Clinical Anatomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A Study of Occurrence and Types of Suprameatal Spines in the Suprameatal Triangle
ISSN: 2455-2631 © March 2021 IJSDR | Volume 6, Issue 3 A STUDY OF OCCURRENCE AND TYPES OF SUPRAMEATAL SPINES IN THE SUPRAMEATAL TRIANGLE Preetha Parthasarathy Under graduate SIMATS Saveetha Dental College, 162, Poonamalle high road, Velappanchavadi, Chennai- 600095. India. Mrs. M.S. Thenmozhi Dept of Anatomy SIMATS Saveetha Dental College, 162, Poonamalle high road, Velappanchavadi, Chennai- 600095. India. Corresponding author: Mrs. Thenmozhi. M.S Dept of anatomy SIMATS Saveetha dental college, Velappanchavadi Chennai-600095 India Running title: Types of suprameatal spines ABSTRACT: AIM: To identify the occurrence and types of suprameatal spines on either sides of the skull in the suprameatal triangle and to study their clinic implications. OBJECTIVE: To figure out the presence of suprameatal spines in the suprameatal triangle and to review the literature on anatomical and clinic aspects of suprameatal triangle. INTRODUCTION: Suprameatal triangle is present between the posterior wall of external acoustic meatus and posterior root of zygomatic process, in the temporal bone. It is also called as Macewen’s triangle. Suprameatal spine is seen below the upper limit of the orifice of the inner end of external acoustic meatus which is closed by tympanic membrane. It is also called as spine of Henle. RESULT: From the above conducted study, it can be seen that, when the suprameatal spines were evaluated according to its type and occurrence, the crest type of spine present was more than the triangle type. The crest type of spine was found to be 62.2% and the triangle type of spine was about 37.8% CONCLUSION: Thus, this study shows the prevalence of crest and triangle type spine in the dry skulls evaluated. -

Gross Anatomy Assignment Name: Olorunfemi Peace Toluwalase Matric No: 17/Mhs01/257 Dept: Mbbs Course: Gross Anatomy of Head and Neck
GROSS ANATOMY ASSIGNMENT NAME: OLORUNFEMI PEACE TOLUWALASE MATRIC NO: 17/MHS01/257 DEPT: MBBS COURSE: GROSS ANATOMY OF HEAD AND NECK QUESTION 1 Write an essay on the carvernous sinus. The cavernous sinuses are one of several drainage pathways for the brain that sits in the middle. In addition to receiving venous drainage from the brain, it also receives tributaries from parts of the face. STRUCTURE ➢ The cavernous sinuses are 1 cm wide cavities that extend a distance of 2 cm from the most posterior aspect of the orbit to the petrous part of the temporal bone. ➢ They are bilaterally paired collections of venous plexuses that sit on either side of the sphenoid bone. ➢ Although they are not truly trabeculated cavities like the corpora cavernosa of the penis, the numerous plexuses, however, give the cavities their characteristic sponge-like appearance. ➢ The cavernous sinus is roofed by an inner layer of dura matter that continues with the diaphragma sellae that covers the superior part of the pituitary gland. The roof of the sinus also has several other attachments. ➢ Anteriorly, it attaches to the anterior and middle clinoid processes, posteriorly it attaches to the tentorium (at its attachment to the posterior clinoid process). Part of the periosteum of the greater wing of the sphenoid bone forms the floor of the sinus. ➢ The body of the sphenoid acts as the medial wall of the sinus while the lateral wall is formed from the visceral part of the dura mater. CONTENTS The cavernous sinus contains the internal carotid artery and several cranial nerves. Abducens nerve (CN VI) traverses the sinus lateral to the internal carotid artery. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

