Bite Me! an Overview of Australian Snakebite Envenomation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Socio-Ecology of Two Species of Australian Native Rodent—Notomys
The socio-ecology of two species of Australian native rodent— Notomys mitchelli and Notomys alexis Clare Bradley PhD candidate Environmental Biology School of Earth and Environmental Sciences University of Adelaide November 2008 Chapter One—Introduction 1. Introduction 1.1. Mammalian social systems Many mammal species live in social groups that can consist of related individuals, family groups, or unrelated animals (Alexander 1974). Animals aggregate in order to better survive and reproduce in their particular environment, possibly gaining from shared parental care, cooperative foraging, or a reduction in predation through increased vigilance (Berger & Stevens 1996; Clutton-Brock 1989a; Hughes 1998; Johnson et al. 2002; Kleiman 1977; see also Carr & Macdonald 1986). The basic determinant of social organisation in animals is the mating system, and mating systems of mammals are generally thought to be governed by the resources available in the habitat, since the distribution of resources determines the spatial distribution of females and this, in turn, determines the distribution of males (Clutton-Brock 1989a; Emlen & Oring 1977; Shier & Randall 2004; Trivers 1972; Wiens 1976; Wittenberger 1980). In very stable or predictable environments, where resources are uniformly distributed in space and time, females can be widely dispersed and monogamous mating systems are thought to be most likely (Emlen & Oring 1977; Keverne 1985; Kleiman 1977; Komers & Brotherton 1997; Reichard 2003). However, increasingly patchy resource distribution acts to ‘clump’ female distribution in areas of higher quality and promote polygynous systems (Clutton-Brock 1989a; Johnson et al. 2002; Orians 1969; Reynolds 1996). In such environments, a successful breeding strategy for a male is one where he can gain access to multiple females through controlling, in some way, the resources that govern the females’ dispersion (Greenwood 1980; Perrin & Mazalov 2000; The socio-ecology of two species of Australian native rodent—N. -

6. Terrestrial Fauna
Moura Link - Aldoga Rail Project Queensland Rail Environmental Impact Statement Terrestrial fauna 6. Terrestrial fauna This section describes the existing environment, potential impacts and mitigation measures for the Project in terms of the terrestrial fauna values. The assessment has been based on a review of existing information and the outcomes of supporting field investigations. It should be noted that the information regarding legislation is current at the time of writing this section but may be subject to change in the future. Legislation requirements covered in the EIS have been cited from: • Environment Protection and Biodiversity Conservation Act 1999 (EPBC Act) • Nature Conservation Act 1992 (NC Act) • Nature Conservation (Wildlife) Regulation 2006 (NC Regulation) • Vegetation Management Act 1999 (VM Act) • Land Protection (Pest and Stock Route Management) Act 2002 • Land Protection (Pest and Stock Route Management) Regulation 2003 The currency of such information will be checked during the detailed design phase of the Project and prior to commencement of construction activities within the project area. Currently the designation of threatened species under the NC Act and NC Regulation is being reviewed to conform with international classification and as such species listed as rare will be reassessed and classified as either least concern, vulnerable, near threatened, endangered or critically endangered. 6.1 Existing environment 6.1.1 Methodology In March 2007, Connell Hatch prepared a desktop ecological assessment to support the development of an Initial Advice Statement, EPBC Referral for determination of the Project’s controlled action status under the EPBC Act and ultimately assist in the EIS process. The Project was deemed a not controlled action under Section 75 of the EPBC Act. -

