Pharmacogenomics of CYP2C9: Functional and Clinical Considerations†
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Impaired Hepatic Drug and Steroid Metabolism in Congenital Adrenal
European Journal of Endocrinology (2010) 163 919–924 ISSN 0804-4643 CLINICAL STUDY Impaired hepatic drug and steroid metabolism in congenital adrenal hyperplasia due to P450 oxidoreductase deficiency Dorota Tomalik-Scharte1, Dominique Maiter2, Julia Kirchheiner3, Hannah E Ivison, Uwe Fuhr1 and Wiebke Arlt School of Clinical and Experimental Medicine, Centre for Endocrinology, Diabetes and Metabolism (CEDAM), University of Birmingham, Birmingham B15 2TT, UK, 1Department of Pharmacology, University Hospital, University of Cologne, 50931 Cologne, Germany, 2Department of Endocrinology, University Hospital Saint Luc, 1200 Brussels, Belgium and 3Department of Pharmacology of Natural Products and Clinical Pharmacology, University of Ulm, 89019 Ulm, Germany (Correspondence should be addressed to W Arlt; Email: [email protected]) Abstract Objective: Patients with congenital adrenal hyperplasia due to P450 oxidoreductase (POR) deficiency (ORD) present with disordered sex development and glucocorticoid deficiency. This is due to disruption of electron transfer from mutant POR to microsomal cytochrome P450 (CYP) enzymes that play a key role in glucocorticoid and sex steroid synthesis. POR also transfers electrons to all major drug- metabolizing CYP enzymes, including CYP3A4 that inactivates glucocorticoid and oestrogens. However, whether ORD results in impairment of in vivo drug metabolism has never been studied. Design: We studied an adult patient with ORD due to homozygous POR A287P, the most frequent POR mutation in Caucasians, and her clinically unaffected, heterozygous mother. The patient had received standard dose oestrogen replacement from 17 until 37 years of age when it was stopped after she developed breast cancer. Methods: Both subjects underwent in vivo cocktail phenotyping comprising the oral administration of caffeine, tolbutamide, omeprazole, dextromethorphan hydrobromide and midazolam to assess the five major drug-metabolizing CYP enzymes. -

NIH Public Access Author Manuscript Pharmacogenet Genomics
NIH Public Access Author Manuscript Pharmacogenet Genomics. Author manuscript; available in PMC 2013 February 01. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Pharmacogenet Genomics. 2012 February ; 22(2): 159–165. doi:10.1097/FPC.0b013e32834d4962. PharmGKB summary: very important pharmacogene information for cytochrome P450, family 2, subfamily C, polypeptide 19 Stuart A. Scotta, Katrin Sangkuhlc, Alan R. Shuldinere,f, Jean-Sébastien Hulotb,g, Caroline F. Thornc, Russ B. Altmanc,d, and Teri E. Kleinc aDepartment of Genetics and Genomic Sciences bCardiovascular Research Center, Mount Sinai School of Medicine, New York, New York cDepartments of Genetics dBioengineering, Stanford University, Stanford, California eDivision of Endocrinology, Diabetes and Nutrition, University of Maryland School of Medicine fGeriatric Research and Education Clinical Center, Veterans Administration Medical Center, Baltimore, Maryland, USA gDepartment of Pharmacology, Université Pierre et Marie Curie-Paris 6, INSERM UMR S 956, Pitié-Salpêtrière University Hospital, Paris, France Abstract This PharmGKB summary briefly discusses the CYP2C19 gene and current understanding of its function, regulation, and pharmacogenomic relevance. Keywords antidepressants; clopidogrel; CYP2C19*17; CYP2C19*2; CYP2C19; proton pump inhibitors; rs4244285 Introduction The cytochrome P450, family 2, subfamily C, polypeptide 19 (CYP2C19) gene is located within a cluster of cytochrome P450 genes (centromere-CYP2C18-CYP2C19-CYP2C9- CYP2C8-telomere) on chromosome 10q23.33. The CYP2C19 enzyme contributes to the metabolism of a large number of clinically relevant drugs and drug classes such as antidepressants [1], benzodiazepines [2], mephenytoin [3], proton pump inhibitors (PPIs) [4], and the antiplatelet prodrug clopidogrel [5]. Similar to other CYP450 genes, inherited genetic variation in CYP2C19 and its variable hepatic expression contributes to the interindividual phenotypic variability in CYP2C19 substrate metabolism. -

