JMSCR Vol.||03||Issue||08||Page 7010-7016||August 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gujarat Maritime Board
TERRESTRIAL ENVIRONMENTAL IMPACT ASSESSMENT REPORT FOR DEVELOPMENT OF COAST GUARD JETTY AND ALLIED FACILITIES WITHIN EXISTING OKHA PORT, OKHA TOWN, OKHAMANDAL TEHSIL, DEVBHUMI DWARKA DISTRICT, GUJARAT Project Proponent GUJARAT MARITIME BOARD (Government of Gujarat Undertaking) SAGAR BHAVAN, Sector 10-A, Opp. Air Force Centre, CHH Rd, Gandhinagar, Gujarat 382010 EIA Consultant Cholamandalam MS Risk Services Limited NABET Accredited EIA Consulting Organisation Certificate No: NABET/EIA/1011/011 PARRY House 3rd Floor, No. 2 N.S.C Bose Road, Chennai - 600 001 Tamil Nadu August 2018 PJ-ENVIR - 2017511-1253 Development of Coast Guard Jetty and allied facilities within existing Okha Port, Okha, District-Devbhumi Dwarka, Gujarat. DECLARATION BY PROJECT PROPONENT OKHA port has conducted the EIA Study on “Development of Coast Guard Jetty and Allied Facilities within Existing Okha Port, Okhamandal Tehsil, Devbhumi Dwarka District, Gujarat” The EIA report preparation has been undertaken in compliance with the ToR issued by MoEF & CC. Information and content provided in the report is factually correct for the purpose and objective for such study undertaken. We hereby declare the ownership of contents (information and data) of EIA/EMP Report. For on behalf of Gujarat Maritime Board Signature: Name: Mr. Atul A. Sharma Designation: Deputy General Manager - Environment Cholamandalam MS Risk Services Page 1 PJ-ENVIR - 2017511-1253 Development of Coast Guard Jetty and allied facilities within existing Okha Port, Okha, District-Devbhumi Dwarka, Gujarat. DECLARATION BY EIA CONSULTANT EIA Study on “Development of Coast Guard Jetty and Allied Facilities within Existing Okha Port, Okhamandal Tehsil, Devbhumi Dwarka District, Gujarat”. This EIA report has been prepared by Cholamandalam MS Risk Services Limited (CMSRSL), in line with EIA Notification, dated 14th September 2006, seeking prior Environmental Clearance from the Ministry of Environment, Forests and Climate Change, New Delhi. -

C1-27072018-Section
TATA CHEMICALS LIMITED LIST OF OUTSTANDING WARRANTS AS ON 27-08-2018. Sr. No. First Name Middle Name Last Name Address Pincode Folio / BENACC Amount 1 A RADHA LAXMI 106/1, THOMSAN RAOD, RAILWAY QTRS, MINTO ROAD, NEW DELHI DELHI 110002 00C11204470000012140 242.00 2 A T SRIDHAR 248 VIKAS KUNJ VIKASPURI NEW DELHI 110018 0000000000C1A0123021 2,200.00 3 A N PAREEKH 28 GREATER KAILASH ENCLAVE-I NEW DELHI 110048 0000000000C1A0123702 1,628.00 4 A K THAPAR C/O THAPAR ISPAT LTD B-47 PHASE VII FOCAL POINT LUDHIANA NR CONTAINER FRT STN 141010 0000000000C1A0035110 1,760.00 5 A S OSAHAN 545 BASANT AVENUE AMRITSAR 143001 0000000000C1A0035260 1,210.00 6 A K AGARWAL P T C P LTD AISHBAGH LUCKNOW 226004 0000000000C1A0035071 1,760.00 7 A R BHANDARI 49 VIDYUT ABHIYANTA COLONY MALVIYA NAGAR JAIPUR RAJASTHAN 302017 0000IN30001110438445 2,750.00 8 A Y SAWANT 20 SHIVNAGAR SOCIETY GHATLODIA AHMEDABAD 380061 0000000000C1A0054845 22.00 9 A ROSALIND MARITA 505, BHASKARA T.I.F.R.HSG.COMPLEX HOMI BHABHA ROAD BOMBAY 400005 0000000000C1A0035242 1,760.00 10 A G DESHPANDE 9/146, SHREE PARLESHWAR SOC., SHANHAJI RAJE MARG., VILE PARLE EAST, MUMBAI 400020 0000000000C1A0115029 550.00 11 A P PARAMESHWARAN 91/0086 21/276, TATA BLDG. SION EAST MUMBAI 400022 0000000000C1A0025898 15,136.00 12 A D KODLIKAR BLDG NO 58 R NO 1861 NEHRU NAGAR KURLA EAST MUMBAI 400024 0000000000C1A0112842 2,200.00 13 A RSEGU ALAUDEEN C 204 ASHISH TIRUPATI APTS B DESAI ROAD BOMBAY 400026 0000000000C1A0054466 3,520.00 14 A K DINESH 204 ST THOMAS SQUARE DIWANMAN NAVYUG NAGAR VASAI WEST MAHARASHTRA THANA -
