A Rash Starting on the Palms and Soles
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
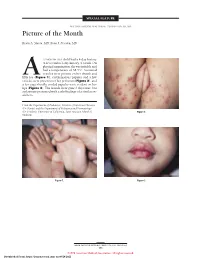
Picture of the Month
SPECIAL FEATURE SECTION EDITOR: WALTER W. TUNNESSEN, JR, MD Picture of the Month Kevin A. Slavin, MD; Ilona J. Frieden, MD 15-MONTH-OLD child had a 4-day history of fever and a 1-day history of a rash. On physical examination she was irritable and had a temperature of 38.3°C. Scattered vesicles were present on her thumb and Afifth toe (Figure 1), erythematous papules and a few vesicles were present over her perineum (Figure 2), and a few superficially eroded papules were evident on her lips (Figure 3). The lesions were gone 3 days later, but a playmate presented with early findings of a similar ex- anthem. From the Department of Pediatrics, Division of Infectious Diseases (Dr Slavin) and the Department of Pediatrics and Dermatology (Dr Frieden), University of California, San Francisco School of Figure 2. Medicine. Figure 1. Figure 3. ARCH PEDIATR ADOLESC MED/ VOL 152, MAY 1998 505 ©1998 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/28/2021 Denouement and Discussion Hand-Foot-and-Mouth Disease Figure 1. Vesicles are present on the thumb and fifth toe. foot-and-mouth disease).1,2,5-9 The lesions on the but- tocks are of the same size and typical of the early forms Figure 2. Multiple erythematous papules and a few scattered vesicles are of the exanthem, but they are not frequently vesicular present over the perineum. in nature. Lesions involving the perineum seem to be more Figure 3. Superficially eroded papules are present on the lips. common in children who wear diapers, suggesting that friction or minor trauma may play a role in the develop- ment of lesions. -

Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet
Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet Hand, foot, and mouth disease is caused by one of several types of viruses Hand, foot, and mouth disease is usually characterized by tiny blisters on the inside of the mouth and the palms of the hands, fingers, soles of the feet. It is commonly caused by coxsackievirus A16 (an enterovirus), and less often by other types of viruses. Anyone can get hand, foot, and mouth disease Young children are primarily affected, but it may be seen in adults. Most cases occur in the summer and early fall. Outbreaks may occur among groups of children especially in child care centers or nursery schools. Symptoms usually appear 3 to 5 days after exposure. Hand, foot, and mouth disease is usually spread through person-to-person contact People can spread the disease when they are shedding the virus in their feces. It is also spread by the respiratory tract from mouth or respiratory secretions (such as from saliva on hands or toys). The virus has also been found in the fluid from the skin blisters. The infection is spread most easily during the acute phase/stage of illness when people are feeling ill, but the virus can be spread for several weeks after the onset of infection. The symptoms are much like a common cold with a rash The rash appears as blisters or ulcers in the mouth, on the inner cheeks, gums, sides of the tongue, and as bumps or blisters on the hands, feet, and sometimes other parts of the skin. The skin rash may last for 7 to 10 days. -

Psoriasis, a Systemic Disease Beyond the Skin, As Evidenced by Psoriatic Arthritis and Many Comorbities
1 Psoriasis, a Systemic Disease Beyond the Skin, as Evidenced by Psoriatic Arthritis and Many Comorbities – Clinical Remission with a Leishmania Amastigotes Vaccine, a Serendipity Finding J.A. O’Daly Astralis Ltd, Irvington, NJ USA 1. Introduction Psoriasis is a systemic chronic, relapsing inflammatory skin disorder, with worldwide distribution, affects 1–3% of the world population, prevalence varies according to race, geographic location, and environmental factors (Chandran & Raychaudhuri, 2010; Christophers & Mrowietz, 2003; Farber & Nall, 1974). In Germany, 33,981 from 1,344,071 continuously insured persons in 2005 were diagnosed with psoriasis; thus the one year prevalence was 2.53% in the study group. Up to the age of 80 years the prevalence rate (range: 3.99-4.18%) was increasing with increasing age and highest for the age groups from 50 to 79 years The total rate of psoriasis in children younger than 18 years was 0.71%. The prevalence rates increased in an approximately linear manner from 0.12% at the age of 1 year to 1.2% at the age of 18 years (Schäfer et al., 2011). In France, a case-control study in 6,887 persons, 356 cases were identified (5.16%), who declared having had psoriasis during the previous 12 months (Wolkenstein et al., 2009). The prevalence of psoriasis analyzed across Italy showed that 2.9% of Italians declared suffering from psoriasis (regional range: 0.8-4.5%) in a total of 4109 individuals (Saraceno et al., 2008). The overall rate of comorbidity in subjects with psoriasis aged less than 20 years was twice as high as in subjects without psoriasis. -

