Bulletin June 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sb238 Testimony Tre-Psm 02-06-17
Bill 238 Testimony: Safe passing distance of 3 feet 30 cyclists killed in Hawaii in last 10 years. If this does not sound like very much, consider that for every cyclist killed, roughly 70 are seriously injured based on national averages. That’s approximately 2,100 bicycle related injuries here in Hawaii. 44% of cyclists fatalities result from being struck from behind or sideswiped, also a national statistic 12% of cyclists feel threatened by motor vehicles passing too close. I’ll explain why. This bill is important because it sets a standard for motorists; unless you are a cyclist, you don’t know what a safe passing distance is. Here is an example: Kamehameha Hwy in windward Oahu. For much of it, there is an 18 to 24 inch shoulder. If the cyclists rides in the middle of the shoulder, there is 9 to 12 inches between his wheel line and the shoulder stripe. A bike’s handle bar is typically two feet wide, some are more. The bar end extends into the lane when the cyclist is in the center of the shoulder. Rocks and dangerous debris often crop up in the shoulder, mandating the cyclist to abruptly swerve within the shoulder lane to avoid a spill. Should the cyclist swerve to the edge of the shoulder stripe, the handlebar will extend a foot into the lane. A car driver that had considered safe clearance to be 2 feet from the cyclist while in the center of the shoulder would strike the cyclist, even though the bicycle wheels remain within the shoulder. -

RADICAL SABBATICAL 8 Days/7 Nights in Hawaii on the Islands of Maui and Oahu
Incredible Adventures & SPECOPS present a RADICAL SABBATICAL 8 days/7 nights in Hawaii on the islands of Maui and Oahu Day 1 - Arrival Welcome to Maui! Your first day in paradise is reserved for pure rest and relaxation – enjoy it while you can. After a personal pick-up at the airport, you and the SPECOPS guide will bond through an intellectu- ally stimulating conversation on your way to a comfortable Bed & Breakfast where the remainder of the day is spent lounging poolside and walking the beautiful beaches of Maui. If you are “geographically challenged,” be careful of the questions you ask. For example, when you're sitting at the bar in your Ad- mit Nothing T-shirt boldly sipping a fu-fu drink, don't look across the water at Lanai and ask “Excuse me, is that Japan?” Day 2 – Chopper Flight, Surfing, Kayaking, Whale Watching (when in season) Bright and early a SPECOPS guide leads the Group to the heliport, which is the exfiltration point for an exhilarating flight/airborne tour to Hana, a sleepy little community nestled between pristine, tropical landscapes and the rugged Pacific Ocean. Upon arrival, another SPECOPS guide meets the Group and leads us to the oceanfront or garden view cottages. Once checked-in, he provides an in-depth ori- entation of the itinerary. The Special Forces instructor is not only a great host, but also a highly experi- enced surfer, lifeguard, medic, boat handler and survival instructor. The morning and afternoon is spent learning about ocean currents, tides, wave dynamics and marine condition evaluation techniques. -
![Road Rash Psp Iso Download Road Rash (E) [SLES-00158] PS1 ISO](https://docslib.b-cdn.net/cover/1899/road-rash-psp-iso-download-road-rash-e-sles-00158-ps1-iso-1241899.webp)
Road Rash Psp Iso Download Road Rash (E) [SLES-00158] PS1 ISO