Lab Manual Axial Skeleton Atla
1 PRE-LAB EXERCISES When studying the skeletal system, the bones are often sorted into two broad categories: the axial skeleton and the appendicular skeleton. This lab focuses on the axial skeleton, which consists of the bones that form the axis of the body. The axial skeleton includes bones in the skull, vertebrae, and thoracic cage, as well as the auditory ossicles and hyoid bone. In addition to learning about all the bones of the axial skeleton, it is also important to identify some significant bone markings. Bone markings can have many shapes, including holes, round or sharp projections, and shallow or deep valleys, among others. These markings on the bones serve many purposes, including forming attachments to other bones or muscles and allowing passage of a blood vessel or nerve. It is helpful to understand the meanings of some of the more common bone marking terms. Before we get started, look up the definitions of these common bone marking terms: Canal: Condyle: Facet: Fissure: Foramen: (see Module 10.18 Foramina of Skull) Fossa: Margin: Process: Throughout this exercise, you will notice bold terms. This is meant to focus your attention on these important words. Make sure you pay attention to any bold words and know how to explain their definitions and/or where they are located. Use the following modules to guide your exploration of the axial skeleton. As you explore these bones in Visible Body’s app, also locate the bones and bone markings on any available charts, models, or specimens. You may also find it helpful to palpate bones on yourself or make drawings of the bones with the bone markings labeled. -

Macroscopic Anatomy of the Nasal Cavity and Paranasal Sinuses of the Domestic Pig (Sus Scrofa Domestica) Daniel John Hillmann Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1971 Macroscopic anatomy of the nasal cavity and paranasal sinuses of the domestic pig (Sus scrofa domestica) Daniel John Hillmann Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Animal Structures Commons, and the Veterinary Anatomy Commons Recommended Citation Hillmann, Daniel John, "Macroscopic anatomy of the nasal cavity and paranasal sinuses of the domestic pig (Sus scrofa domestica)" (1971). Retrospective Theses and Dissertations. 4460. https://lib.dr.iastate.edu/rtd/4460 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. 72-5208 HILLMANN, Daniel John, 1938- MACROSCOPIC ANATOMY OF THE NASAL CAVITY AND PARANASAL SINUSES OF THE DOMESTIC PIG (SUS SCROFA DOMESTICA). Iowa State University, Ph.D., 1971 Anatomy I University Microfilms, A XEROX Company, Ann Arbor. Michigan I , THIS DISSERTATION HAS BEEN MICROFILMED EXACTLY AS RECEIVED Macroscopic anatomy of the nasal cavity and paranasal sinuses of the domestic pig (Sus scrofa domestica) by Daniel John Hillmann A Dissertation Submitted to the Graduate Faculty in Partial Fulfillment of The Requirements for the Degree of DOCTOR OF PHILOSOPHY Major Subject: Veterinary Anatomy Approved: Signature was redacted for privacy. h Charge of -^lajoï^ Wor Signature was redacted for privacy. For/the Major Department For the Graduate College Iowa State University Ames/ Iowa 19 71 PLEASE NOTE: Some Pages have indistinct print. -

Surgical Management of Posterior Petrous Meningiomas
Neurosurg Focus 14 (6):Article 7, 2003, Click here to return to Table of Contents Surgical management of posterior petrous meningiomas JAMES K. LIU, M.D., OREN N. GOTTFRIED, M.D., AND WILLIAM T. COULDWELL, M.D., PH.D. Department of Neurosurgery, University of Utah School of Medicine, Salt Lake City, Utah Posterior petrous meningiomas (commonly termed posterior pyramid meningiomas and/or meningiomas of the pos- terior surface of the petrous pyramid) are the most common meningiomas of the posterior cranial fossa. They are locat- ed along the posterior surface of the temporal bone in the region of the cerebellopontine angle. They often mimic vestibular schwannomas, both clinically and on neuroimaging studies. Common clinical symptoms include hearing loss, cerebellar ataxia, and trigeminal neuropathy. The site of dural origin determines the direction of cranial nerve dis- placement. Total resection can be achieved in most cases with a low morbidity rate and an excellent prognosis. The authors review the surgical management of posterior petrous meningiomas. KEY WORDS • meningioma • cerebellopontine angle • skull base surgery • petrous bone Posterior fossa meningiomas comprise approximately In their series Samii and Ammirati18 used the term “pos- 10% of all intracranial meningiomas.8 Castellano and terior pyramid meningiomas” and defined them as tumors Ruggiero4 reviewed Olivecrona’s experience with treat- whose main direction of growth brings them in contact ing posterior fossa meningiomas and classified them with the posterior pyramid, irrespective of their site of based on the site of dural attachment. They described the dural attachment. They also designated those located ante- location as cerebellar convexity (10%), tentorium (30%), rior and those posterior to the internal acoustic meatus. -