A Resident's Guide to Pediatric Rheumatology
A RESIDENT’S GUIDE TO PEDIATRIC RHEUMATOLOGY 4th Revised Edition - 2019 A RESIDENT’S GUIDE TO PEDIATRIC RHEUMATOLOGY This guide is intended to provide a brief introduction to basic topics in pediatric rheumatology. Each topic is accompanied by at least one up-to-date reference that will allow you to explore the topic in greater depth. In addition, a list of several excellent textbooks and other resources for you to use to expand your knowledge is found in the Appendix. We are interested in your feedback on the guide! If you have comments or questions, please feel free to contact us via email at [email protected]. Supervising Editors: Dr. Ronald M. Laxer, SickKids Hospital, University of Toronto Dr. Tania Cellucci, McMaster Children’s Hospital, McMaster University Dr. Evelyn Rozenblyum, St. Michael’s Hospital, University of Toronto Section Editors: Dr. Michelle Batthish, McMaster Children’s Hospital, McMaster University Dr. Roberta Berard, Children’s Hospital – London Health Sciences Centre, Western University Dr. Liane Heale, McMaster Children’s Hospital, McMaster University Dr. Clare Hutchinson, North York General Hospital, University of Toronto Dr. Mehul Jariwala, Royal University Hospital, University of Saskatchewan Dr. Lillian Lim, Stollery Children’s Hospital, University of Alberta Dr. Nadia Luca, Alberta Children’s Hospital, University of Calgary Dr. Dax Rumsey, Stollery Children’s Hospital, University of Alberta Dr. Gordon Soon, North York General Hospital and SickKids Hospital Northern Clinic in Sudbury, University -

Viral Rashes: New and Old Peggy Vernon, RN, MA, CPNP, DCNP, FAANP C5
Viral Rashes: New and Old Peggy Vernon, RN, MA, CPNP, DCNP, FAANP C5 Disclosures •There are no financial relationships with commercial interests to disclose Viral Rashes: New and Old •Any unlabeled/unapproved uses of drugs or products referenced will be disclosed Peggy Vernon, RN, MA, CPNP, DCNP, FAANP ©Pvernon2021 ©Pvernon2021 Restrictions Objectives • Permission granted to the 2021 National Nurse • Identify a potential sequelae from hand, foot and Practitioner Symposium and its attendees mouth disease • Describe the pattern of distribution and lesion • All rights reserved. No part of this presentation may description of varicella be reproduced, stored, or transmitted in any form or • Identify a precursor of Henoch Schonlein Purpura by any means without written permission of the author •Contact Peggy Vernon at [email protected] ©Pvernon2021 ©Pvernon2021 Viral Exanthems Morbilliform Exanthems •Morbilliform • Measles (rubeola) •Papular-nodular • Rubella •Vesiculobullous • Roseola •Petechial • Erythema Infectiosum •Purpuric • Pityriasis Rosea • Infectious Mono ©Pvernon2021 ©Pvernon2021 1 Viral Rashes: New and Old Peggy Vernon, RN, MA, CPNP, DCNP, FAANP C5 Measles (Rubeola) MEASLES (RUBEOLA) • Prodrome: fever, malaise, cough, DIFFERENTIAL DIAGNOSIS conjunctivitis. Patient appears quite ill •Other morbilliform eruptions: Rubella, • Koplik’s spots: bluish-white erythema infectiosum, pityriasis rosea, elevations on buccal mucosa infectious mono • Exanthem: erythematous •DRUG maculopapular eruption, from scalp to forehead, posterior -

Drug Treatments in Psoriasis
Drug Treatments in Psoriasis Authors: David Gravette, Pharm.D. Candidate, Harrison School of Pharmacy, Auburn University; Morgan Luger, Pharm.D. Candidate, Harrison School of Pharmacy, Auburn University; Jay Moulton, Pharm.D. Candidate, Harrison School of Pharmacy, Auburn University; Wesley T. Lindsey, Pharm.D., Associate Clinical Professor of Pharmacy Practice, Drug Information and Learning Resource Center, Harrison School of Pharmacy, Auburn University Universal Activity #: 0178-0000-13-108-H01-P | 1.5 contact hours (.15 CEUs) Initial Release Date: November 29, 2013 | Expires: April 1, 2016 Alabama Pharmacy Association | 334.271.4222 | www.aparx.org | [email protected] SPRING 2014: CONTINUING EDUCATION |WWW.APARX.Org 1 EducatiONAL OBJECTIVES After the completion of this activity pharmacists will be able to: • Outline how to diagnose psoriasis. • Describe the different types of psoriasis. • Outline nonpharmacologic and pharmacologic treatments for psoriasis. • Describe research on new biologic drugs to be used for the treatment of psoriasis as well as alternative FDA uses for approved drugs. INTRODUCTION depression, and even alcoholism which decreases their quality of Psoriasis is a common immune modulated inflammatory life. It is uncertain why these diseases coincide with one another, disease affecting nearly 17 million people in North America and but it is hypothesized that the chronic inflammatory nature of Europe, which is approximately 2% of the population. The highest psoriasis is the underlying problem. frequencies occur in Caucasians -