road rash psp iso download Road Rash (E) [SLES-00158] PS1 ISO. The PlayStation (officially abbreviated to PS, and commonly known as the PS1 or its codename, PSX) is a home video game console developed and marketed by Sony Computer Entertainment. The console was released on 3 December 1994 in Japan, 9 September 1995 in North America, 29 September 1995 in Europe, and 15 November 1995 in Australia. The console was the first of the PlayStation lineup of home video game consoles. It primarily competed with the Nintendo 64 and the Sega Saturn as part of the fifth generation of video game consoles. The PlayStation is the first “computer entertainment platform” to ship 100 million units, which it had reached 9 years and 6 months after its initial launch. In July 2000, a redesigned, slim version called the PS one was released, replacing the original grey console and named appropriately to avoid confusion with its successor, the PlayStation 2. The PlayStation 2, which is backwards compatible with the PlayStation’s DualShock controller and games, was announced in 1999 and launched in 2000. The last PS one units were sold in late 2006 to early 2007 shortly after it was officially discontinued, for a total of 102 million units shipped since its launch 11 years earlier. Games for the PlayStation continued to sell until Sony ceased production of both the PlayStation and PlayStation games on 23 March 2006 – over 11 years after it had been released, and less than a year before the debut of the PlayStation 3. DOWNLOADING AND RUNNING ISO FILES: Road Rash (E) [SLES-00158] is one of the best games of PS1 console. -

Computers Guide to Sega Genesis Ebook
COMPUTERS GUIDE TO SEGA GENESIS PDF, EPUB, EBOOK S. Schwartz | 191 pages | 31 Dec 1990 | Compute! Publications Inc.,U.S. | 9780874552386 | English | Greensboro, United States Computers Guide to Sega Genesis PDF Book Would you recommend this Guide? It makes quality products that not only emulate the classics but oftentimes improve them. Destroy them both, while avoiding their balls at the same time. Interactive Studios. Multiplayer adaptors — There are a number of multiplayer adapters which allow for up to four players to participate in games designed for multiplayer action. Loungefly licenses dozens of pop-culture brands and turns them into cute and clever bags and accessories. Be sure to keep an eye out for Buzz Bombers, because there are loads of 'em in this area. Use the steps and quickly make your way to the top, because the water will be rising. Jump on any purple platforms to avoid getting pushed off, and get back on the green block when it's safe. Inhale another bubble, and head up the steps. Also known as Vasum. Hop on one of the platforms of the first conveyor belt, and ride it across. Madagascar's Cancelled Party Game. In my links page, I have some good links to sites where you can download ROMs. Similar and even more unsuccessful baseball bat and golf club peripheral systems were also available and as such were limited use with the specific games for which they were designed. Move on, and you'll see a moving platform going up and down beside a wall. At the end, avoid the spikes, and jump on the ledge. -

Godlike Gaming.Pdf
For kids today who are growing up with gesture recognition consoles and augmented reality goggles, it might be hard to imagine that only a generation ago, playing a video game meant popping a quarter in an arcade cabinet located in the corner of a mall or restaurant. The gaming industry has indeed come a long way from arcade games like Tron and Pac-Man to Massively Multiplayer Online role-playing games like World of Warcraft. The video gaming industry is the fastest growing segment in the entertainment industry. Worth US$71 billion, it has already Pac-Man, developed by Namco, was surpassed the music industry and is fast catching up with the US$87 first released in Japan on May 22, billion film industry. Major video game titles of today have budgets 1980. comparable to that of Hollywood blockbusters. Grand Theft Auto V, a popular game title, was produced with a budget of US$250 million, in line with Hollywood blockbusters like Spiderman 3, Avatar, etc. While the industry has capitalized on the public’s seemingly unquenchable appetite for video games, there is still a huge potential for growth. However, there are also significant risks and uncertainties for companies in this industry. The success or failure of a major title can make or break a publisher’s or developer’s Super Mario Bros. sold over 40 business. It is amidst all these insecurities that IP becomes vital. million copies, making it the best- Developing a pre-emptive IP strategy to safeguard appropriate IP selling video game of the whole rights is essential for the success of a game publisher. -

