ Diagnosis of an epilepsy syndrome. Types of seizures include generalized seizures, focal (partial) seizures, and status epilepticus (Centers for Disease Control and Prevention [CDC] 2018, Epilepsy Foundation 2016). ○ Generalized seizures affect both sides of the brain and include: . Tonic-clonic (grand mal): begin with stiffening of the limbs, followed by jerking of the limbs and face . Myoclonic: characterized by rapid, brief contractions of body muscles, usually on both sides of the body at the same time . Atonic: characterized by abrupt loss of muscle tone; they are also called drop attacks or akinetic seizures and can result in injury due to falls . Absence (petit mal): characterized by brief lapses of awareness, sometimes with staring, that begin and end abruptly; they are more common in children than adults and may be accompanied by brief myoclonic jerking of the eyelids or facial muscles, a loss of muscle tone, or automatisms. ○ Focal seizures are located in just 1 area of the brain and include: . Simple: affect a small part of the brain; can affect movement, sensations, and emotion, without a loss of consciousness . Complex: affect a larger area of the brain than simple focal seizures and the patient loses awareness; episodes typically begin with a blank stare, followed by chewing movements, picking at or fumbling with clothing, mumbling, and performing repeated unorganized movements or wandering; they may also be called “temporal lobe epilepsy” or “psychomotor epilepsy” . -

The Value of Seizure Semiology in Lateralizing and Localizing Partially Originating Seizures
Review Article The value of seizure semiology in lateralizing and localizing partially originating seizures Mohammed M. Jan, MBChB, FRCP(C). observations help in lateralizing (left versus right) and ABSTRACT localizing (involved brain region) the seizure onset. Therefore, this information is vital not only for seizure Diagnosing epilepsy depends heavily on a detailed, and accurate description of the abnormal transient classification, but more so for identification of surgical neurological manifestations. Observing the candidates. The EEG and neuroimaging, particularly seizures yields important semiologic features that MRI, are needed to identify focal physiological and characterize epilepsy. Video-EEG monitoring allows pathological brain abnormalities.3-5 The development of the identification of important lateralizing (left video-EEG monitoring has allowed careful correlation of versus right), and localizing (involved brain region) semiologic features with simultaneous EEG recordings.6 semiologic features. This information is vital for As a result, clinical semiology gained greater reliability identifying the seizure origin for possible surgical in diagnosing specific seizure types and localizing their interventions. The aim of this review is to present a onset.7 The aim of this review is to present a summary summary of important semiologic characteristics of various seizures that are important for accurate seizure of important semiologic characteristics of various lateralization and localization. This would most seizures that are needed for accurate lateralization likely help during reviewing video-EEG recorded and localization. This would most likely help during seizures of intractable patients for possible epilepsy reviewing video-EEG recorded seizures of intractable surgery. Semiologic features of partial and secondarily patients for possible epilepsy surgery. generalized seizures can be grouped into one of 4 History taking. -
Epilepsy and Communication
fasic England Gloss ry Epilepsy and communication Epilepsy is a chronic disorder of the brain • Temporal Lobe epilepsy characterised by recurrent seizures, which affects • Dravet syndrome people worldwide (WHO, 2016). The World Health Organisation deKnes a seizure as a transient loss of There are a range of communication difficulties function of all or part of the brain due to excessive associated with epilepsy. For some people, electrical discharges in a group of brain cells. Physical, communication difficulties can become more sensory or other functions can be temporarily lost. pronounced at times immediately before, during or after seizure activity. Epilepsy affects 1 in 177 young people under the age of 25 so there are around 112,000 young people with Communication difficulties may include: epilepsy in the UK (Joint Epilepsy Council, 2011). In 75% • Comprehension difficulties: Children may Knd it of people, seizures are well controlled with medication hard to understand what others are saying to but 25% continue to have seizures despite treatment. them or what is expected of them, and may struggle to understand environmental cues, daily Epilepsy can be linked with learning, behavioural and routines or activity sequences. speech and language difficulties. This is increasingly • Attention and listening difficulties: Children recognised and the risks are greater if epilepsy occurs may have difficulties in attending to spoken before 2 years of age. Parkinson (1994) found that language, or to an activity. from a small study of children referred for assessment of their epilepsy, 40% had undiagnosed language • Expressive difficulties: It may be hard for impairment of varying degrees of severity. -