Identification and Characterization of CYP2C18 in the Cynomolgus Macaque (Macaca Fascicularis)
NOTE Toxicology Identification and Characterization of CYP2C18 in the Cynomolgus Macaque (Macaca fascicularis) Yasuhiro UNO1)*, Kiyomi MATSUNO1), Chika NAKAMURA1), Masahiro UTOH1) and Hiroshi YAMAZAKI2) 1)Pharmacokinetics and Bioanalysis Center (PBC), Shin Nippon Biomedical Laboratories (SNBL), Kainan, Wakayama 642–0017 and 2)Laboratory of Drug Metabolism and Pharmacokinetics, Showa Pharmaceutical University, Machida, Tokyo 194–8543, Japan (Received 3 August 2009/Accepted 15 September 2009/Published online in J-STAGE 25 November 2009) ABSTRACT. The macaque is widely used for investigation of drug metabolism due to its evolutionary closeness to the human. However, the genetic backgrounds of drug-metabolizing enzymes have not been fully investigated; therefore, identification and characterization of drug-metabolizing enzyme genes are important for understanding drug metabolism in this species. In this study, we isolated and char- acterized a novel cytochrome P450 2C18 (CYP2C18) cDNA in cynomolgus macaques. This cDNA was highly homologous (96%) to human CYP2C18 cDNA. Cynomolgus CYP2C18 was preferentially expressed in the liver and kidney. Moreover, a metabolic assay using cynomolgus CYP2C18 protein heterologously expressed in Escherichia coli revealed its activity toward S-mephenytoin 4’-hydrox- ylation. These results suggest that cynomolgus CYP2C18 could function as a drug-metabolizing enzyme in the liver. KEY WORDS: cloning, CYP2C18, cytochrome P450, liver, monkey. J. Vet. Med. Sci. 72(2): 225–228, 2010 Cytochrome P450 (CYP) is a superfamily of some of the Such species differences also could be explained by func- most important drug-metabolizing enzymes and consists of tional disparity of the orthologous CYPs between the two a large number of subfamilies [14]. In humans, the CYP2C species, such as, if an ortholog to human CYP with low (or subfamilies contain important enzymes that metabolize no) expression and drug-metabolizing activity, for example approximately 20% of all prescribed drugs [3]. -

Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid
Comprehensive Summaries of Uppsala Dissertations from the Faculty of Pharmacy 231 _____________________________ _____________________________ Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21 BY JOHAN BYLUND ACTA UNIVERSITATIS UPSALIENSIS UPPSALA 2000 Dissertation for the Degree of Doctor of Philosophy (Faculty of Pharmacy) in Pharmaceutical Pharmacology presented at Uppsala University in 2000 ABSTRACT Bylund, J. 2000. Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid: Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21. Acta Universitatis Upsaliensis. Comprehensive Summaries of Uppsala Dissertations from Faculty of Pharmacy 231 50 pp. Uppsala. ISBN 91-554-4784-8. Cytochrome P450 (P450 or CYP) is an enzyme system involved in the oxygenation of a wide range of endogenous compounds as well as foreign chemicals and drugs. This thesis describes investigations of P450-catalyzed oxygenation of prostaglandins, linoleic and arachidonic acids. The formation of bisallylic hydroxy metabolites of linoleic and arachidonic acids was studied with human recombinant P450s and with human liver microsomes. Several P450 enzymes catalyzed the formation of bisallylic hydroxy metabolites. Inhibition studies and stereochemical analysis of metabolites suggest that the enzyme CYP1A2 may contribute to the biosynthesis of bisallylic hydroxy fatty acid metabolites in adult human liver microsomes. 19R-Hydroxy-PGE and 20-hydroxy-PGE are major components of human and ovine semen, respectively. They are formed in the seminal vesicles, but the mechanism of their biosynthesis is unknown. Reverse transcription-polymerase chain reaction using degenerate primers for mammalian CYP4 family genes, revealed expression of two novel P450 genes in human and ovine seminal vesicles. -