Road Rash Free Game Download Full Version
Road rash free game download full version Road Rash is racing game, published in by Electronic Arts. We gave We gave this game stunning rating of 85 and you can download it for free right here. download here.. How to Download Road Rash Game For Pc Full Version. Devesh. The Best Racing Game First Of all Install The Game After Installation, An Icon On Deskto Is Can Play this Installation. Thanks Click the Link below to Download this Game! File Size Downloading Road Rash on checkgames4u is free of cost and full version. Free Road Rash PC Game Download Full Version Hang On ISO Setup Download Road Rash 2 PC Game Full Version, Download Road Rash Game For. Minimum System Requirements. OS: Windows /XP/Vista; CPU: Pentium, 75 MHz Processor; RAM: 16 MB; Hard Drive: 30 MB free; Video. By GamesNostalgia: Road Rash is a violent motorcycle racing video game developed and In a remake was created for the 3DO and this version was ported to Windows in Anyway feel free to not download it:). Road Rash Game Free Download With Full Version For PC Is Now Available Here. Motor Bike Video Games Is Published By Electronic Arts. Fantastic Top. Road rash is a motorbike racing game. Road rash is the game where you have to try To take the lead in every race. If you become 1st, 2nd or 3rd place on the. Road Rash Free Download PC Game setup in single direct link for windows. Road Rash is a racing game which includes bike Rash PC Game. Road rash bike racing game free download full version pc. -

Classic Retro Games You Can Still Play Online
Classic Retro Games You Can Still Play Online Today’s game comes with a storyline, amazing graphics and of course, new challenges but still, retro games still have their charm. Sometimes, it feels nice to revisit the games that we played when we were children. Whether you played these retro games in your video games or Windows XP, you enjoyed them a lot, right? You will be fascinated to know that you will enjoy them even now! The retro games from the 80s and 90s are available online, sometimes in websites and other times in the form of a gaming app. The main point is that you can bring back your childhood days by playing these retro games online. Pac Man Pac Man is a maze arcade game that was invented in 1980 by Namco. It was a commercial success and in fact, was named one of the greatest video games of all time. The bold use of color and its signature music is all you need to go back to the sweet time. The game was particularly made colorful to appeal to the young players. In Pac Man, the player had to eat the tiny dots placed inside the maze while protecting oneself from the four colored ghosts. Did you know that these ghosts have names? The red one is Blinky, the pink one is Pinky, the cyan one is Inkly and the orange is named Clyde. When the player manages to eat all the dots, the next level starts. If the player makes contact with the ghost, life will be lost. -
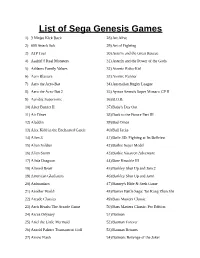
List of Sega Genesis Games