14582 IBE Newsletter 2003
International Bureau for Epilepsy Annual Report 2003 Setting the Standard From Our Vision IBE has a vision of the world where everywhere ignorance and fear about epilepsy are replaced by understanding and care. Our Mission IBE exists to improve the social condition and quality of life of people with epilepsy and those who care for them. Our Goals • ORGANISATION To provide an international umbrella organisation for national epilepsy organisations whose primary purpose is to improve the social condition and quality of life of people with epilepsy and those who care for them. • SUPPORT To provide a strong global network to support the development of new Chapters, to support existing Chapters to develop to their fullest potential and to encourage co-operation and contact between Chapters. • COMMUNICATION To promote the facts about epilepsy and to communicate IBE’s vision, mission and messages to the widest possible audience. • EDUCATION To increase understanding and knowledge of epilepsy. • REPRESENTATION To provide an international and global platform for the representation of epilepsy. 2 International Bureau for Epilepsy Foreward During my fifteen years working, first in the British Parliament and Government and now in the European Parliament, I have seen and welcomed an ever-increasing awareness of the importance and benefits of strong partnerships. Networks and alliances are more than just “buzz words” – they are proven methods of achieving desired goals. They may not be easy to achieve, but, once in place, they make it simpler for patients, carers, professionals and academics to explain health needs and options for action and they make it easier for policy-makers to listen and to understand what is needed. -

Prognostic Utility of Hypsarrhythmia Scoring in Children with West
Clinical Neurology and Neurosurgery 184 (2019) 105402 Contents lists available at ScienceDirect Clinical Neurology and Neurosurgery journal homepage: www.elsevier.com/locate/clineuro Prognostic utility of hypsarrhythmia scoring in children with West syndrome T after ketogenic diet ⁎ Yunjian Zhang1, Lifei Yu1, Yuanfeng Zhou, Linmei Zhang, Yi Wang, Shuizhen Zhou Department of Pediatric Neurology, Children’s Hospital of Fudan University, China ARTICLE INFO ABSTRACT Keywords: Objective: The aim of this study was to evaluate the clinical efficacy and electroencephalographic (EEG) changes West syndrome of West syndrome after ketogenic diet (KD) therapy and to explore the correlation of EEG features and clinical Ketogenic diet efficacy. EEG Patients and methods: We retrospectively studied 39 patients with West syndrome who accepted KD therapy from Hypsarrhythmia May 2011 to October 2017. Outcomes including clinical efficacy and EEG features with hypsarrhythmia severity scores were analyzed. Results: After 3 months of treatment, 20 patients (51.3%) had ≥50% seizure reduction, including 4 patients (10.3%) who became seizure-free. After 6 months of treatment, 4 patients remained seizure free, 12 (30.8%) had 90–99% seizure reduction, 8 (20.5%) had a reduction of 50–89%, and 15 (38.5%) had < 50% reduction. Hypsarrhythmia scores were significantly decreased at 3 months of KD. They were associated with seizure outcomes at 6 months independent of gender, the course of disease and etiologies. Patients with a hypsar- rhythmia score ≥8 at 3 months of therapy may not be benefited from KD. Conclusion: Our findings suggest a potential benefit of KD for patients with drug-resistant West syndrome. Early change of EEG after KD may be a predictor of a patient’s response to the therapy. -
Best Practice Guidelines for Training
Best practice guidelines for training professional carers in the administration of Buccal (Oromucosal) Midazolam for the treatment of prolonged and / or clusters of epileptic seizures in the community Safe & Effective | Kind & Caring | Exceeding Expectation Epilepsy Nurses Association (ESNA) June 2019 1. Foreword One of the most important components of epilepsy care is the pre-hospital community management of prolonged or repeated seizures, which, if untreated, can increase the risk of status epilepticus. Convulsive status epilepticus is a medical emergency requiring admission to hospital and has a mortality rate of up to 20 per cent. Effective management of seizures in the community in people at high risk of status epilepticus could significantly reduce mortality, morbidity and emergency health care utilisation. The Joint Epilepsy Council issued guidance until it was disbanded in 2015, leaving a vacuum in the review and update of clinical guidelines. Unfortunately, the clinical processes ensuring the safety and consistency of buccal midazolam usage demonstrates considerable heterogeneity. There are no current guidelines, standards or pathways to ensure the safety of all involved in the process i.e. patient, carer or professional. ESNA is an organisation principally formed by nurses with an interest in epilepsy. Most ESNA members support or complete training for buccal midazolam to ensure core competencies are up to date and patient safety is protected. ESNA is joined by the International League Against Epilepsy (British Chapter) and the Royal College of Psychiatrists (ID Faculty) as the other principal specialist clinical stakeholders with an interest to ensure governance in this complex care area is addressed robustly. ESNA has collaborated with the ILAE and the Royal College of Psychiatrists to produce updated buccal midazolam guidance. -