Venemous Snakes
WASAH WESTERN AUSTRALIAN SOCIETY of AMATEUR HERPETOLOGISTS (Inc) K E E P I N G A D V I C E S H E E T Venomous Snakes Southern Death Adder (Acanthophis Southern Death antarcticus) – Maximum length 100 cm. Adder Category 5. Desert Death Adder (Acanthophis pyrrhus) – Acanthophis antarcticus Maximum length 75 cm. Category 5. Pilbara Death Adder (Acanthophis wellsi) – Maximum length 70 cm. Category 5. Western Tiger Snake (Notechis scutatus) - Maximum length 160 cm. Category 5. Mulga Snake (Pseudechis australis) – Maximum length 300 cm. Category 5. Spotted Mulga Snake (Pseudechis butleri) – Maximum length 180 cm. Category 5. Dugite (Pseudonaja affinis affinis) – Maximum Desert Death Adder length 180 cm. Category 5. Acanthophis pyrrhus Gwardar (Pseudonaja nuchalis) – Maximum length 100 cm. Category 5. NOTE: All species listed here are dangerously venomous and are listed as Category 5. Only the experienced herpetoculturalist should consider keeping any of them. One must be over 18 years of age to hold a category 5 license. Maintaining a large elapid carries with 1 it a considerable responsibility. Unless you are Pilbara Death Adder confident that you can comply with all your obligations and licence requirements when Acanthophis wellsi keeping dangerous animals, then look to obtaining a non-venomous species instead. NATURAL HABITS: Venomous snakes occur in a wide variety of habitats and, apart from death adders, are highly mobile. All species are active day and night. HOUSING: In all species listed except death adders, one adult (to 150 cm total length) can be kept indoors in a lockable, top-ventilated, all glass or glass-fronted wooden vivarium of Western Tiger Snake at least 90 x 45 cm floor area. -

Death Adders {Acanthophis Laevis Complex) from the Island of Ambon
ZOBODAT - www.zobodat.at Zoologisch-Botanische Datenbank/Zoological-Botanical Database Digitale Literatur/Digital Literature Zeitschrift/Journal: Herpetozoa Jahr/Year: 2006 Band/Volume: 19_1_2 Autor(en)/Author(s): Kuch Ulrich, McGuire Jimmy A., Yuwono Frank Bambang Artikel/Article: Death adders (Acanthophis laevis complex) from the island of Ambon (Maluku, Indonesia) 81-82 ©Österreichische Gesellschaft für Herpetologie e.V., Wien, Austria, download unter www.biologiezentrum.at SHORT NOTE HERPETOZOA 19(1/2) Wien, 30. Juli 2006 SHORT NOTE 81 O. & PINTO, I. & BRUFORD, M. W. & JORDAN, W. C. & NICHOLS, R. A. (2002): The double origin of Iberian peninsular chameleons.- Biological Journal of the Linnean Society, London; 75: 1-7. PINHO, C. & FER- RAND, N. & HARRIS, D. J. (2006): Reexamination of the Iberian and North African Podarcis phylogeny indi- cates unusual relative rates of mitochondrial gene evo- lution in reptiles.- Molecular Phylogenetics and Evolu- tion, Chicago; 38: 266-273. POSADA, D. &. CRANDALL, K. A. (1998): Modeltest: testing the model of DNA substitution- Bioinformatics, Oxford; 14: 817-818. SWOFFORD, D. L. (2002): PAUP*. Phylogenetic analy- sis using parsimony (*and other methods). Version 4.0. Sinauer Associates, Uderland, Massachusetts. WADK, E. (2001): Review of the False Smooth snake genus Macroprotodon (Serpentes, Colubridae) in Algeria with a description of a new species.- Bulletin National Fig. 1 : Adult death adder (Acanthophis laevis com- History Museum London (Zoology), London; 67 (1): plex) from Negeri Lima, Ambon (Central Maluku 85-107. regency, Maluku province, Indonesia). Photograph by U. KUCH. KEYWORDS: mitochondrial DNA, cyto- chrome b, Macroprotodon, evolution, systematics, Iberian Peninsula, North Africa SUBMITTED: April 1,2005 and Bali by the live animal trade. -