List of Sega Genesis Games 1) 3 Ninjas Kick Back 28) Art Alive 2) 688 Attack Sub 29) Art of Fighting 3) ATP Tour 30) Asterix and the Great Rescue 4) Aaahh!!! Real Monsters 31) Asterix and the Power of the Gods 5) Addams Family Values 32) Atomic Robo-Kid 6) Aero Blasters 33) Atomic Runner 7) Aero the Acro-Bat 34) Australian Rugby League 8) Aero the Acro-Bat 2 35) Ayrton Senna's Super Monaco GP II 9) Aerobiz Supersonic 36) B.O.B. 10) After Burner II 37) Baby's Day Out 11) Air Diver 38) Back to the Future Part III 12) Aladdin 39) Bad Omen 13) Alex Kidd in the Enchanted Castle 40) Ball Jacks 14) Alien 3 41) Ballz 3D: Fighting at Its Ballziest 15) Alien Soldier 42) Barbie Super Model 16) Alien Storm 43) Barbie Vacation Adventure 17) Alisia Dragoon 44) Bare Knuckle III 18) Altered Beast 45) Barkley Shut Up and Jam 2 19) American Gladiators 46) Barkley Shut Up and Jam! 20) Animaniacs 47) Barney's Hide & Seek Game 21) Another World 48) Barver Battle Saga: Tai Kong Zhan Shi 22) Arcade Classics 49) Bass Masters Classic 23) Arch Rivals: The Arcade Game 50) Bass Masters Classic: Pro Edition 24) Arcus Odyssey 51) Batman 25) Ariel the Little Mermaid 52) Batman Forever 26) Arnold Palmer Tournament Golf 53) Batman Returns 27) Arrow Flash 54) Batman: Revenge of the Joker 55) Battle Mania 84) Bubble and Squeak 56) Battle Squadron 85) Bubsy II 57) BattleTech: A Game of Armored Combat 86) Bubsy in: Claws Encounters of the Furred Kind 58) Battletoads 87) Buck Rogers: Countdown to Doomsday 59) Battletoads-Double Dragon 88) Bugs Bunny in Double Trouble 60) -

In the United States District Court for the District Of
Case 1:11-cv-00554-JMS-BMK Document 18 Filed 01/19/12 Page 1 of 15 PageID #: <pageID> IN THE UNITED STATES DISTRICT COURT FOR THE DISTRICT OF HAWAII STATE FARM FIRE & CASUALTY CIVIL NO. CV 11-00554 JMS-BMK COMPANY and STATE FARM (Declaratory Judgment) MUTUAL AUTOMOBILE INSURANCE COMPANY, Illinois FINDINGS AND corporations, RECOMMENDATION GRANTING PLAINTIFFS’ MOTION FOR Plaintiffs, DEFAULT JUDGMENT vs. ANTHONY SANTIAGO and MICHELLE DENAULT, Defendants. FINDINGS AND RECOMMENDATION GRANTING PLAINTIFFS’ MOTION FOR DEFAULT JUDGMENT Currently pending before this Court is Plaintiffs STATE FARM FIRE & CASUALTY COMPANY (“SFFCC”) and STATE FARM MUTUAL AUTOMOBILE INSURANCE COMPANY’s (“SFMAIC”) (collectively, “Plaintiffs” or “State Farm”) Motion for Default Judgment (“Motion”) filed on December 2, 2011. Said Motion came on for hearing on December 28, 2011. Upon careful consideration of the Motion, the supporting memoranda, and the arguments of counsel, this Court hereby finds and recommends that the Motion be GRANTED. Case 1:11-cv-00554-JMS-BMK Document 18 Filed 01/19/12 Page 2 of 15 PageID #: <pageID> BACKGROUND 1. In this action, State Farm seeks a binding declaration that, inter alia, it has no duty to defend or indemnify Defendants ANTHONY SANTIAGO (“Santiago”) and MICHELLE DENAULT (“Denault”) under two insurance policies issued by State Farm in connection with any claims that may arise out of a robbery and assault committed by Defendant Santiago on or about August 3, 2010. 2. In the instant Motion, State Farm seeks default judgment against Defendants Santiago and Denault pursuant to Rule 55 of the Federal Rules of Civil Procedure (“FRCP”) on the ground that Defendants have not answered or otherwise pled in response to Plaintiffs’ Complaint for Declaratory Judgment, filed herein on September 13, 2011 (“Complaint”), and that the undisputed facts establish, as a matter of law, that there is no coverage available under the subject insurance policies. -

James Hein 02/08/18 WP 1 Riding the Dragon the Landscape Becomes A
James Hein English 1100 2-1-18 James Hein 02/08/18 WP 1 Riding the Dragon The landscape becomes a blur of deciduous tree mixing with luscious evergreen pines as we climb into the Great Smokey Mountains flies past my tinted motorcycle visor. While riding a motorcycle is fun you, you should always follow the speed limits. An oddly warm day in the middle of May even for the higher elevations. I am thankful for my all black hoodie soaking up some of the sun rays as they poke through the trees casting shadows across the road. Ahead of me, rides a tall lanky man some would best describe him as a string bean, six foot two, 185 pounds soaking wet. He looks slightly too tall for his silver and black Yamaha FZ6r, a fast sports bike style motorcycle. Hunter is a very