A Rare Case of Immune Reconstitution Inflammatory Syndrome Development in an Immunocompromised Patient with Progressive Multifocal Leukoencephalopathy And
Hindawi Publishing Corporation Case Reports in Neurological Medicine Volume 2013, Article ID 460701, 5 pages http://dx.doi.org/10.1155/2013/460701 Case Report A Rare Case of Immune Reconstitution Inflammatory Syndrome Development in an Immunocompromised Patient with Progressive Multifocal Leukoencephalopathy and Multicentric Castleman’s Disease Mohankumar Kurukumbi,1 Sheldon Steiner,1,2 Shariff Dunlap,1 Sherita Chapman,3 Noha Solieman,1 and Annapurni Jayam-Trouth1 1 Department of Neurology, Howard University Hospital, 2041 Georgia Avenue, Washington, DC 20060, USA 2 Department of Neurology, Howard University College of Medicine, Washington, DC 20060, USA 3 Department of Neurology, University of Virginia, Charlottesville, VA 22908, USA Correspondence should be addressed to Mohankumar Kurukumbi; [email protected] Received 27 June 2013; Accepted 17 July 2013 AcademicEditors:T.K.Banerjee,J.L.Gonzalez-Guti´ errez,´ R. Hashimoto, J. C. Kattah, and Y. Wakabayashi Copyright © 2013 Mohankumar Kurukumbi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Immune reconstitution inflammatory syndrome (IRIS) development in HIV with preexistent progressive multifocal leukoen- cephalopathy (PML) has been extensively studied. PML-IRIS typically manifests clinically as new or worsening neurologic symptoms in conjunction with enlarging CNS lesions and occurs in approximately 10–20 percent of HIV-infected patients with PML who begin HAART. Likewise, Multicentric Castleman’s Disease (MCD), a rare malignant lymphoproliferative disorder, has a strong and well-known association with HIV. Our case provides a rare instance of PML-IRIS in combination with MCD in an HIV-positive individual. -

Epilepsy Syndromes E9 (1)
EPILEPSY SYNDROMES E9 (1) Epilepsy Syndromes Last updated: September 9, 2021 CLASSIFICATION .......................................................................................................................................... 2 LOCALIZATION-RELATED (FOCAL) EPILEPSY SYNDROMES ........................................................................ 3 TEMPORAL LOBE EPILEPSY (TLE) ............................................................................................................... 3 Epidemiology ......................................................................................................................................... 3 Etiology, Pathology ................................................................................................................................ 3 Clinical Features ..................................................................................................................................... 7 Diagnosis ................................................................................................................................................ 8 Treatment ............................................................................................................................................. 15 EXTRATEMPORAL NEOCORTICAL EPILEPSY ............................................................................................... 16 Etiology ................................................................................................................................................ 16 -
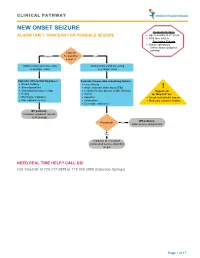
Seizure, New Onset
CLINICAL PATHWAY NEW ONSET SEIZURE Inclusion Criteria ALGORITHM 1. CONCERN FOR POSSIBLE SEIZURE • Age 6 months to 21 years • First-time seizure Exclusion Criteria • Status epilepticus (refer to status epilepticus pathway) Concern Unsure for possible Yes seizure? Obtain history and screening Obtain history and screening neurologic exam neurologic exam Consider differential diagnoses: Evaluate for possible provoking factors: • Breath holding • Fever/illness • Stereotypies/tics • Acute traumatic brain injury (TBI) ! • Vasovagal/syncope/vertigo • Central nervous system (CNS) infection Urgent call • Reflux • Tumor to ‘OneCall’ for: • Electrolyte imbalance • Ingestion • Suspected infantile spasm • Non epileptic seizure • Intoxication • Medically complex children • Electrolyte imbalance Off pathway: Consider outpatient referral to Neurology Off pathway: Provoked? Yes Address provoking factors No Continue to new onset unprovoked seizure algorithm on p.2 NEED REAL TIME HELP? CALL US! Call ‘OneCall’ at 720-777-3999 or 719-305-3999 (Colorado Springs) Page 1 of 17 CLINICAL PATHWAY ALGORITHM 2. NEW ONSET UNPROVOKED SEIZURE Inclusion Criteria • Age 6 months to 21 years New onset unprovoked • First-time unprovoked seizure seizure • Newly recognized seizure or epilepsy syndrome Exclusion Criteria • Provoked seizure: any seizure as a symptom of fever/illness, acute traumatic brain injury (TBI), Has central nervous system (CNS) infection, tumor, patient returned ingestion, intoxication, or electrolyte imbalance Consult inpatient • to baseline within No