Gluten Opioids: Immune Dysfunction, and Mood Updated: SEPT 2020 Erik Vose, NMD Disclaimer: “Gluten-Free” Does Not Necessarily Mean Healthy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of in Silico Approach for Prediction of Presence of Opioid Peptides in Wheat
Evaluation of in silico approach for prediction of presence of opioid peptides in wheat This is the Accepted version of the following publication Garg, Swati, Apostolopoulos, Vasso, Nurgali, Kulmira and Mishra, Vijay Kumar (2018) Evaluation of in silico approach for prediction of presence of opioid peptides in wheat. Journal of Functional Foods, 41. 34 - 40. ISSN 1756-4646 The publisher’s official version can be found at https://www.sciencedirect.com/science/article/pii/S1756464617307454 Note that access to this version may require subscription. Downloaded from VU Research Repository https://vuir.vu.edu.au/36577/ 1 1 Evaluation of in silico approach for prediction of presence of opioid peptides in wheat 2 gluten 3 Abstract 4 Opioid like morphine and codeine are used for the management of pain, but are associated 5 with serious side-effects limiting their use. Wheat gluten proteins were assessed for the 6 presence of opioid peptides on the basis of tyrosine and proline within their sequence. Eleven 7 peptides were identified and occurrence of predicted sequences or their structural motifs were 8 analysed using BIOPEP database and ranked using PeptideRanker. Based on higher peptide 9 ranking, three sequences YPG, YYPG and YIPP were selected for determination of opioid 10 activity by cAMP assay against µ and κ opioid receptors. Three peptides inhibited the 11 production of cAMP to varied degree with EC50 values of YPG, YYPG and YIPP were 5.3 12 mM, 1.5 mM and 2.9 mM for µ-opioid receptor, and 1.9 mM, 1.2 mM and 3.2 mM for κ- 13 opioid receptor, respectively. -

Bibliography Section
ISSN 0021-9673 VOL. 524 NO.6 DECEMBER 21, 1990 THIS ISSUE COMPLETES VOL. 524 Bibliography Section EDITORS R. W. Giese (Boston, MA) J. K. Haken (Kensington, N.S.W.) K. Macek (Prague) L. R. Snyder (Orinda, CA) EDITOR, SYMPOSIUM VOLUMES, E. Heitmann (Orinda, CAl EDITORIAL BOARD D. W. Armstrong (Rolla. MO) W. A. Aue (Halifax) P. Bocek (Brno) A. A. Boulton (Saskatoon) P. W. Carr (Minneapolis. MN) N. H. C. Cooke (San Ramon. CAl V. A. Davankov (Moscow) Z. Deyl (Prague) S. Dilli (Kensington. N.S.W.) H. Engelhardt (Saarbrucken) F. Erni (Basle) M. B. Evans (Hatfield) J. L. Glajch (N. Billerica. MA) G. A. Guiochon (Knoxville. TN) P. R. Haddad (Kensington. N.S.w.) I. M. Hais (Hradec Kralove) W. S. Hancock (San Francisco, CAl S. Hjerten (Uppsala) Cs. Horvath (New Haven, CT) J. F. K. Huber (Vienna) K.-P. Hupe (Waldbronn) 1. W. Hutchens (Houston. TX) J. Janak (Brno) P. Jandera (Pardubice) B. L. Karger (Boston. MA) E. sz. Kovats (Lausanne) A. J. P. Martin (Cambridge) L. W. McLaughlin (Chestnut Hill, MA) E D. Morgan (Keele) J. D. Pearson (Kalamazoo. MI) H. Poppe (Amsterdam) F. E. Regnier (West Lafayette. IN) P. G. Righetti (Milan) P. Schoenmakers (Eindhoven) G..Schomburg (MulheimjRuhr) R. Schwarzeobach (Dubendorf) R. E. .s~OlJ~ (West Lafayette. IN) -A.JVI. Siouffi'(Marseille) D. J. Strydom' (Boston, MA) K. K. Ugger (Mainz) R. VerP'l0rte (Leideo). Gy. Vigh tColiege Statioo, TX) oJ. T vtiMpo (E~SI ta~sihg. MI) B. D. ~&terlunp ,(UPl1sala) EDITORS, BIBLIOGRAPHY SECTION z. Deyl (Prague), J. Janak (Brno). V. Schwarz (Prague), K Ma~ek (Prague) ELSEVIER JOURNAL OF CHROMATOGRAPHY Scope. -