Charles Darwin University Death Adder Envenoming Causes
Charles Darwin University Death Adder Envenoming Causes Neurotoxicity Not Reversed by Antivenom - Australian Snakebite Project (ASP-16) Johnston, Christopher; O'Leary, Margaret; Brown, Simon; Currie, Bart; Halkidis, Lambros; Whitaker, Richard; Close, Benjamin; Isbister, Geof Published in: PLoS Neglected Tropical Diseases DOI: 10.1371/journal.pntd.0001841 Published: 01/01/2012 Document Version Publisher's PDF, also known as Version of record Link to publication Citation for published version (APA): Johnston, C., O'Leary, M., Brown, S., Currie, B., Halkidis, L., Whitaker, R., Close, B., & Isbister, G. (2012). Death Adder Envenoming Causes Neurotoxicity Not Reversed by Antivenom - Australian Snakebite Project (ASP-16). PLoS Neglected Tropical Diseases, 6(9), 1-8. https://doi.org/10.1371/journal.pntd.0001841 General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 03. Oct. 2021 Death Adder Envenoming Causes Neurotoxicity Not Reversed by Antivenom - Australian Snakebite Project (ASP-16) Christopher I. -
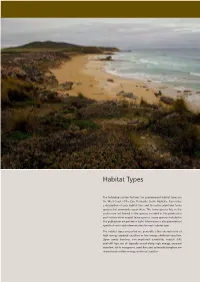
Habitat Types
Habitat Types The following section features ten predominant habitat types on the West Coast of the Eyre Peninsula, South Australia. It provides a description of each habitat type and the native plant and fauna species that commonly occur there. The fauna species lists in this section are not limited to the species included in this publication and include other coastal fauna species. Fauna species included in this publication are printed in bold. Information is also provided on specific threats and reference sites for each habitat type. The habitat types presented are generally either characteristic of high-energy exposed coastline or low-energy sheltered coastline. Open sandy beaches, non-vegetated dunefields, coastal cliffs and cliff tops are all typically found along high energy, exposed coastline, while mangroves, sand flats and saltmarsh/samphire are characteristic of low energy, sheltered coastline. Habitat Types Coastal Dune Shrublands NATURAL DISTRIBUTION shrublands of larger vegetation occur on more stable dunes and Found throughout the coastal environment, from low beachfront cliff-top dunes with deep stable sand. Most large dune shrublands locations to elevated clifftops, wherever sand can accumulate. will be composed of a mosaic of transitional vegetation patches ranging from bare sand to dense shrub cover. DESCRIPTION This habitat type is associated with sandy coastal dunes occurring The understory generally consists of moderate to high diversity of along exposed and sometimes more sheltered coastline. Dunes are low shrubs, sedges and groundcovers. Understory diversity is often created by the deposition of dry sand particles from the beach by driven by the position and aspect of the dune slope. -

The Brown Snake Complex Genus Pseudonaja Formally Demansia
The Brown Snake Complex Genus Pseudonaja formally Demansia All Brown Snakes are egg layers not live bearers and all but one species the Ringed Brown (Pseudonaja modesta) should be classed as deadly. Specific antivenom is Brown snake antivenom. The Common or Eastern Brown (Pseudonaja textilis textilis) Found over much of Victoria especially in the drier areas. It is to be found in the south eastern corner of South Australia and most of New South Wales. Its range covers most of Queensland and has been recorded in a few spots of the Northern Territory; it is also found in parts of New Guinea. The venom of this snake is strongly coagulant and neurotoxic though other toxins are also present. The Eastern brown usually produces from 10 to 30 eggs. Egg counts will usually depend on the size of the snake. Browns are quite common in the wheat and other grain growing areas and their numbers have multiplied to take advantage of the mice that follow the grain. Browns being rather slender snakes can get their heads down mouse burrows or into places where mice would otherwise be safe. The Browns eat all the mice meaning the whole family. After taking care of the larger mice they’ll consume all the baby mice. If the mother gets away and these baby mice were left then she would return and rear them. Within a few more weeks all the females would be pregnant and then they would of course, start to breed like mice. My belief is that without Brown snakes in Australia we would find it very difficult to grow any grain (cereal) crops at all. -