A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD)
A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD) WHO Western Pacific Region PUBLICATION ISBN-13 978 92 9061 525 5 A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD) WHO Library Cataloguing in Publication Data A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD) 1. Hand, foot and mouth disease – epidemiology. 2. Hand, foot and mouth disease – prevention and control. [ ii ] 3. Disease outbreaks. 4. Enterovirus A, Human. I. Regional Emerging Disease Intervention Center. ISBN 978 92 9061 525 5 (NLM Classification: WC 500) © World Health Organization 2011 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). For WHO Western Pacific Regional Publications, request for permission to reproduce should be addressed to the Publications Office, World Health Organization, Regional Office for the Western Pacific, P.O. Box 2932, 1000, Manila, Philippines, (fax: +632 521 1036, e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

UC Davis Dermatology Online Journal
UC Davis Dermatology Online Journal Title Proposed classification for koebner, wolf isotopic, renbok, koebner nonreaction, isotopic nonreaction & other related phenomen. Permalink https://escholarship.org/uc/item/96s656b4 Journal Dermatology Online Journal, 20(11) Authors Kannangara, Ajith P Yosipovitch, Gil Fleischer Jr., Alan B Publication Date 2014 DOI 10.5070/D32011024682 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 eScholarship.org Powered by the California Digital Library University of California Volume 20 Number 11 November 2014 Commentary Proposed classification for koebner, wolf isotopic, renbok, koebner nonreaction, isotopic nonreaction & other related phenomen. Ajith P. Kannangara MD1, Gil Yosipovitch MD PhD2, Alan B. Fleischer Jr MD3 Dermatology Online Journal 20 (11): 12 1Base Hospital Balapitiya, Ministry of Health, Sri Lanka 2Department of Dermatology, Temple University School of Medicine, Philadelphia, USA 3Department of Dermatology, Wake Forest University School of Medicine; Winston-Salem, North Carolina, USA Correspondence: Ajith P. Kannangara, M.D Base Hospital Balapitiya, Ministry of Health, Sri Lanka. E-mail: [email protected] Abstract Students of skin diseases have long noted a variety of disease responses and non-responses to trauma and the presence of structural abnormalities. This article will review the series of these responses including: Koebner phenomenon, Wolf isotopic response, Renbök response, Koebner nonreaction, isotopic nonreaction, and other related skin reactions. Because most of these reported phenomena have similar morphological features the diagnosis is often made on the basis of differences in the clinical presentation. Note that some of the cutaneous reactions of similar phenomena have been described using varied nomenclature, further adding to the confusion. -

The Management of Psoriasis in Adults
DORSET MEDICINES ADVISORY GROUP THE MANAGEMENT OF PSORIASIS IN ADULTS Psoriasis is a common, genetically determined, inflammatory and proliferative disorder of the skin, the most characteristic lesions consisting of chronic, sharply demarcated, dull-red, scaly plaques, particularly on the extensor prominences and in the scalp. Self-care advice Many people's psoriasis symptoms start or become worse because of a certain event, known as a trigger. Common triggers include: • an injury to skin such as a cut, scrape, insect bite or sunburn (this is known as the Koebner response) • drinking excessive amounts of alcohol • smoking • stress • hormonal changes, particularly in women (for example during puberty and the menopause) • certain medicines such as lithium, some antimalarial medicines, anti-inflammatory medicines including ibuprofen, ACE inhibitors (used to treat high blood pressure) and beta blockers (used to treat congestive heart failure) • throat infections - in some people, usually children and young adults, a form of psoriasis called guttate psoriasis (which causes smaller pink patches, often without a lot of scaling) develops after a streptococcal throat infection, although most people who have streptococcal throat infections do not develop psoriasis • other immune disorders, such as HIV, which cause psoriasis to flare up or to appear for the first time Advice for patients can be found here Management pathway For people with any type of psoriasis assess: • disease severity • the impact of disease on physical, psychological and social wellbeing • whether they have psoriatic arthritis • the presence of comorbidities. • Consider using the Dermatology quality of life assessment: www.pcds.org.uk/p/quality-of-life Assess the severity and impact of any type of psoriasis: • at first presentation • before referral for specialist advice and at each referral point in the treatment pathway • to evaluate the efficacy of interventions. -