Efficacy and Safety of Gluten-Free and Casein-Free Diets Proposed in Children Presenting with Pervasive Developmental Disorders (Autism and Related Syndromes)
FRENCH FOOD SAFETY AGENCY Efficacy and safety of gluten-free and casein-free diets proposed in children presenting with pervasive developmental disorders (autism and related syndromes) April 2009 1 Chairmanship of the working group Professor Jean-Louis Bresson Scientific coordination Ms. Raphaëlle Ancellin and Ms. Sabine Houdart, under the direction of Professor Irène Margaritis 2 TABLE OF CONTENTS Table of contents ................................................................................................................... 3 Table of illustrations .............................................................................................................. 5 Composition of the working group ......................................................................................... 6 List of abbreviations .............................................................................................................. 7 1 Introduction .................................................................................................................... 8 1.1 Context of request ................................................................................................... 8 1.2 Autism: definition, origin, practical implications ........................................................ 8 1.2.1 Definition of autism and related disorders ......................................................... 8 1.2.2 Origins of autism .............................................................................................. 8 1.1.2.1 Neurobiological -

Opioid Peptides in Peripheral Pain Control
Review Acta Neurobiol Exp 2011, 71: 129–138 Opioid peptides in peripheral pain control Anna Lesniak*, Andrzej W. Lipkowski Mossakowski Medical Research Centre Polish Academy of Sciences, Warsaw; *Email: [email protected] Opioids have a long history of therapeutic use as a remedy for various pain states ranging from mild acute nociceptive pain to unbearable chronic advanced or end-stage disease pain. Analgesia produced by classical opioids is mediated extensively by binding to opioid receptors located in the brain or the spinal cord. Nevertheless, opioid receptors are also expressed outside the CNS in the periphery and may become valuable assets in eliciting analgesia devoid of shortcomings typical for the activation of their central counterparts. The discovery of endogenous opioid peptides that participate in the formation, transmission, modulation and perception of pain signals offers numerous opportunities for the development of new analgesics. Novel peptidic opioid receptor analogs, which show limited access through the blood brain barrier may support pain therapy requiring prolonged use of opioid drugs. Key words: immune cells, opioid peptides, pain, peripheral analgesia Abbreviations: β-FNA - β-funaltrexamine, BBB - blood-brain-barrier, CGRP - calcitonin gene-related peptide, CFA - complete Freund adjuvant, CNS - central nervous system, CRF - corticotropin releasing factor, CYP - cyprodime, DAGO - [Tyr-D-Ala- Gly-Me-Phe-Gly-ol]-enkephalin, DAMGO - [D-Ala2, N-MePhe4, Gly-ol]-enkephalin, DOR - delta opioid receptor, DPDPE - [D-Pen2,5]-enkephalin, DRG - dorsal root ganglion, EM-1 - endomorphin 1, EM-2 - endomorphin 2, KOR - kappa opioid receptor, MOR - mu opioid receptor, NLZ – naloxonazine, NTI - naltrindole, NLXM - naloxone methiodide; nor-BNI – nor-binaltorphimine, PDYN - prodynorphin, PENK - proenkephalin, PNS - peripheral nervous system, POMC - proopiomelanocortin INTRODUCTION ic pain. -

Chemical Characterization and Opioid Activity of an Exorphin Isolated from in Vivo Digests of Casein
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Volume 196, number2 FEBS 3363 February 1986 Chemical characterization and opioid activity of an exorphin isolated from in vivo digests of casein Hans Meisel Institut fir Chemie und Physik der Bundesanstalt fzZr Milchforschung, 2300 Kiel, FRG Received 17 October 1985; revised version received 4 December 1985 The in vivo formation of an opioid peptide (exorphin) derived from p-casein has been proved for the first time. It was isolated from duodenal thyme of minipigs after feeding with the milk protein casein. The exorphin has been identified as a /?-casein fragment by end-group determinations and qualitative amino acid analysis of the purified peptide. This peptide, named /I-casomorphin-l l, displayed substantial opioid activity in an opiate receptor-binding assay. Exorphin Casomorphin @Casein (Duodenal digest) Opioid activity 1. INTRODUCTION cipitated casein (Biogen-~asein, Bayr. Milchver- sorgung, N~rnberg) after overnight fasting. Post- The existence of opioid peptides has been de- prandial duodenum samples were taken for 8 h, scribed in partial enzymatic digests of proteins frozen immediately in liquid nitrogen and freeze- derived from foodstuffs [l-3]. These peptides are dried. A control experiment was performed after called exorphins because of their exogenous origin feeding with a maize starch diet composed as in [9] and morphine-like activities. without casein. Such opioid peptides have been discovered re- The extraction of 110 g freeze-dried duodenal cently in enzymatic digests of whole bovine casein thyme from 5 collection periods with chloroform/ and were designated as Bcasomorphins because methanol (65 : 35, v/v), and the following batchwise their sequences identified them as fragments of adsorption/desorption procedure was performed bovine fl-casein [4]. -