The Braincase of Two Late Cretaceous Asian Multituberculates Studied by Serial Sections
The braincase of two Late Cretaceous Asian multituberculates studied by serial sections J0RN H. HURUM Hurum, J.H. 1998. The braincase of two Late Cretaceous Asian multituberculatesstudied by serial sections. -Acta Palaeontologica Polonica 43, 1, 21-52. The braincase structure of two Late Cretaceous Mongolian djadochtatherian multituber- culates Nemegtbaatar gobiensis and Chulsanbaatar vulgaris from the ?late Campanian of Mongolia is presented based on the two serially sectioned skulls and additional specimens. Reconstructions of the floor of the braincase in both taxa are given. The complete intracranial sphenoid region is reconstructed for the first time in multitubercu- lates. Cavum epiptericum is a separate space with the taenia clino-orbitalis (ossified pila antotica) as the medial wall, anterior lamina of the petrosal and possibly the alisphenoid as the lateral wall, and the basisphenoid, petrosal and possibly alisphenoid ventrally. The fovea hypochiasmatica is shallow, tuberculurn sellae is wide and more raised from the skull base than it is in the genus Pseudobolodon. The dorsal opening of the carotid canal is situated in the fossa hypophyseos. The taenia clino-orbitalis differs from the one described in Pseudobolodon and Lambdopsalis in possessing just one foramen (metoptic foramen). Compared to all extant mammals the braincase in Nemegtbaatar and Chulsan- baatar is primitive in that both the pila antotica and pila metoptica are retained. In both genera the anterior lamina of the petrosal is large with a long anterodorsal process while the alisphenoid is small. A review is given of the cranial anatomy in Nemegtbaatar and Chulsanbaatar. K e y w o r d s : Braincase structure, sphenoid complex, cavum epiptericum,Mammalia, Multituberculata,Djadochtatheria, Cretaceous, Mongolia. -

Macewen'striangle
European Journal of Molecular & Clinical Medicine ISSN 2515-8260 Volume 07, Issue 5, 2020 MacEwen’sTriangle- A Review Dr. Bhaskaran Sathyapriya, Professor, Department of Anatomy, Sree Balaji Dental College & Hospital, Bharath Institute of Higher Education & Research, Chennai Chandrakala B1, Govindarajan Sumathy2, Syed FazilHasan 3, Priyadharshini.M3, Srilakshmi.B 3,Bhaskaran Sathyapriya* 1. Senior Lecturer, Department of Anatomy, Sree Balaji Dental College & Hospital, Bharath Institute of Higher Education & Research, Chennai. 2. Professor and Head, Department of Anatomy, Sree Balaji Dental College & Hospital, Bharath Institute of Higher Education & Research, Chennai. 3. Graduate student, Sree Balaji Dental College and Hospital, Bharath Institute of Higher Education and Research *Professor, Department of Anatomy, Sree Balaji Dental College & Hospital, Bharath Institute of Higher Education & Research, Chennai. Abstract In the temporal bone, between the posterior wall of the external acoustic meatus and the posterior root of the zygomatic process is the area called the suprameatal triangle, suprameatal pit, mastoid fossa, foveolasuprameatica, or Mac Ewen's triangle, through which an instrument may be pushed into the mastoid antrum..In the adult, the antrum lies approximately 1.5 to 2 cm deep to the suprameatal triangle. This is an important landmark when performing a cortical mastoidectomy. The triangle lies deep to the cymba conchae.The sex determination of unknown human skulls can be evaluated by using the measurement of the area formed by the xerographic projection of 3craniometric points related to the mastoid process: the porion, asterion, and mastoidale points. Keywords: MacEwen's triangle,mastoidectomy,suprameatal spine,Mastoid antrum ,sex determination,zygomatic process,mastoid process. Introduction MacEwen's triangle is a very important surgical landmark for the mastoid antrum or the largest mastoid air cell.[9] It is also known as Suprameatal triangle or Mastoid fossa.[4] The suprameataltrigone plays a big role in the aspect of clinics. -

