Dignity in Choice: a Terminally Ill Patient's Right to Choose Cody Bauer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Necessary Right of Choice for Physician-Assisted Suicide
Student Publications Student Scholarship Fall 2017 The ecesN sary Right of Choice for Physician- Assisted Suicide Kerry E. Ullman Gettysburg College Follow this and additional works at: https://cupola.gettysburg.edu/student_scholarship Part of the Applied Ethics Commons, and the Ethics in Religion Commons Share feedback about the accessibility of this item. Ullman, Kerry E., "The eN cessary Right of Choice for Physician-Assisted Suicide" (2017). Student Publications. 574. https://cupola.gettysburg.edu/student_scholarship/574 This open access student research paper is brought to you by The uC pola: Scholarship at Gettysburg College. It has been accepted for inclusion by an authorized administrator of The uC pola. For more information, please contact [email protected]. The ecesN sary Right of Choice for Physician-Assisted Suicide Abstract Research-based paper on the importance of the right for terminally ill patients facing a painful death to be able to choose how they end their life Keywords Assisted-Suicide, Maynard, Kevorkian, Terminally-ill Disciplines Applied Ethics | Ethics in Religion Comments Written for FYS 150: Death and the Meaning of Life. Creative Commons License Creative ThiCommons works is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This student research paper is available at The uC pola: Scholarship at Gettysburg College: https://cupola.gettysburg.edu/ student_scholarship/574 Ullman 1 Kerry Ullman Professor Myers, Ph.D. Death and the Meaning of Life - FYS 30 November 2017 Assisted Suicide The Necessary Right of Choice for Physician-Assisted Suicide Imagine being told you have less than six months left to live. On top of that horrific news, you experience excruciating pain every single day that is far more atrocious than anything you could have possibly imagined. -
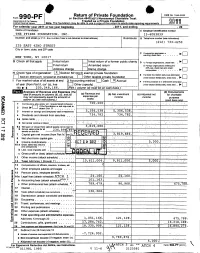
Return of Private Foundation CT' 10 201Z '
Return of Private Foundation OMB No 1545-0052 Form 990 -PF or Section 4947(a)(1) Nonexempt Charitable Trust Department of the Treasury Treated as a Private Foundation Internal Revenue Service Note. The foundation may be able to use a copy of this return to satisfy state reporting requirem M11 For calendar year 20 11 or tax year beainnina . 2011. and ending . 20 Name of foundation A Employer Identification number THE PFIZER FOUNDATION, INC. 13-6083839 Number and street (or P 0 box number If mail is not delivered to street address ) Room/suite B Telephone number (see instructions) (212) 733-4250 235 EAST 42ND STREET City or town, state, and ZIP code q C If exemption application is ► pending, check here • • • • • . NEW YORK, NY 10017 G Check all that apply Initial return Initial return of a former public charity D q 1 . Foreign organizations , check here . ► Final return Amended return 2. Foreign organizations meeting the 85% test, check here and attach Address chang e Name change computation . 10. H Check type of organization' X Section 501( exempt private foundation E If private foundation status was terminated Section 4947 ( a)( 1 ) nonexem pt charitable trust Other taxable p rivate foundation q 19 under section 507(b )( 1)(A) , check here . ► Fair market value of all assets at end J Accounting method Cash X Accrual F If the foundation is in a60-month termination of year (from Part Il, col (c), line Other ( specify ) ---- -- ------ ---------- under section 507(b)(1)(B),check here , q 205, 8, 166. 16) ► $ 04 (Part 1, column (d) must be on cash basis) Analysis of Revenue and Expenses (The (d) Disbursements total of amounts in columns (b), (c), and (d) (a) Revenue and (b) Net investment (c) Adjusted net for charitable may not necessanly equal the amounts in expenses per income income Y books purposes C^7 column (a) (see instructions) .) (cash basis only) I Contribution s odt s, grants etc. -