Koebner Phenomenon in Rheumatoid Arthritis
ndrom Sy es tic & e G n e e n G e f T o Yamamoto and Ueki, J Genet Syndr Gene Ther 2013, 4:8 Journal of Genetic Syndromes h l e a r n a r p DOI: 10.4172/2157-7412.1000173 u y o J & Gene Therapy ISSN: 2157-7412 Review Article Open Access Koebner Phenomenon in Rheumatoid Arthritis Yamamoto T1* and Ueki H2 1Department of Dermatology, Fukushima Medical University, Japan 2Department of Dermatology, Kawasaki Medical School, Japan Abstract Koebner phenomenon indicates the newly appearance of isomorphic lesions at the sites of mechanically stimulated or injured skin. This phenomenon can be seen in various inflammatory, auto-immune, viral, fibrotic, and even tumoral disorders. Also, rheumatic diseases such as lupus erythematosus, dermatomyositis, and rheumatoid arthritis (RA) often present with cutaneous manifestations with isomorphic response of Koebner. RA presents with various skin conditions as extra-articular manifestations. Rheumatoid nodule is the representative specific skin lesion which frequently occurs on the hand, elbow, sole, sacrum, occipital area, and so on. These sites are susceptible to both outer and inner mechanical stress. Rheumatoid nodules involve not only skin but internal tissues such as spine, lung, heart valves, and gastrointestinal tract, which are also susceptible to mechanical stress. This isomorphic response may be induced at deeper levels than skin, and thus considered to be “deep” or “internal” Koebner phenomenon. Other than rheumatoid nodules, several specific skin conditions are associated with RA, such as palisaded neutrophilic granulomatous dermatitis and rheumatoid neutrophilic dermatitis, which can be seen on the fingers, elbows, knees and sole. -
Guidelines for Occupational Health Follow up of Communicable Diseases for Manager/Supervisors
Winnipeg Regional Health Authority Occupational and Environmental Safety & Health (OESH) Guidelines for Occupational Health Follow Up of Communicable Diseases For Manager/Supervisors Page | 1 2019.02.04 version 2 Winnipeg Regional Health Authority Occupational and Environmental Safety & Health (OESH) INTRODUCTION ................................................................................................................................................................................. 3 WORKERS COMPENSATION BOARD (WCB) CLAIMS ........................................................................................................................... 5 ANTIBIOTIC RESISTANT ORGANISMS (AROS) ..................................................................................................................................... 6 BLOOD AND BODY FLUID EXPOSURES ............................................................................................................................................... 9 CIMEX LECTULARIUS (BED BUGS) .................................................................................................................................................... 10 CREUTZFELDT-JAKOB DISEASE (CJD) ................................................................................................................................................ 11 DIARRHEA (BACTERIAL, CLOSTRIDIUM DIFFICILE (C. DIFFICILE), VIRAL) ........................................................................................... 12 GROUP A STREPTOCOCCUS ............................................................................................................................................................ -

Hand-Foot-And-Mouth Disease Caused by Coxsackievirus A6 on the Rise
Hand-foot-and-mouth Disease Caused by Coxsackievirus A6 on the Rise Brooks David Kimmis, MD; Christopher Downing, MD; Stephen Tyring, MD, PhD CVA16 has traditionally been the primary strain caus- PRACTICE POINTS ing HFMD, CVA6 has become a major cause of HFMD • Coxsackievirus A6 is an increasingly more common outbreaks in the United States and worldwide in recent cause of hand-foot-and-mouth disease (HFMD), years.6-12 Interestingly, CVA6 also has been found to be often with atypical presentation, more severe disease, associated with adult HFMD, which has increased in and association with HFMD in adults. incidence. The CVA6 strain was first identified in associa- • Coxsackievirus A6 has become a major cause of tion with the disease during HFMD outbreaks in Finland HFMD outbreak in the United States and worldwide. and Singapore in 2008,13,14 with similar strains detected in subsequent outbreaks in Taiwan, Japan, Spain, France, China, India, and the United States.12,15-25 Most cases took place in warmer months, with one winter outbreak in Hand-foot-and-mouth disease (HFMD) is a viral illness caused Massachusetts in 2012.24 most commonly by coxsackievirus A16 (CVA16) and enterovirus 71 (EV71). The disease mainly affects pediatric populations younger Herein, we review the incidence of CVA6, as well as than 5 years and is characterized by lesions of the oral mucosa, its atypical presentation, diagnosis, and treatment to aid palms, and soles, lasting for 7 to 10 days. In recent years, CVA6 has dermatologists. Given the increasing incidence of HFMD become a major cause of HFMD outbreaks in the United States and caused by CVA6 and its often atypical presentation, it is worldwide.