Atlas of the Facial Nerve and Related Structures
Rhoton Yoshioka Atlas of the Facial Nerve Unique Atlas Opens Window and Related Structures Into Facial Nerve Anatomy… Atlas of the Facial Nerve and Related Structures and Related Nerve Facial of the Atlas “His meticulous methods of anatomical dissection and microsurgical techniques helped transform the primitive specialty of neurosurgery into the magnificent surgical discipline that it is today.”— Nobutaka Yoshioka American Association of Neurological Surgeons. Albert L. Rhoton, Jr. Nobutaka Yoshioka, MD, PhD and Albert L. Rhoton, Jr., MD have created an anatomical atlas of astounding precision. An unparalleled teaching tool, this atlas opens a unique window into the anatomical intricacies of complex facial nerves and related structures. An internationally renowned author, educator, brain anatomist, and neurosurgeon, Dr. Rhoton is regarded by colleagues as one of the fathers of modern microscopic neurosurgery. Dr. Yoshioka, an esteemed craniofacial reconstructive surgeon in Japan, mastered this precise dissection technique while undertaking a fellowship at Dr. Rhoton’s microanatomy lab, writing in the preface that within such precision images lies potential for surgical innovation. Special Features • Exquisite color photographs, prepared from carefully dissected latex injected cadavers, reveal anatomy layer by layer with remarkable detail and clarity • An added highlight, 3-D versions of these extraordinary images, are available online in the Thieme MediaCenter • Major sections include intracranial region and skull, upper facial and midfacial region, and lower facial and posterolateral neck region Organized by region, each layered dissection elucidates specific nerves and structures with pinpoint accuracy, providing the clinician with in-depth anatomical insights. Precise clinical explanations accompany each photograph. In tandem, the images and text provide an excellent foundation for understanding the nerves and structures impacted by neurosurgical-related pathologies as well as other conditions and injuries. -