DDMP-Devbhumi Dwarka
District Disaster Management Plan DEVBHUMI DWARKA COLLECTOR OFFICE DEVBHUMI DWARKA 2018 Website: http://devbhumidwarka.gujarat.gov.in 1 Dr. Narendra Kumar Meena, IAS District Collector Devbhumi Dwarka At.Khambhalia FOREWORD Dr. Narendra Kumar Meena, IAS District Collector Devbhumi Dwarka 2 INDEX Sr.No. Detail Page No. 1 Chapter-1 6-16 Introduction 06 What is Disaster 09 Objective of plan 09 Scope of the plan 10 Authority and Responsibility 10 Approach to Disaster Management 10 Warning, Relief and Recovery 10 Mitigation, Prevention and Preparedness 10 Finance 11 District Profile 12 Area and Administration 12 Climate and Coastal villages 13 River and Dam 13 Port and fisheries 14 Salt work 14 Live stock 14 Road and Railway 15 Health 15 Temperature and Rainfall 15 2 Chapter-2 HRVA 16-26 Hazards Risk & Vulnerabilty Analysis 17 Identify the Hazards of concern 18 Methodology of HRVA 20 Assign the Prpbability Rating 20 Assign the Impact Rating 21 Assign the Vunrebaility Ranking 21 Areas with highest Vulnerability 22 Outcome 22 3 Chapter-3 Institutional arrangement 27-41 DM structure in State 28 Incident Response System at State 28 Incident Response System at District 29 DEOC 30 DDMC 35 TDMC 35 CDMC 36 VDMC 38 Emmergency rescue kit 39 Forecasting warning system 40 4 Chapter-4 Preventtion and Mitigation measures 42-55 Prevention and mitigation plan 43 Mitigation measures for all Disaster 44 Structural and Non Structural Measures for all Disaster 54 List of On Going Programmes 50 Development Scheme 53 Risk Management Funding 54 5 Preparedness Measures 56-70 3 Identification of Stakeholder and Person of training 57 Training Need Analysis 61 Activation of IRS 62 Awareness Generation 64 NGO and Other stake holder coordination 64 DRM Programme 66 Community Warning System 69 Disaster Advisory Action Plsn 70 6 Chapter-6 Response Measures 71-89 Warning and Alert 72 District Crisis Management Meeting 73 Activation of EOC 73 Role and Responsibility of Each Department 73 Incident Command System 84 7. -

General Population Tables, Series-25
CENSUS OF INDIA 2001 SERIES 25 GUJARAT GENERAL POPULATION TABLES (Tables A-I to A-4) DIRECTORATE OF CENSUS OPERTIONS GUJARAT, AHMADABAD 315.475 2001 GPT Contents Page PREFACE V FIGURES AT A GLANCE IX MAP RELATING TO ADMINISTRATIVE DIVISIONS XI SECTION 1 - GENERAL NOTE GENERAL NOTE :.?-\'2 Basic Census Concepts and Definitions 1~ - 19 SECTION 2 . TABLES A -1: NUMBER OF VILLAGES, TOWNS, HOUSEHOLDS, POPULATION AND AREA Statements 2.b - ~S Map relating to Rural and Urban Population by Sex 2001 :"lei Map relating to Sex ratio - 2001 L1[ Diagram regarding Area, India and States 2001 yJ Diagram regarding Population, India and States - 2001 4 c) Diagram regarding Population, State and Districts- 2001 ~7 Map relating to Density of Population L,C) Table A-1 :~ I - 7 'i, c Appendix - 1 b'1-q 1 A -2: DECADAL VARIATION IN POPULATION SINCE 1901 lul- I~S Statements '('):-\ - \\3 - Diagram relating to Growth of Population 1901-2001 India and State GUJarat \, S Table A-2 1\ 1 - 12 'j' Appendix 127 --\2'6 A -3: VILLAGES BY POPULATION SIZE CLASS I"L-q- \Gq . ' Statements I '2 cl .