Pgx - Cytochrome P450 2C19 (CYP2C19)
PGx - Cytochrome P450 2C19 (CYP2C19) This assay is used to identify patients who may be at risk for altered metabolism of drugs that are modified by CYP2C19. Cytochrome P450 (CYP) isozyme 2C19 is responsible for phase I metabloism of about 40% of drugs including: clopidogrel, phenytoin, diazepam, R-warfarin, tamoxifen, some antidepressants, proton pump inhibitors, and antimalarials. Testing Method and Background This test utilizes the eSensor® 2C19 Genotyping Test is an in vitro diagnostic for the detection and genotyping a panel of variants involved with enzyme metabolism using isolated genomic DNA. The eSensor® technology uses a solid-phase electrochemical method for determining the genotyping status. The eSensor® 2C19 Genotyping Test is for research use only (RUO). CYP2C19 drug metabolism varies among individuals depending on specific genotype. The CYP2 family has many single- nucleotide polymorphisms (SNPs). CYP2C19 gene is located on chromosome 10q23.33 and is highly polymorphic, which can lead to large individual variation in CYP2C19 enzyme activity and related drug response phenotypes and/or undesired adverse drug events. Specifically, the CYP2C19 gene has more than 34 variant alleles identified, which in turn affects the pharmacokinetics of many drugs. Highlights of PGx - Cytochrome P450 2C19 (CYP2C19) Targeted Region CYP2C19: Detects 11 variants/polymorphisms 681G>A (*2) 636G>A (*3) 1A>G (*4) 1297C>T (*5) 395G>A (*6) 19294T>A (*7) 358T>C (*8) 431G>A (*9) 680C>T (*10) 1228C>T (*13) -806C>T (*17) Ordering Information Get started -

Anti-Ulcer Efficacy of Soluble Epoxide Hydrolase Inhibitor TPPU on Diclofenac-Induced Intestinal Ulcers S
Supplemental material to this article can be found at: http://jpet.aspetjournals.org/content/suppl/2016/03/17/jpet.116.232108.DC1 1521-0103/357/3/529–536$25.00 http://dx.doi.org/10.1124/jpet.116.232108 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 357:529–536, June 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Anti-Ulcer Efficacy of Soluble Epoxide Hydrolase Inhibitor TPPU on Diclofenac-Induced Intestinal Ulcers s Sumanta Kumar Goswami, Debin Wan, Jun Yang, Carlos A. Trindade da Silva, Christophe Morisseau, Sean D. Kodani, Guang-Yu Yang, Bora Inceoglu, and Bruce D. Hammock Department of Entomology and Nematology, and Comprehensive Cancer Center (S.K.G., D.W., J.Y., C.A.T.S., C.M., S.D.K., B.I., B.D.H.), University of California–Davis, Davis, California; Department of Genetics and Biochemistry (C.A.T.S.), Federal University of Uberlandia, Uberlandia, Minas Gerais, Brazil; Department of Pathology (G.-Y.Y.), Feinberg School of Medicine, Northwestern University, Chicago, Illinois Downloaded from Received January 13, 2016; accepted March 16, 2016 ABSTRACT Proton pump inhibitors such as omeprazole (OME) reduce the with OME (20 mg/kg, PO). In addition, the effect of treatment was severity of gastrointestinal (GI) ulcers induced by nonsteroidal studied on levels of Hb in blood, EETs in plasma, inflammatory jpet.aspetjournals.org anti-inflammatory drugs (NSAIDs) but can also increase the markers such as myeloperoxidase (MPO) in intestinal tissue chance of dysbiosis. The aim of this study was to test the homogenates, and tissue necrosis factor-a (TNF-a) in serum. -

Polymorphic Human Sulfotransferase 2A1 Mediates the Formation of 25-Hydroxyvitamin