handsome, charismatic guy, intellectual and able to hold a conversation with just about anyone. I have known Hunter now for about four years having been stationed together in the Marine Corps. We decided to finally take our “guy’s trip” due to the fact my wife was going to Maine for our soon to be born son’s baby shower. Even though Hunter is a very smart man, he can tend to let speed get the best of him. I’m trying to keep up with Hunter, but I can feel every pothole and bump in the road. Unlike Hunter’s motorcycle mine is an all-black Kawasaki Ninja 250 nearly one third the size of his. -
Bear Baiting on U.S. Army Fort Wainwright Lands 2016
FREE RECYCLED an edition of the Recycled material is used in the making of our ALASKA POST newsprint The Interior Military News Connection Vol. 7, No. 12 Fort Wainwright, Alaska March 25, 2016 Guardsmen participate in cold weather exchange with Mongolian Armed Forces Alaska National Guard Public Affairs golia’s peace-keeping operations capability,” said Maj. Samuel Scott, 1-197th R&S executive officer. A five-man team from the Alaska Army Nation- Training events included equipment briefs, cold weath- al Guard’s 1-297th Reconnaissance and Surveillance er injury classes, field demonstrations of the effects of Squadron has returned from Mongolia after a cold cold weather on equipment and operations, avalanche weather subject-matter-expert exchange with the Mon- safety and skiing. The culminating exercise was a climb golian Armed Forces last month. of a local peak in which MAF and AKARNG Soldiers The purpose of the exercise was to support the Alaska had the opportunity to use techniques learned during the National Guard’s state partnership with Mongolia, giv- subject matter expert exchange. ing MAF Soldiers the opportunity to learn about cold Along with Scott, the AKARNG team consisted of weather and mountain tactics, techniques and procedures Staff Sgt. Cody Tirpak, Staff Sgt. Dayton Will, Sgt. Eli- Alaska Guardsman Staff Sgt. Cody Tirpak, 1-297th from AKARNG Soldiers. The four-day exchange was jah Gutierrez and Sgt. Jacob Rukovishnikoff, all experts Reconnaissance and Surveillance Squadron, demon- conducted at the Five Hills Training Area near Ulaan- in different facets of cold weather travel and mountain- strates proper glissading during a cold weather sub- baatar, Mongolia, Feb. -

000 Front Page.Pub
007 Racing * 007: Licence to Kill* 100% Dynamite* 1000 Miglia * 1000cc Turbo * 12 Volt * 18 Wheeler * 18 Wheeler: American Pro Trucker * 18 Wheels of Steel Across America * 18 Wheels of Steel: Convoy * 187 Ride or Die * 19 Part 1: Boot Camp* 1nsane * 1Xtreme * 280 ZZZAP * 3D Deathchase* 3D Real Driving * 3D Scooter Racing * 3D Slot Car Racing * 3D Stock Car Championship* 3D Ultra RC Racers * 3D Waterski * 4 Wheel Thunder * 4D Sports Driving * 4D Sports Driving Master Tracks I * 4-Wheel Thunder * 4x4 EVO 2 * 4X4 Evo 2 * 4x4 EVO 2 * 4x4 Evolution * 4X4 Evolution * 4x4 Evolution * 4X4 Evolution 2 * 4x4 Off-Road Racing* 4x4 Off-Road Racing * 4x4 World Trophy * 4X4 World Trophy * 500cc GP * 500cc Grand Prix * 500cc Motomanager * 5th Gear * 750cc Grand Prix* 911 Tiger Shark * A2 Racer * A2 Racer II * A2 Racer III: Europa Tour * AB Cop * Ace Combat 3 * Ace Combat 3: Electrosphere * Ace Driver * Ace Driver Victory Lap * Action Biker* Action Biker * Action Fighter* Action Girlz Racing * Adrenalin * Adrenalin 2 * Adrenalin 2: Rush Hour * Adrenalin Extreme Show * Advan Racing * Advance GTA * Advance GTA 2 * Advance Rally * Aero Fighters Assault * AeroGauge * African Raiders-01 * African Trail Simulator* Agent X* Air Race * Air Race Championship * Al Unser Jr.'s Turbo Racing * Al Unser Jr's Road to the Top * Al Unser, Jr. Arcade Racing * Alarm for Cobra 11: Hot Pursuit * Alfa Romeo Racing Italiano * All Japan Grand Touring Car Championship * All Points Bulletin * All Terrain Rally * All Terrain Vehicle Simulator * Alley Rally * All-Star Racing *