- \ ?>,3 TABLE A-3 1".'3 - i G Li Appendix U>:; - \G ~ A - 4: TOWNS AND URBAN AGGLOMERATIONS CLASSIFIED BY (11- :~'tB POPULATION SIZE. CLASS IN 2001 WITH VARIATION SINCE 1901 Statements \"13 - LYO Diagram regarding Growth of Urban Population showing percentage (1901-2001) 2y/ Map showing Population of Towns in six size classes 2001 :2 Li 3 - 2. {~ '5 Map showing Urban Agglomerations (2.':17 Alphabetical list of towns, 2001 2.L\l1-- 2~y Alphabetical list of Urban Agglomerations -

District Disaster Management Plan DEVBHUMI DWARKA
District Disaster Management Plan DEVBHUMI DWARKA COLLECTOR OFFICE DEVBHUMI DWARKA 2017 Website: http://devbhumidwarka.gujarat.gov.in 1 FOREWORD Devbhumi Dwarka district is bifurecated from Jamnagar District in August, 2013. The District is multi hazard prone district, it is affeccted by various disasters like Drought, Scarcity, Flood, Cyclone, earthquake and Industrial accidents. The district had faced multitude of Disaster as Floods, Cyclone, Heavy Rain, Lightening, Earthquake and Fires. Experience has shown that pre- planned and practiced procedures for handling an emergency can considerably reduce loss of life and minimize damage too. The industries have onsite emergency plans but those were limited to the particular territory, but now under the Disaster Risk Management Program Gujarat State Disaster Management Authority, and District Disaster Management Committee- Devbhumi Dwarka are preparing the communities from grass root level to top level for securing quick response mechanism right from bottom to top level under the three DRM Components these are Awareness generation, Plan Preparation and Capacity Building. Disaster Management Plan of Devbhumi Dwarka District has been updated and additional details have been incorporated. The success of disaster management depends upon the co- coordinator and effective performance of the duties assigned to each and every department/agency. The Role of each department in the event of an emergency is specified in the District Disaster Management Plan. I take this opportunity to place on individuals, agencies, organizations who have contributed for the preparation and updation of the Multi Hazards / Disaster Management Plan of Devbhumi Dwarka. I hope that all the administrative units of the district, safety departments of all industries and Mutual Aid Scheme Members will use this action plan in the true spirit. -

World Bank Document
IN: NATIONLA CYCLONE RISK MITIGATION PROJECT II (P144726) I. General Public Disclosure Authorized 1. Bank’s approval Date of the procurement Plan: Original: May 21, 2015 2. Date of General Procurement Notice: May 5, 2015 3. Period covered by this procurement plan: The procurement period of project covered from Year May 5, 2015 to October 2016 II. Goods and Works and non-consulting services. 