Supplemental material to this article can be found at: http://dmd.aspetjournals.org/content/suppl/2018/01/17/dmd.117.078428.DC1 1521-009X/46/4/367–379$35.00 https://doi.org/10.1124/dmd.117.078428 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 46:367–379, April 2018 Copyright ª 2018 by The American Society for Pharmacology and Experimental Therapeutics Polymorphic Human Sulfotransferase 2A1 Mediates the Formation of 25-Hydroxyvitamin D3-3-O-Sulfate, a Major Circulating Vitamin D Metabolite in Humans s Timothy Wong, Zhican Wang, Brian D. Chapron, Mizuki Suzuki, Katrina G. Claw, Chunying Gao, Robert S. Foti, Bhagwat Prasad, Alenka Chapron, Justina Calamia, Amarjit Chaudhry, Erin G. Schuetz, Ronald L. Horst, Qingcheng Mao, Ian H. de Boer, Timothy A. Thornton, and Kenneth E. Thummel Departments of Pharmaceutics (T.W., Z.W., B.D.C., M.S., K.G.C., C.G., B.P., Al.C., J.C., Q.M., K.E.T.), Medicine and Kidney Research Institute (I.H.d.B.), and Biostatistics (T.A.T.), University of Washington, Seattle, Washington; Department of Pharmacokinetics and Drug Metabolism, Amgen Inc., South San Francisco, California (Z.W.); Department of Pharmacokinetics and Drug Metabolism, Amgen Inc., Cambridge, Massachusetts (R.S.F.); St. Jude Children’s Research Hospital, Memphis, Tennessee Downloaded from (Am.C., E.G.S.); and Heartland Assays LLC, Ames, Iowa (R.L.H.) Received September 1, 2017; accepted January 10, 2018 ABSTRACT dmd.aspetjournals.org Metabolism of 25-hydroxyvitamin D3 (25OHD3) plays a central role in with the rates of dehydroepiandrosterone sulfonation. Further analysis regulating the biologic effects of vitamin D in the body. -

Inhibition of Cytochrome P450 2C8-Mediated Drug Metabolism by the Flavonoid Diosmetin
Drug Metab. Pharmacokinet. 26 (6): 559568 (2011). Copyright © 2011 by the Japanese Society for the Study of Xenobiotics (JSSX) Regular Article Inhibition of Cytochrome P450 2C8-mediated Drug Metabolism by the Flavonoid Diosmetin Luigi QUINTIERI1,PietroPALATINI1,StefanoMORO2 and Maura FLOREANI1,* 1Department of Pharmacology and Anaesthesiology, University of Padova, Italy 2Molecular Modeling Section (MMS), Department of Pharmaceutical Sciences, University of Padova, Italy Full text of this paper is available at http://www.jstage.jst.go.jp/browse/dmpk Summary: The aim of this study was to assess the effects of diosmetin and hesperetin, two flavonoids present in various medicinal products, on CYP2C8 activity of human liver microsomes using paclitaxel oxidation to 6¡-hydroxy-paclitaxel as a probe reaction. Diosmetin and hesperetin inhibited 6¡-hydroxy- paclitaxel production in a concentration-dependent manner, diosmetin being about 16-fold more potent than hesperetin (mean IC50 values 4.25 « 0.02 and 68.5 « 3.3 µM for diosmetin and hesperetin, respectively). Due to the low inhibitory potency of hesperetin, we characterized the mechanism of diosmetin-induced inhibition only. This flavonoid proved to be a reversible, dead-end, full inhibitor of CYP2C8, its mean inhibition constant (Ki)being3.13« 0.11 µM. Kinetic analysis showed that diosmetin caused mixed-type inhibition, since it significantly decreased the Vmax (maximum velocity) and increased the Km value (substrate concentration yielding 50% of Vmax) of the reaction. The results of kinetic analyses were consistent with those of molecular docking simulation, which showed that the putative binding site of diosmetin coincided with the CYP2C8 substrate binding site. The demonstration that diosmetin inhibits CYP2C8 at concentrations similar to those observed after in vivo administration (in the low micromolar range) is of potential clinical relevance, since it may cause pharmacokinetic interactions with co- administered drugs metabolized by this CYP. -

Cholesterol Metabolites 25-Hydroxycholesterol and 25-Hydroxycholesterol 3-Sulfate Are Potent Paired Regulators: from Discovery to Clinical Usage