Topographical Anatomy and Morphometry of the Temporal Bone of the Macaque
Folia Morphol. Vol. 68, No. 1, pp. 13–22 Copyright © 2009 Via Medica O R I G I N A L A R T I C L E ISSN 0015–5659 www.fm.viamedica.pl Topographical anatomy and morphometry of the temporal bone of the macaque J. Wysocki 1Clinic of Otolaryngology and Rehabilitation, II Medical Faculty, Warsaw Medical University, Poland, Kajetany, Nadarzyn, Poland 2Laboratory of Clinical Anatomy of the Head and Neck, Institute of Physiology and Pathology of Hearing, Poland, Kajetany, Nadarzyn, Poland [Received 7 July 2008; Accepted 10 October 2008] Based on the dissections of 24 bones of 12 macaques (Macaca mulatta), a systematic anatomical description was made and measurements of the cho- sen size parameters of the temporal bone as well as the skull were taken. Although there is a small mastoid process, the general arrangement of the macaque’s temporal bone structures is very close to that which is observed in humans. The main differences are a different model of pneumatisation and the presence of subarcuate fossa, which possesses considerable dimensions. The main air space in the middle ear is the mesotympanum, but there are also additional air cells: the epitympanic recess containing the head of malleus and body of incus, the mastoid cavity, and several air spaces on the floor of the tympanic cavity. The vicinity of the carotid canal is also very well pneuma- tised and the walls of the canal are very thin. The semicircular canals are relatively small, very regular in shape, and characterized by almost the same dimensions. The bony walls of the labyrinth are relatively thin. -
The Axial Skeleton Visual Worksheet
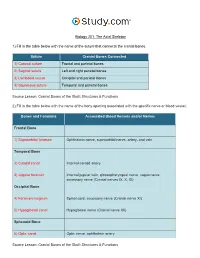
Biology 201: The Axial Skeleton 1) Fill in the table below with the name of the suture that connects the cranial bones. Suture Cranial Bones Connected 1) Coronal suture Frontal and parietal bones 2) Sagittal suture Left and right parietal bones 3) Lambdoid suture Occipital and parietal bones 4) Squamous suture Temporal and parietal bones Source Lesson: Cranial Bones of the Skull: Structures & Functions 2) Fill in the table below with the name of the bony opening associated with the specific nerve or blood vessel. Bones and Foramina Associated Blood Vessels and/or Nerves Frontal Bone 1) Supraorbital foramen Ophthalmic nerve, supraorbital nerve, artery, and vein Temporal Bone 2) Carotid canal Internal carotid artery 3) Jugular foramen Internal jugular vein, glossopharyngeal nerve, vagus nerve, accessory nerve (Cranial nerves IX, X, XI) Occipital Bone 4) Foramen magnum Spinal cord, accessory nerve (Cranial nerve XI) 5) Hypoglossal canal Hypoglossal nerve (Cranial nerve XII) Sphenoid Bone 6) Optic canal Optic nerve, ophthalmic artery Source Lesson: Cranial Bones of the Skull: Structures & Functions 3) Label the anterior view of the skull below with its correct feature. Frontal bone Palatine bone Ethmoid bone Nasal septum: Perpendicular plate of ethmoid bone Sphenoid bone Inferior orbital fissure Inferior nasal concha Maxilla Orbit Vomer bone Supraorbital margin Alveolar process of maxilla Middle nasal concha Inferior nasal concha Coronal suture Mandible Glabella Mental foramen Nasal bone Parietal bone Supraorbital foramen Orbital canal Temporal bone Lacrimal bone Orbit Alveolar process of mandible Superior orbital fissure Zygomatic bone Infraorbital foramen Source Lesson: Facial Bones of the Skull: Structures & Functions 4) Label the right lateral view of the skull below with its correct feature. -

Modern Surgery, 4Th Edition, by John Chalmers Da Costa Rare Medical Books
Thomas Jefferson University Jefferson Digital Commons Modern Surgery, 4th edition, by John Chalmers Da Costa Rare Medical Books 1903 Modern Surgery - Chapter 23. Diseases and Injuries of the Head John Chalmers Da Costa Jefferson Medical College Follow this and additional works at: https://jdc.jefferson.edu/dacosta_modernsurgery Part of the History of Science, Technology, and Medicine Commons Let us know how access to this document benefits ouy Recommended Citation Da Costa, John Chalmers, "Modern Surgery - Chapter 23. Diseases and Injuries of the Head" (1903). Modern Surgery, 4th edition, by John Chalmers Da Costa. Paper 29. https://jdc.jefferson.edu/dacosta_modernsurgery/29 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Modern Surgery, 4th edition, by John Chalmers Da Costa by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Diseases of the Head 595 XXIII. DISEASES AND INJURIES OF THE HEAD. I. DISEASES OF I:: HEAD. IN approaching a case of brain disorder, first endeavor to locate the seat of the trouble; next, ascertain the nature of the lesion; and, finally, deter- mine the best plan of treatment, operative or otherwise.