BIOLOGICAL SURVEY of KANGAROO ISLAND SOUTH AUSTRALIA in NOVEMBER 1989 and 1990
A BIOLOGICAL SURVEY OF KANGAROO ISLAND SOUTH AUSTRALIA IN NOVEMBER 1989 and 1990 Editors A. C. Robinson D. M. Armstrong Biological Survey and Research Section Heritage and Biodiversity Division Department for Environment, Heritage and Aboriginal Affairs, South Australia 1999 i Kangaroo Island Biological Survey The Biological Survey of Kangaroo Island, South Australia was carried out with the assistance of funds made available by, the Commonwealth of Australia under the 1989-90 National Estate Grants Programs and the State Government of South Australia. The views and opinions expressed in this report are those of the authors and do not necessarily represent the views or policies of the Australian Heritage Commission or the State Government of South Australia. The report may be cited as: Robinson, A. C. & Armstrong, D. M. (eds) (1999) A Biological Survey of Kangaroo Island, South Australia, 1989 & 1990. (Heritage and Biodiversity Section, Department for Environment, Heritage and Aboriginal Affairs, South Australia). Copies of the report may be accessed in the library: Environment Australia Department for Environment, Heritage and Aboriginal Affairs GPO Box 636 or 1st Floor, Roma Mitchell House CANBERRA ACT 2601 136 North Terrace, ADELAIDE SA 5000 EDITORS A.C. Robinson, D.M. Armstrong, Biological Survey and Research, Heritage &Biodiversity Section, Department for Environment Heritage and Aboriginal Affairs PO Box 1047 ADELAIDE 5001 AUTHORS D M Armstrong, P.J.Lang, A C Robinson, Biological Survey and Research, Heritage &Biodiversity Section, Department for Environment, Heritage and Aboriginal Affairs PO Box 1047 ADELAIDE 5001 N Draper, Australian Cultural Heritage Management Pty Ltd, 53 Hackney Rd. HACKNEY, SA 5069 G Carpenter, Biodiversity Monitoring and Evaluation, Heritage &Biodiversity Section, Department for Environment Heritage and Aboriginal Affairs. -
Creatures That Can Kill You 5
AROUND THE WORLD PREVIEWITH WSNAKES Preview Snakes slither through nearly every country on Earth. Most snakes are harmless, but some of them are are anything but. In this chapter, we will travel from India to Australia to Africa. The scariest, the deadliest, and the most feared snakes—they’re all here! 1 Around The World With Snakes AROUNDIn a rice THEfield in WORLD India, a young WITH worker namedSNAKES Abhay stepped carefully around the plants he tended. As always, Abhay listened for any quick rustling through the leaves or, worse yet, In a ricea sudden field hissing. in India, But as thea youngsky began workergrowing named Abhaydark stepped with rain carefully clouds, Abhay around became the careless plants he in his hurry to finish his job. He moved quickly tended.through As always, some tallerAbhay plants listened that blocked for any his quick rustlingview through of the ground. the leaves or, worse yet, a sudden hissing. But as the sky began growing dark with rain clouds, Abhay became careless in his hurry to finish his job. He moved quickly through some taller plants that blocked his view of the ground. Then, just at the edge of the field, Abhay felt something very strange. It was as if a thick cord of rope had been yanked beneath his left foot. 3 4 MARIE NOBLE In that same instant, Abhay saw a flash of brown and gold rise up before him—the dreaded Indian cobra. It was not the first time he had seen this terrifying snake. From the time he was a young child, Abhay had often seen these 6- to 10-foot snakes slithering through the village where he lived. -

Frogs & Reptiles NE Vic 2018 Online
Reptiles and Frogs of North East Victoria An Identication and Conservation Guide Victorian Conservation Status (DELWP Advisory List) cr critically endangered en endangered Reptiles & Frogs vu vulnerable nt near threatened dd data deficient L Listed under the Flora and Fauna Guarantee Act (FFG, 1988) Size: of North East Victoria Lizards, Dragons & Skinks: Snout-vent length (cm) Snakes, Goannas: Total length (cm) An Identification and Conservation Guide Lowland Copperhead Highland Copperhead Carpet Python Gray's Blind Snake Nobbi Dragon Bearded Dragon Ragged Snake-eyed Skink Large Striped Skink Frogs: Snout-vent length male - M (mm) Snout-vent length female - F (mm) Austrelaps superbus 170 (NC) Austrelaps ramsayi 115 (PR) Morelia spilota metcalfei – en L 240 (DM) Ramphotyphlops nigrescens 38 (PR) Diporiphora nobbi 8.4 (PR) Pogona barbata – vu 25 (DM) Cryptoblepharus pannosus Snout-Vent 3.5 (DM) Ctenotus robustus Snout-Vent 12 (DM) Guide to symbols Venomous Lifeform F Fossorial (burrows underground) T Terrestrial Reptiles & Frogs SA Semi Arboreal R Rock-dwelling Habitat Type Alpine Bog Montane Forests Alpine Grassland/Woodland Lowland Grassland/Woodland White-lipped Snake Tiger Snake Woodland Blind Snake Olive Legless Lizard Mountain Dragon Marbled Gecko Copper-tailed Skink Alpine She-oak Skink Drysdalia coronoides 40 (PR) Notechis scutatus 200 (NC) Ramphotyphlops proximus – nt 50 (DM) Delma inornata 13 (DM) Rankinia diemensis Snout-Vent 7.5 (NC) Christinus marmoratus Snout-Vent 7 (PR) Ctenotus taeniolatus Snout-Vent 8 (DM) Cyclodomorphus praealtus -