Download Download
KLIM, AN INSTITUTIONAL RIGHT TO DIE, VOICES IN BIOETHICS, VOL. 2 (2016) An Institutional Right to Die: Neither Coercive nor Immoral Casimir Klim Keywords: right to die, health law, end of life INTRODUCTION The question of whether or not the terminally ill should be granted an institutional right to die rose to the forefront of the national consciousness recently, due in large part to the efforts of the late Brittany Maynard. Diagnosed with untreatable brain cancer, Maynard decided to end her life last fall in Oregon, where state law permits physician-assisted suicide.1 In an editorial for CNN, Maynard wrote: “having this choice at the end of my life has … given me a sense of peace during a tumultuous time that otherwise would be dominated by fear, uncertainty, and pain” (“My right to death with dignity at 29”). Having the option to end her life gave Maynard back her sense of agency and allowed her to die on her own terms. ANALYSIS Laws like Oregon’s Death with Dignity Act are not without their critics, however. Prominent among them is philosopher J. David Velleman, who makes a case against these laws in his essay “Against the Right to Die.” Velleman challenges those—like Maynard—who claim that state-sanctioned assisted suicide can preserve the dignity of the terminally ill. He claims that dignity and autonomy are intertwined in such a way that someone lacking dignity also necessarily lacks the ability to rationally choose suicide. Velleman also argues that the presence of an institutional right to die places an undue pressure on the terminally ill to exercise such a right. -
FENA Conversation with Fran
FINAL EXIT NETWORK VOL 18 • NO 1 WINTER, JAN/FEB 2019 CONTENTS TTHEHE TIME TO IMPROVE OREGON-STYLE LAWS? .........3 GOODGOOD DEMENTIA ADVANCE DEATHDEATH DIRECTIVES ...........................5 FISCAL YEAR REPORT ............9 SOCIETYSOCIETY AMERICANS ACCEPT FEN EUTHANASIA ..................... 11 A Conversation With Fran By Michael James, FEN Life Member enior Guide Fran Schindler’s voice was raspy after five days of protesting in Washington, DC, but this remarkable 79- Q: year-old’sS enthusiasm for FEN and life in general was loud and clear. “The privilege of someone being What’s going to willing to have me with them when they die, when I happen to you? only just sit with them, is the most meaningful thing I have ever done.” In the late 1980s, Fran faced a series of daunt- ing issues: a brain tumor, divorce, and mysterious A. symptoms which mimicked ALS. She acknowledg- es she became obsessed with finding ways to kill I will get dead. herself during those dark days. Eventually she heard Faye Girsh lecture about FEN. She quickly signed up for training and got her FEN membership card in November 2006. Twelve years later she estimates FRAN continued on page 2 Renew your membership online: www.finalexitnetwork.org FRAN continued from page 1 she’s been present for over 70 individuals who have taken their lives using FEN protocol. “At the FEN training class I discovered a major benefit of being a “Start doing FEN member. I looked at the trainers and my fellow classmates—people who didn’t know me—and real- what you want ized that if I needed them they would be there for me. -

AMWA Centennial Meeting Poster and Oral Presentation Abstracts
AMWA Centennial Meeting Poster and Oral Presentation Abstracts Compiled by: Kimberly Seidel and Carey Wickham Table of Contents: ATTENDING PHYSICIAN POSTER PRESENTATIONS: 1 RESIDENT PHYSICIAN POSTER PRESENTATIONS: 7 RESIDENT PHYSICIAN ORAL PRESENTATIONS: 11 STUDENT POSTER PRESENTATIONS: 14 Attending Physician Poster Presentations: A Patient's Right to Die-- What other options do we have? Author: Mei-Ean Yeow Institution: Rush University Medical Center Presenter: Mei-Ean Yeow, [email protected] Poster number: 1 A patient’s right to die/physician assisted suicide remains a controversial topic both in the medical field and in the community at large, especially with recent high profile cases such as the Brittany Maynard case. Hospice & Palliative care physicians not infrequently face requests for hastened deaths from their patients. We describe two cases and discuss the ethical, legal and moral challenges, along with alternative options that can provide comfort and dignity at the end of life. Cases: Ms A was a 76 yr old female on hospice care with lung cancer which had metastasized to bone and throat. Along with worsening pain, she also felt that she was choking on her secretions. Despite aggressive medical management, she continued to be in distress and pain and asked us to give her medications to help her die. After multiple meetings, a decision was made to pursue palliative sedation (PS). Mr S was a 71 yr old male with renal cell carcinoma, metastasized to brain, lung and liver. He was a retired epidemiologist, who valued his intellect and clear thinking highly. His functional status begun to decline and he was also having problems with word-finding. -

NOW Is Time to Address Dementia
The Human Right To A Death With Dignity Special Edition FEN responds in hour of crises VOL 19 • NO 2 SPRING 2020 NOW is time to address dementia Final Exit Network has created surrounding the explosion in a new Advance Directive designed Alzheimer’s and other forms of to prevent dying people from being dementia, because no state that offers force fed against their wishes – Medical Aid in Dying accommodates even if suffering from dementia. patients who are not “of sound mind” What’s more, FEN will go to court when it is time to receive assistance. in an effort to set a legal precedent Now there is a second, more ensuring that VSED (Voluntarily pressing crisis: COVID-19. The Stopping Eating and Drinking) is specter of a ventilator is now reality always available to those who sign for many of us who were already the Supplemental Advance Directive concerned about how we would die. for Dementia Care. FEN is stepping up in this time This document, and the drive to of dual crises, and this edition of the make it legally binding, has been magazine is keenly focused on on our agenda for some time. We what we all need to know. recognized the growing crisis – Brian Ruder, FEN President Life (and death) in the time of COVID-19 By Lowrey Brown words apply equally well when applied to laws FEN Client Services Director and social customs that would rob so many of The title is hardly original wordplay at the right to shape how their life stories end. -