H OH metabolites OH Review Cholesterol Metabolites 25-Hydroxycholesterol and 25-Hydroxycholesterol 3-Sulfate Are Potent Paired Regulators: From Discovery to Clinical Usage Yaping Wang 1, Xiaobo Li 2 and Shunlin Ren 1,* 1 Department of Internal Medicine, McGuire Veterans Affairs Medical Center, Virginia Commonwealth University, Richmond, VA 23249, USA; [email protected] 2 Department of Physiology and Pathophysiology, School of Basic Medical Sciences, Fudan University, Shanghai 200032, China; [email protected] * Correspondence: [email protected]; Tel.: +1-(804)-675-5000 (ext. 4973) Abstract: Oxysterols have long been believed to be ligands of nuclear receptors such as liver × recep- tor (LXR), and they play an important role in lipid homeostasis and in the immune system, where they are involved in both transcriptional and posttranscriptional mechanisms. However, they are increas- ingly associated with a wide variety of other, sometimes surprising, cell functions. Oxysterols have also been implicated in several diseases such as metabolic syndrome. Oxysterols can be sulfated, and the sulfated oxysterols act in different directions: they decrease lipid biosynthesis, suppress inflammatory responses, and promote cell survival. Our recent reports have shown that oxysterol and oxysterol sulfates are paired epigenetic regulators, agonists, and antagonists of DNA methyl- transferases, indicating that their function of global regulation is through epigenetic modification. In this review, we explore our latest research of 25-hydroxycholesterol and 25-hydroxycholesterol 3-sulfate in a novel regulatory mechanism and evaluate the current evidence for these roles. Citation: Wang, Y.; Li, X.; Ren, S. Keywords: oxysterol sulfates; oxysterol sulfation; epigenetic regulators; 25-hydroxysterol; Cholesterol Metabolites 25-hydroxycholesterol 3-sulfate; 25-hydroxycholesterol 3,25-disulfate 25-Hydroxycholesterol and 25-Hydroxycholesterol 3-Sulfate Are Potent Paired Regulators: From Discovery to Clinical Usage. -

Synonymous Single Nucleotide Polymorphisms in Human Cytochrome
DMD Fast Forward. Published on February 9, 2009 as doi:10.1124/dmd.108.026047 DMD #26047 TITLE PAGE: A BIOINFORMATICS APPROACH FOR THE PHENOTYPE PREDICTION OF NON- SYNONYMOUS SINGLE NUCLEOTIDE POLYMORPHISMS IN HUMAN CYTOCHROME P450S LIN-LIN WANG, YONG LI, SHU-FENG ZHOU Department of Nutrition and Food Hygiene, School of Public Health, Peking University, Beijing 100191, P. R. China (LL Wang & Y Li) Discipline of Chinese Medicine, School of Health Sciences, RMIT University, Bundoora, Victoria 3083, Australia (LL Wang & SF Zhou). 1 Copyright 2009 by the American Society for Pharmacology and Experimental Therapeutics. DMD #26047 RUNNING TITLE PAGE: a) Running title: Prediction of phenotype of human CYPs. b) Author for correspondence: A/Prof. Shu-Feng Zhou, MD, PhD Discipline of Chinese Medicine, School of Health Sciences, RMIT University, WHO Collaborating Center for Traditional Medicine, Bundoora, Victoria 3083, Australia. Tel: + 61 3 9925 7794; fax: +61 3 9925 7178. Email: [email protected] c) Number of text pages: 21 Number of tables: 10 Number of figures: 2 Number of references: 40 Number of words in Abstract: 249 Number of words in Introduction: 749 Number of words in Discussion: 1459 d) Non-standard abbreviations: CYP, cytochrome P450; nsSNP, non-synonymous single nucleotide polymorphism. 2 DMD #26047 ABSTRACT Non-synonymous single nucleotide polymorphisms (nsSNPs) in coding regions that can lead to amino acid changes may cause alteration of protein function and account for susceptivity to disease. Identification of deleterious nsSNPs from tolerant nsSNPs is important for characterizing the genetic basis of human disease, assessing individual susceptibility to disease, understanding the pathogenesis of disease, identifying molecular targets for drug treatment and conducting individualized pharmacotherapy. -
Warfarin Sensitivity (CYP2C8, CYP2C9