1. Prior Review Threshold: Procurement Decisions subject to Prior Review by the Bank as stated in Appendix 1 to the Guidelines for Procurement: Procurement Method Prior Review Threshold Comments Public Disclosure Authorized US$ 1. ICB (Goods) Above US$ 2 million All 2. NCB (Goods) Above US$ 2 million All 3. ICB (Works) Above US$ 10 million All 4. NCB (Works) Above US$ 10 million All 5. Services (non-consultant) Above US$ 2 million All 6. LIB Above US$ 30,000 Procurement Methods and Threshold Category Method of Procurement Threshold (US$ Equivalent) Public Disclosure Authorized Goods and Non-consultant ICB >3,000,000 services LIB Wherever agreed by the Bank NCB Up to 3,000,000 (with NCB conditions) Shopping Up to 100,000 DC As per Para 3.7 of the Bank Guidelines Force Account As per Para 3.9 of Guidelines Framework Agreements As per Para 3.6 of Guidelines Works ICB >40,000,000 NCB Up to 40,000,000 (with NCB conditions) Shopping Up to 200,000 Public Disclosure Authorized Force Account As per Para 3.9 of Guidelines DC As per Para 3.7 of Guidelines Community Participation As per Para 3.19 of Guidelines Page 1 of 4 Prior Review by the Bank. -
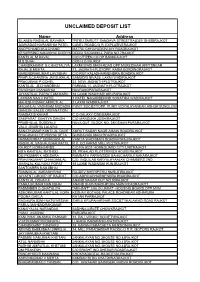
Unclaimed Deposit List
UNCLAIMED DEPOSIT LIST Name Address SILABEN RASIKLAL BAVARIA "PITRU SMRUTI" SANGAVA STREETRAJDEV SHERIRAJKOT JAMNADAS NARANBHAI PATEL CANEL ROADC/O R. EXPLASIVERAJKOT ANOPCHAND MULCHAND MATRU CHHAYADIGVIJAY ROADRAJKOT KESARISING NANJIBHAI DODIYA DODIA SADANMILL PARA NO.7RAJKOT KANTILAL M RAVAL C/O CITIZEN CO.OP.BANKRAJKOT M S SHAH CCB.H.O.RAJKOT CHANDRAKANT G CHHOTALIYA LAXMI WADI MAIN ROAD OPP MURLIDHAR APPTSNEAR RAJAL B MEHTA 13, JAGNATH PLOTOPP. KADIA BORDINGRAJKOT NARENDRAKUMAR LAVJIBHAI C/O RUP KALADHARMENDRA ROADRAJKOT PRAFULCHANDRA JAYSUKHLAL SAMUDRI NIVAS5, LAXMI WADIRAJKOT PRAGJIBHAI P GOHEL 22. NEW JAGNATH PLOTRAJKOT KANTILAL JECHANDBHAI PARIMAL11, JAGNATH PLOTRAJKOT RAYDHAN CHANABHAI NAVRANGPARARAJKOT JAYANTILAL PARSOTAM MARU 18 LAXMI WADIHARI KRUPARAJKOT LAXMAN NAGJI PATEL 1 PATEL NAGARBEHIND SORATHIA WADIRAJKOT MAHESHKUMAR AMRUTLAL 2 LAXMI WADIRAJKOT MAGANLAL VASHRAM MODASIA PUNIT SOCIETYOPP. PUNIT VIDYALAYANEAR ASHOK BUNGLOW GANESH SALES ORGANATION RAMDAS B KAHAR C.O GALAXY CINEMARAJKOT SAMPARAT SAHITYA SANGH C/O MANSUKH JOSHIRAJKOT PRABHULAL BUDDHAJI NAVA QUT. BLOCK NO. 28KISHAN PARARAJKOT VALJI JIVABHIA LALKIYA SANATKUMAR KANTILAL DAVE AMRUT SADAR NAGR AMAIN ROADRAJKOT BHAGWANJI DEVSIBHAI SETA GUNDAVADI MAIN ROADRAJKOT HASMUKHRAY CHHAGANLAL VANIYA WADI MAIN ROADNATRAJRAJKOT RASIKLAL VAGHAJIBHAI PATEL R.K. CO.KAPAD MILL PLOTRAJKOT RAJKOT HOMEGARDS C/O RAJKOT HOMEGUARD CITY UNITRAJKOT NITA KANTILAL RATHOD 29, PRHALAD PLOTTRIVEDI HOUSERAJKOT DILIPKUMAR K ADESARA RAMNATH PARAINSIDE BAHUCHARAJI NAKARAJKOT PRAVINKUMAR CHHAGANLAL -

Jamnagar District Geographical Area (1/2) (Gujarat State) Jamnagar Geographical Area (2/2)
69°0'0"E 69°10'0"E 69°20'0"E 69°30'0"E 69°40'0"E 69°50'0"E 70°0'0"E 70°10'0"E 70°20'0"E 70°30'0"E 70°40'0"E JAMNAGAR DISTRICT GEOGRAPHICAL AREA (1/2) (GUJARAT STATE) JAMNAGAR GEOGRAPHICAL AREA (2/2) 23°0'0"N KEY MAP 23°0'0"N ± CA-11 ARABIAN SEA CA-12 CA-07 CA-06 CA-10 CA-01 CA-05 CA-02 CA-08 CA-04 CA-03 CA-14 CA-09 CA-07 CA-06 RAJKOT CA-20 CA-15 CA-18 CA-10 JAMNAGAR CA-13 CA-19 CA-17 CA-01 CA-05 CA-16 #AMRAN CA-02 22°50'0"N 22°50'0"N PORBANDAR CA-08 JODIYA CA-04 BALAMBHA CA-03 # TotalGeographicalArea(Sq.KMs) No.ChargeAreas JODIYA CA-11 10630 20 FOR DETAILS OF CHARGE AREAS FROM /" S CA-01 TO CA-10,REFER TO H 2 Charge Areas Identification Important location within 5 JAMNAGAR MAP (2/2) CA-1 To CA-10 Jamnagar Urban CA-11 Jodiya CA-12 Dhrol CA-09 22°40'0"N CA-13 Kalavad 22°40'0"N CA-14 Jamnagar HADIYANA LATIPUR # # Tow CA-15 Lalpur ards CA-16 Jamjodhpur SH22 Tan G kara CA-17 Bhanvad U H6 L S CA-18 Khambhalia F /"DHROL CA-19 Kalyanpur O CA-20 Okhamandal F CA-12 K 22 INS VALSURA SH U KHIJADIA BIRD SANCTUARY DHROL T !. !. C DHUNVAV H # S H25 22°30'0"N 22°30'0"N OKHA JAMNAGAR To LEGEND !. -

Bla Coke Private Limited
+91-9624396922 Bla Coke Private Limited https://www.indiamart.com/bla-coke-limited/ Promoter family of our company was one of the biggest Coal miners in India before nationalisation of Coal mines. Our experience comes from being in the Coal and Coke business for last three generations. Over the years, we have mastered the art of ... About Us Promoter family of our company was one of the biggest Coal miners in India before nationalisation of Coal mines. Our experience comes from being in the Coal and Coke business for last three generations. Over the years, we have mastered the art of making Coke of the highest quality. In the year 1989, we obtained necessary license from Government of India to manufacture Coke at Village Arambhada, Mithapur, District Jamnagar in Gujarat. We were the first company to produce Coke in Gujarat. We were the first Indian Coke oven unit in the private sector to produce premium grade Low Ash Metallurgical Coke (LAMC). We were also the first Indian company to put up a port based merchant non – recovery Coke plant. Since then, the company has increased its production capacity from time to time. It is now a fully mechanised and automated State of the Art plant. We import our raw material - Coking Coal - from Australia and the finished product i.e. LAMC is supplied to various customers in Gujarat and other States of India. We have the facility of unloading and storage of adequate quantity of raw material. We also have Stockyard to store Coke of various sizes. We have constructed hardstand at screening plant to get clean Coke. -

TENDERING STATE HEALTH SOCIETY-GUJARAT Tender Have Been Invited from Chartered Accountants Firms Those Empanelled with ICAI
TENDERING STATE HEALTH SOCIETY-GUJARAT Tender have been invited from Chartered Accountants Firms those empanelled with ICAI for MEF for the F.Y.2020-21 for providing their services of concurrent audit of State Health Society-Gujarat granted by National Health Mission and Concurrent Audit of units Covered under State Health Society-Gujarat for the financial year 2021-22 through E-Tendering as per schedule time frame given below. Technical bid has to be submitted by both online and by physical Only by Speed Post / RPAD/Courier/by hand in Seal Pack Cover. Request for Proposal (RFP) can be download from www.nrhm.gujarat.gov.in, www.gujhealth.gujarat.gov.in and www.nprocure.com 1. Date of Tender & Time : 13/05/2021, 12:00PM 2. Pre bid meeting date & time : 20/05/2021, 12:00 PM 3. Last date and time for submit of bid(online) : 03/06/2021,06:00 PM 4. Last date and time for submit of bid(Physical) : 04/06/2021 Before 6:00 PM 5. Date and time