Proteomic and Genomic Characterisation of Venom Proteins from Oxyuranus Species
This file is part of the following reference: Welton, Ronelle Ellen (2005) Proteomic and genomic characterisation of venom proteins from Oxyuranus species. PhD thesis, James Cook University Access to this file is available from: http://eprints.jcu.edu.au/11938 Chapter 1 Introduction and literature review Chapter 1 Introduction and literature review 1.1 INTRODUCTION Animal venoms are an evolutionary adaptation to immobilise and digest prey and are used secondarily as a defence mechanism (Tu and Dekker, 1991). Intriguingly, evolutionary adaptations have produced a variety of venom proteins with specific actions and targets. A cocktail of protein and peptide toxins have varying molecular compositions, and these unique components have evolved for differing species to quickly and specifically target their prey. The compositions of venoms differ, with components varying within the toxins of spiders, stinging fish, jellyfish, octopi, cone shells, ticks, ants and snakes. Toxins have evolved for the varying mode of actions within different organisms, yet many enzymes are common to different venoms including L-amino oxidases, esterases, aminopeptidases, hyaluronidases, triphosphatases, alkaline phosphomonoesterases, 2 2 phospholipases, phosphodiesterases, serine-metalloproteases and Ca +IMg +-activated proteases. The enzymes found in venoms fall into one or more pharmacological groups including those which possess neurotoxic (causing paralysis or interfering with nervous system function), myotoxic (damaging muscle), haemotoxic (affecting the blood, -

NATURE TERRITORY April 2019 Newsletter of the Northern Territory Field Naturalists' Club Inc
NATURE TERRITORY April 2019 Newsletter of the Northern Territory Field Naturalists' Club Inc. In This Issue April Meeting p. 2 April Field Trip p. 3 Upcoming Activities p. 3 Death Adders pp. 4-5 Publications p. 5 Podcasts pp. 6-7 Chitter Chatter pp. 8-9 Club notices p. 10 Club web-site: http://ntfieldnaturalists.org.au/ Black-ringed Mangrove Snake (Hydrelaps darwiniensis) swimming around mangroves in Darwin Harbour. Photo: Nick Volpe FOR THE DIARY April Meeting: Wednesday 10 - Oysters going troppo ? research behind the recent success presented by Samantha Nowlands April Field Trip: Sunday 14 - Butterflies at East Point with Tissa Ratnayeke See pages 2 - 3 for m ore det ails Disclaimer: The views expressed in Nature Territory are not necessarily those of the NT Field Naturalists' Club Inc. or members of its Committee. April Meeting Oysters going troppo ? research behind the recent success presented by Samantha Nowland Wednesday 10, 7.45 pm, CDU Casuarina, Room BLUE 2.2.24 Sum m ary: Darwin Aquaculture Centre's (DAC) Black-lip Oyster hatchery research program and work with Aboriginal communities in South Goulburn Island has received a lot of media coverage in recent years, and it isn't stopping any time soon. DAC's collaboration with Traditional Owners in the Warruwi community on South Goulburn Island was showcased nationally this weekend on ABC's Landline program (https://www.abc.net.au/news/2019-03-30/native-oysters:-the-beginning-of-a-new-industry-in/10956306). The DAC team has worked extremely hard to get this program to where it is today.