The History of Iodine in Medicine Part I
usually credited with the discovery of the elementary nature of chlorine, which he announced in 1810.”14 The History of Iodine Bernard Courtois, a French chemist, was a saltpeter in Medicine (potassium nitrate) manufacturer. Saltpeter was one of the compounds needed for the manufacture of gunpow- Part I: From Discovery to der. Seaweed ash was used as a valuable source of so- dium and potassium salts. Sulfuric acid was added to Essentiality remove interfering compounds before the salts could be precipitated. One day toward the end of AD 1811, Cour- by Guy E. Abraham, MD tois added too much acid to the suspension of seaweed Part I: From Discovery to Essentiality ash. The iodides in seaweed were oxidized to iodine, The essential element iodine has been kept in the Dark which sublimated and formed a violet vapor above the Ages over the last 60 years after World War II. In order preparation. The crystals obtained from condensation of to partially remedy the gross neglect of this essential the iodine vapor were analyzed by Courtois and he pre- element by the medical profession, poorly represented in pared several iodide salts. Courtois never published his medical textbooks and vilified in endocrine publications, findings. Some of these crystals ended up in the hands the Journal of The Original Internist will start a series of of Gay-Lussac and Ampere who gave some to H. Davy. publications on the history of iodine in medicine from discovery to the present. This series of publications is Although Courtois discovered iodine in 1811, it was part of a book on the Iodine Project which was imple- Gay-Lussac who proved that it was a new element and mented by the author 6 years ago. -

Gluten Exorphin C
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector Volume 316, number I, 17-19 FEBS 11997 January 1993 0 1993 Federation of European Biochemical Societies 00145793/93/$6.00 Gluten exorphin C A novel opioid peptide derived from wheat gluten Shin-ichi Fukudome” and Masaaki Yoshikawab “Research Control Depu~t~eilt~ ~is~sh~n Flbur hilling Co., Ltd., Niho~bu~ll~~ Chuv-ku, Tokyo 103, Jupan and ‘Department of’ Food Science and Technology, Faculty of Agriculture, K.yoto University, Kyoto 606, Japan Received 5 November 1992; revised version received 30 November 1992 A novel opioid peptide, Tyr-Pro-Be-Ser-Leu, was isolated from the pepsin-trypsin-chymotrypsin digest of wheat gluten. Its IC,, values were 40 PM and 13.5 PM in the GPI and MVD assays, respectively. This peptide was named gluten exorphin C. Gluten exorphin C had a structure quite different from any of the endogenous and exogenous opioid peptides ever reported in that the N-terminal Tyr was the only aromatic amino acid. The analogs containing Tyr-Pro-X-Ser-Leu were synthesized to study its StructLlre~activity relationship. Peptides in which X was an aromatic amino acid or an aiiphatic hydrophobic amino acid had opioid activity. Opioid peptide; Wheat; Gluten; Exorphin 1. INTRODUCTION one was from U.S.P.C., Inc. 13HJDAG0 and [“HIDADLE were from Amersham. Other reagents used were of reagent grade or better. The presence of the opioid peptides has been recog- 2.2. Enqnzatic digestion ofwheat gluten nized in the pepsin digest of wheat gluten [1,2]. -