State Court Rewriting of Overbroad Statutes
University of Pennsylvania Carey Law School Penn Law: Legal Scholarship Repository Prize Winning Papers Student Papers 2017 State Court Rewriting of Overbroad Statutes David Schneyer Follow this and additional works at: https://scholarship.law.upenn.edu/prize_papers Repository Citation Schneyer, David, "State Court Rewriting of Overbroad Statutes" (2017). Prize Winning Papers. 11. https://scholarship.law.upenn.edu/prize_papers/11 This Prize Paper is brought to you for free and open access by the Student Papers at Penn Law: Legal Scholarship Repository. It has been accepted for inclusion in Prize Winning Papers by an authorized administrator of Penn Law: Legal Scholarship Repository. For more information, please contact [email protected]. David Schneyer First Amendment Seminar Professor Seth Kreimer State Court Rewriting of Overbroad Statutes I. Introduction: Overbreadth and the Problem of Federalism ............................................. 2 II. State Court Narrowing of Overbroad Statutes: a 50-State Survey .............................. 7 A. States that Rewrite Overbroad Statutes .......................................................................... 10 1. California ........................................................................................................................ 11 2. Massachusetts ................................................................................................................. 16 3. Other States that Rewrite Overbroad Statutes. .............................................................. -

QUIZ: Are You Ready to Die?
QUIZ: Are you ready to die? 1. Do you have an irreversible physical illness or condition -- one that will not get better? __Yes __No 2. Do you suffer unbearably most of the time? __Yes __No 3. Will you lose any semblance of who you are as a person as your illness progresses? __Yes __No 4. If you didn’t have this illness, would you want to live? __Yes __No 5. Have you explored all alternatives to ending your life, for example, further treatment, comfort care? __Yes __No 6. Have you discussed your thoughts about dying with those closest to you? __Yes __No 7. Are people you love and respect sympathetic with your wishes? __Yes __No 8. Are your ideas about dying now consistent with your religious and ethical values? __Yes __No 9. Do you have a plan that follows authoritative information from respected sources to accomplish a peaceful and dignified death? __Yes __No 10. Do you have a plan that will not jeopardize or traumatize anyone else? __Yes __No 11. Have you discussed with an authoritative source what other choices you have to end your life besides the plan you have? __Yes __No 12. Will someone be with you so you do not die alone? __Yes __No 13. Have you explored the Final Exit Network program? __Yes __No __________________ If you have answered Yes to all 13 questions you might be a candidate for an assisted, hastened death. If you have answered No to any of these questions, you should not act to hasten your death until you have explored the possibilities further. -

Criteria for Physician Assisted Suicide and Politically, Because It Raises Many Issues
Dilemmas of Physician Assisted Suicide An International Perspective Joy Chang Finance, Real Estate, & Law Philosophy Mentor: Dr. David Adams Kellogg Honors College Capstone Project Abstract Switzerland Netherland The topic of the permissibility of physician assisted suicide PAS: Legal since Jan. 1, 1942 PAS: Legal since Feb. 19, 2008 (PAS) has always been a highly debated topic, socially, morally, “Whoever, from selfish motives , induces Criteria for Physician Assisted Suicide and politically, because it raises many issues. These include the another to commit suicide or assists him therein Unbearable Suffering shall be punished, if the suicide was successful sanctity of life and the goals of medicine. Some worry that Both the suffering and the desire to die were or attempted, by confinement in a penitentiary enduring legalizing physician assisted suicide will desensitize physicians for not more than five years or by The decision to die was voluntary to human suffering and lead down a slippery slope to killing of imprisonment.” The person was award and had considered the ill, weak, and disabled, among others. Source: Article 115 of the Penal Code of Switzerland. valuable alternatives Legally, physician assisted suicide is currently allowed in five No alternative to improve the situation were states: Oregon, Montana, Washington, New Mexico, and available The person’s death did not cause unnecessary Vermont. Assisted suicide has been legalized in the Netherlands suffering to others and in Switzerland. Since Oregon was the first state where PAS was legalized, I will discuss Oregon’s requirement for PAS and compare it with the current standard of assisted suicide in other countries. -