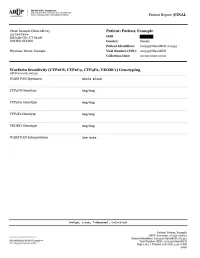
Patient Report |FINAL Section 79-1 of New York State Civil Rights Law requires informed consent be obtained from patients (or their legal guardians) prior to pursuing genetic testing. These forms must be kept on file by the ordering physician. Consent forms for genetic testing are available at www.aruplab.com. Incidental findings are not reported unless clinically significant but are available upon request. A Neg result indicates that no variants were detected. All variant alleles are defined based on consensus nomenclature and suggest reduced function of the associated protein(s). CYP2C8 and CYP2C9 are associated with inactivation of warfarin through metabolism. Variant alleles suggest reduced rates of warfarin metabolism, a prolonged time required to achieve steady-state concentrations, and a reduced dose requirement. CYP4F2 is associated with vitamin K recycling. Variant alleles suggest an increased dose requirement. VKORC1 is the therapeutic target for warfarin. Variant alleles suggest increased warfarin sensitivity and a reduced dose requirement. Dosing calculators such as that available through www.WarfarinDosing.org are available to predict loading and therapeutic/maintenance doses. This result has been reviewed and approved by , Ph.D. BACKGROUND INFORMATION: Warfarin Sensitivity (CYP2C8, CYP2C9 , CYP4F2, VKORC1) Genotyping CHARACTERISTICS: Warfarin sensitivity can lead to a life-threatening overdose event such as excessive bleeding. Genetic variation is recognized to explain a large proportion of variability in warfarin dose requirements. This test may predict individual warfarin sensitivity and non-standard dose requirements. The cytochrome P450 (CYP) isozymes 2C8 and 2C9 are involved in the metabolism of many drugs. Variants in the genes that code for CYP2C8 and CYP2C9 may influence pharmacokinetics of substrates such as warfarin, and may predict or explain non-standard dose requirements, therapeutic failure or adverse reactions. -

Caffeine Metabolism and Cytochrome P450 Enzyme Mrna Expression
Caffeine metabolism and Cytochrome P450 enzyme mRNA expression levels of genetically diverse inbred mouse strains Neal Addicott - CSU East Bay, Michael Malfatti - Lawrence Livermore National Laboratory, Gabriela G. Loots - Lawrence Livermore National Laboratory Metabolic pathways for caffeine 4. Results 1. Introduction (in mice - human overlaps underlined) Metabolites 30 minutes after dose Caffeine is broken down in humans by several enzymes from the Cytochrome Caffeine (1,3,7 - trimethylxanthine) O CH3 (n=6 per strain) CH3 6 N Paraxanthine/Caffeine N 7 Theophylline/Caffeine *Theobromine/Caffeine P450 (CYP) superclass of enzymes. These CYP enzymes are important in Theophylline 1 5 0.06 0.06 0.06 8 (7-N-demethylization) (1,3 - dimethylxanthine) 2 4 9 3 O N 0.05 0.05 0.05 activating or eliminating many medications. The evaluation of caffeine O H N 1,3,7 - trimethyluricacid CH 3 O CH3 N CH eine Peak Area Peak eine eine Peak Area eine Cyp1a2 3 CH 0.04 Area Peak eine 0.04 0.04 f f N f metabolites in a patient has been proposed as a means of estimating the activity 1 7 3 (3-N-demethylization) N Cyp3a4 N1 7 (8-hydrolyzation) 8 OH 0.03 0.03 0.03 of some CYP enzymes, contributing to genetics-based personalized medicine. O 3 N N Cyp1a2 3 O N Paraxanthine (1-N-demethylization) N 0.02 0.02 0.02 CH3 (1,7 - dimethylxanthine) CH3 O CH3 0.01 0.01 0.01 CH3 Theophylline Peak Area / Ca Peak Theophylline Paraxanthine Peak Area / Ca The frequency and distribution of polymorphisms in inbred strains of mice N Area / Ca Peak Theobromine 7 paraxanthine peak area /caffeine peak area /caffeine paraxanthine peak area theophylline peak area /caffeine peak area /caffeine theophylline peak area N1 Theobromine 0 0 peak area /caffeine peak area theobromine 0 0 C57BL/6JC57BL BALB/cJBALB CBA/JCBA/J DBA/2JDBA/2J .