Evaluation of Production of Opioid Peptides from Wheat Proteins
Evaluation of Production of Opioid Peptides from Wheat Proteins Swati Garg This thesis is submitted in total fulfilment of the requirements for the degree of Doctor of Philosophy Principal Supervisor: Dr. Vijay Kumar Mishra Co-Supervisors: Associate Professor Kulmira Nurgali Professor Vasso Apostolopoulos Institute for Sustainable Industries and Liveable Cities Victoria University Melbourne, Australia 2019 I dedicate this thesis to my father-in-law Late Sh. Puran Chand Goel & my family Abstract Opioids such as morphine and codeine are the most commonly clinically used drugs for pain management, but have associated side-effects. Food-derived opioid peptides can be suitable alternative due to less side-effect and are relatively inexpensive to produce. So, wheat protein (gluten) was tested as source for production of opioid peptides. The thesis reports results of investigations carried out on production of opioid peptides from wheat gluten using enzymatic hydrolysis and fermentation by selected lactic acid bacteria and characterisation of bioactivity (opioid) of prepared peptides and gluten hydrolysates. Gluten protein sequences were accessed using in silico approach (Biopep database and PeptideRanker) to predict presence of opioid peptides. The search was based on presence of tyrosine and proline. This led to selection of three peptides for which opioid activity was measured by cAMP (cyclic adenosine monophosphate) assay. The EC50 values of YPG, YYPG and YIPP were 1.78 mg/mL, 0.74 mg/mL and 1.42 mg/mL for μ- opioid receptor, respectively. Hydrolysates from gluten were produced using two different approaches, fermentation using lactic acid bacteria (LAB) and by commercial proteases. Six LAB (Lb. acidophilus, Lb. -

Current Medicinal Chemistry, 2016, 23, 893-910
893 Send Orders for Reprints to [email protected] Current Medicinal Chemistry, 2016, 23, 893-910 eISSN: 1875-533X ISSN: 0929-8673 Current Impact Factor: Food Proteins as Source of Opioid Peptides-A Review 3.85 Medicinal Chemistry The International Journal for Timely In-depth Reviews Swati Garg, Kulmira Nurgali and Vijay Kumar Mishra* in Medicinal Chemistry BENTHAM SCIENCE College of Health and Biomedicine, Victoria University, PO Box 14428, Melbourne, Victoria 8001, Australia Abstract: Traditional opioids, mainly alkaloids, have been used in the clinical management of pain for a number of years but are often associated with numerous side-effects including sedation, dizziness, physical dependence, tolerance, addiction, nausea, vomiting, constipa- tion and respiratory depression which prevent their effective use. Opioid peptides derived from food provide significant advantages as safe and natural alternative due to the possibility of their production using animal and plant proteins as well as comparatively less side-effects. This review aims to discuss the current literature on food-derived opioid peptides focusing on their produc- tion, methods of detection, isolation and purification. The need for screening more dietary proteins as a source of novel opioid peptides is emphasized in order to fully understand their potential in pain management either as a drug or as part of diet complementing therapeutic prescription. Keywords: Opioids, peptide, opioid-receptors, casomorphins, exorphin, fermentation. 1. INTRODUCTION dicinal effects are predominantly due to the presence of polyphenols, antioxidants, probiotics, tannins, polyun- Food provides energy and essential nutrients to the saturated fatty acids or bioactive peptides. body in the form of carbohydrates, proteins, fats, vita- mins and minerals which are necessary for proper Bioactive peptides are inactive within native pro- growth, development and functioning of the body. -