Death and Dignity Michael Gardner Brigham Young University, [email protected]
Brigham Young University Prelaw Review Volume 31 Article 4 4-2017 Death and Dignity Michael Gardner Brigham Young University, [email protected] Follow this and additional works at: https://scholarsarchive.byu.edu/byuplr Part of the Law Commons, and the Social and Behavioral Sciences Commons BYU ScholarsArchive Citation Gardner, Michael (2017) "Death and Dignity," Brigham Young University Prelaw Review: Vol. 31 , Article 4. Available at: https://scholarsarchive.byu.edu/byuplr/vol31/iss1/4 This Article is brought to you for free and open access by the All Journals at BYU ScholarsArchive. It has been accepted for inclusion in Brigham Young University Prelaw Review by an authorized editor of BYU ScholarsArchive. For more information, please contact [email protected], [email protected]. deaTh and digniTy Kelton Gardner1 n April 2014, Brittany Maynard, a 29-year-old resident of Ana- heim, California and recent graduate student of the University Iof California, was diagnosed with grade four astrocytoma—a form of brain cancer—and was given a prognosis of six months to live. Brittany and her family moved to Oregon, one of only fve states at the time that had legalized physician-assisted suicide. As the quality of her life decreased dramatically, Brittany decided she wanted a physician-assisted suicide. This process would consist of taking prescribed pills (known as barbiturates) in the comfort of her own home at the time of her own choosing. On November 1, 2014, Brittany ended her life as she intended. In an article she posted on CNN’s website, Brittany expressed her gratitude for laws allowing physician-assisted suicide in circumstances of imminent death and tremendous pain. -

World Federation Right to Die Societies 2012
Notes from the World Federation of Right to Die Societies 17th World Congress Biennial Conference - June 2012 Zurich, Switzerland by Faye Girsh Day 1 I got here yesterday in the cold rain. Staying at the Swissotel, a big, modern building near the train station. Cold as it was it was warming to start bumping into old friends from Europe, Canada and Australia. This is an expensive city! Ted Goodwin, the current WF Prez, and I went across the street and had plain spaghetti, nothing else, for $10. The currency is colorful and beautiful but hard to hold on to. Today about 15 of us had signed up for a tour led by the conference organizer, Bernhard Sutter, VP of Exit Swiss Deutsche here in Zurich. Besides being young, energetic and delightful he has put together an amazingly wide array of speakers demonstrating just how broad the World Federation is. Tomorrow I’ll report on the actual program so you'll see what I mean. This morning he led us – on trains and trams – to the charming, rustic, vibrant old town, which unfortunately is pretty far from our hotel. Among other things we saw a church with Chagall windows. The weather was good, thank the Swiss gods. Around noon we went to a river boat where we sat down to an elegant lunch while cruising down the river. Both banks were right out of a post card with their pretty homes, picturesque steeples, and lots of green. It did rain a few drops while we wined and dined but was OK for some of us who returned by tram to the hotel. -

How Relevant Is the Hippocratic Oath in Guiding Physicians' Views on Physician-Assisted Suicide
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Honors Theses, University of Nebraska-Lincoln Honors Program Spring 2020 How Relevant is the Hippocratic Oath in Guiding Physicians' Views on Physician-assisted Suicide Megan Neal University of Nebraska - Lincoln Follow this and additional works at: https://digitalcommons.unl.edu/honorstheses Part of the Gerontology Commons, and the Medicine and Health Commons Neal, Megan, "How Relevant is the Hippocratic Oath in Guiding Physicians' Views on Physician-assisted Suicide" (2020). Honors Theses, University of Nebraska-Lincoln. 210. https://digitalcommons.unl.edu/honorstheses/210 This Thesis is brought to you for free and open access by the Honors Program at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Honors Theses, University of Nebraska-Lincoln by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Running head: HOW RELEVANT IS THE HIPPOCRATIC OATH HOW RELEVANT IS THE HIPPOCRATIC OATH IN GUIDING PHYSICIANS’ VIEWS ON PHYSICIAN-ASSISTED SUICIDE An Undergraduate Honors Thesis Submitted in Partial fulfillment of University Honors Program Requirements University of Nebraska-Lincoln By Megan Neal, BS Biological Sciences College of Arts and Sciences 2020 Faculty Mentor: Julie Masters, PhD, Gerontology HOW RELEVANT IS THE HIPPOCRATIC OATH 2 Table of Contents Dedication…………………………………………………………………………3 Abstract……………………………………………………………………………4 Literature Review…………………………………………………………………5-20 Method……………………………………………………………………………21 Results……………………………………………………………………………22-25 Discussion………………………………………………………………………...26-31 References………………………………………………………………………..31-37 Appendices……………………………………………………………………….37-45 HOW RELEVANT IS THE HIPPOCRATIC OATH 3 Dedication First, I would like to thank all the physicians that participated in the interviews for this study. Their dedication of time and deep consideration of the topics are what made this study possible.