Food Addiction Institute Page 1 10/14/2009 Bibliography On
Food Addiction Institute Bibliography on Science and Treatment of Food Addiction up to 2009 This is a bibliography making the case for food addiction as a Substance Use Disorder. While all of the publications are a part of the argument for food as a biochemical dependency, those books and articles which are either original in making a part of the case or which give an overview of a section of the peer- reviewed professional literature are emphasized in bold type. There are 2,734 citations: 1) A majority are specific findings in peer reviewed scientific journals studying aspects of chemical dependency on food; - biochemical effects of sugar, fat, caffeine - interacting with dopamine and serotonin receptors; 2) Several are studies of other biochemical mechanisms effecting chemical dependency including leptin deficiency curtailing satiation, glycemic and insulin malfunctions, and allergies to wheat and other food substance; 3) Over 200 are journal articles showing the similar or identical biochemical or brain imaging results in studies of addiction to alcohol. cocaine, heroin, morphine, nicotine, gambling, sex and marijuana; 4) Over 100 are basic science studies mapping brain pathways or biochemical reactions to stress; 5) Over 100 are basic texts about obesity, eating disorders or addiction; and texts of self help treatments of food addiction, cookbooks eliminating addictive foods, 6) The rest are clinical studies including case studies of recovered food addicts, research on the effectiveness of food-related Twelve Step Programs, quantitative outcome research on food addiction treatment programs and qualitative research on food addiction denial. PW October 2009 For some of these 105 references there is a brief explanatory comment PW October 2009. -
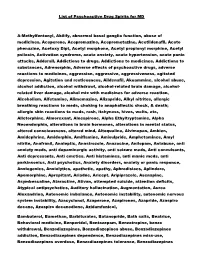
List of Psychoactive Drug Spirits for MD A-Methylfentanyl, Abilify
List of Psychoactive Drug Spirits for MD A-Methylfentanyl, Abilify, abnormal basal ganglia function, abuse of medicines, Aceperone, Acepromazine, Aceprometazine, Acetildenafil, Aceto phenazine, Acetoxy Dipt, Acetyl morphone, Acetyl propionyl morphine, Acetyl psilocin, Activation syndrome, acute anxiety, acute hypertension, acute panic attacks, Adderall, Addictions to drugs, Addictions to medicines, Addictions to substances, Adrenorphin, Adverse effects of psychoactive drugs, adverse reactions to medicines, aggression, aggressive, aggressiveness, agitated depression, Agitation and restlessness, Aildenafil, Akuammine, alcohol abuse, alcohol addiction, alcohol withdrawl, alcohol-related brain damage, alcohol- related liver damage, alcohol mix with medicines for adverse reaction, Alcoholism, Alfetamine, Alimemazine, Alizapride, Alkyl nitrites, allergic breathing reactions to meds, choking to anaphallectic shock, & death; allergic skin reactions to meds, rash, itchyness, hives, welts, etc, Alletorphine, Almorexant, Alnespirone, Alpha Ethyltryptamine, Alpha Neoendorphin, alterations in brain hormones, alterations in mental status, altered consciousness, altered mind, Altoqualine, Alvimopan, Ambien, Amidephrine, Amidorphin, Amiflamine, Amisulpride, Amphetamines, Amyl nitrite, Anafranil, Analeptic, Anastrozole, Anazocine, Anilopam, Antabuse, anti anxiety meds, anti dopaminergic activity, anti seizure meds, Anti convulsants, Anti depressants, Anti emetics, Anti histamines, anti manic meds, anti parkinsonics, Anti psychotics, Anxiety disorders, -

Opioid Peptides Encrypted in Intact Milk Protein Sequences
Downloaded from British Journal of Nutrition (2000), 84, Suppl. 1, S27±S31 S27 https://www.cambridge.org/core Opioid peptides encrypted in intact milk protein sequences Hans Meisel1* and R. J. FitzGerald2 1 Bundesanstalt fuÈr Milchforschung, Institut fuÈr Chemie und Physik, Kiel, Germany . IP address: 2Life Science Department, University of Limerick, Limerick, Ireland Opioid agonistic and antagonistic peptides which are inactive within the sequence of the 170.106.40.40 precursor milk proteins can be released and thus activated by enzymatic proteolysis, for example during gastrointestinal digestion or during food processing. Activated opioid peptides are potential modulators of various regulatory processes in the body. Opioid peptides can interact with subepithelial opioid receptors or specific luminal binding sites in the intestinal tract. , on Furthermore, they may be absorbed and then reach endogenous opioid receptors. 23 Sep 2021 at 10:35:19 Opioid peptides: Milk protein Introduction biological activity of opioid peptides because it is reported to maintain the proper orientation of the Tyr and Phe side , subject to the Cambridge Core terms of use, available at Milk proteins are potential sources of opioid agonistic and chains (Mierke et al. 1990). antagonistic peptides. The structures of biologically active Opioid antagonists are peptides related to `atypical' sequences were obtained from in vitro enzymatic and/or by opioid peptides, i.e. they are opioid receptor ligands sharing in vivo gastrointestinal digests of the appropriate precursor several characteristics with agonistic opioid peptides proteins; chemical synthesis has been carried out to confirm derived from milk proteins (Teschemacher et al. 1994). the sequence of potential bioactive peptides (for reviews, They are not found in the sequence of endogenous see Teschemacher et al.