for opening of technical bid : 07/06/2021, 12:00 PM 6. Date and time for opening of financial bid : 15/06/2021, 12:00 PM Venue : "Meeting Hall", Finance Management Group, C/o. Mission Director’s Office, State Program Management Unit, 1st Floor, NHM Bhavan, Civil Hospital campus, Sector-12 Gandhinagar-382012. Mission Director State Health Mission Gandhingar E-mail : [email protected], Tel 9879829962, 9726399693, 9687631926. For Technical Support please contact on : 7359021663 Address for Speed Post / RPAD / courier : Program Manager (Finance), Finance Management Group, C/o. -

The Gulf of Kutch Marine National Park and Sanctuary: a Case Study
Gulf of Kutch Marine National Park and Marine Wildlife Sanctuary: A case study Item Type monograph Authors Biswas, Nilanjana Publisher International Collective in Support of Fishworkers Download date 30/09/2021 23:12:44 Link to Item http://hdl.handle.net/1834/19897 The Gulf of Kutch Marine National Park and Sanctuary: A Case Study By Nilanjana Biswas International Collective in Support of Fishworkers Chennai International Collective in Support of Fishworkers (ICSF) List of Acronyms and Abbreviations BOD biological oxygen demand bn billion CF Conservator of Forests CRZ Coastal Regulation Zone CZM Coastal Zone Management DCC Digvijay Cement Company EEZ exclusive economic zone EMCB Environment Management Capacity Building GEER Gujarat Environment and Education Research Foundation GMB Gujarat Maritime Board GSFC Gujarat State Fertilizer Company ha hectare HMKP Hind Mazdoor Kisan Panchayat ICMAM integrated coastal and marine area management plan ICZM integrated coastal zone management IOC Indian Oil Company ISI Indian Standards Institution MARPOL International Convention for the Prevention of Pollution from Ships MASS Machchimaar Adhikar Sangharsh Samiti MCPA marine and coastal protected areas MLD million litres per day mn million MNPS Marine National Park and Sanctuary MoEF Ministry of Environment and Forests MoU memorandum of understanding MPA marine protected area NBWL National Board for Wild Life NFF National Fishworkers' Forum NGO non-governmental organization NIO National Institute of Oceanography NRC National Research Council PA protected area RPL Reliance Petroleum Limited RTI Right to Information (Act) International Collective in Support of Fishworkers (ICSF) SBM single buoy mooring SEAP State Environmental Action Programme SEZ special economic zone sq km square kilometre TCL Tata Chemicals Limited tpa tonnes per annum WII Wildlife Institute of India WLPA Wild Life (Protection) Act, 1972 International Collective in Support of Fishworkers (ICSF) Contents Summary 1 1. -

TCSRD Annual Report 2008-09
Annual Report 2008-09 CONTENTS Introduction 1 Vision, Mission & Values 2 President’s Message 3 Guiding Principles 4 Mithapur Region 5 Natural Resource Management 6 Income Generation 8 Health Education & Infrastructure 9 Environment 10 Babrala Region 11 Natural Resource Management 12 Income Generation 13 Health Education & Infrastructure 14 Environment 15 Haldia Region 16 Natural Resource Management & Income Generation 17 Health & Education 18 Volunteer programs 19 Volunteer Speak 20 Best Volunteer 21 Introduction Every Company has a special continuing responsibility towards the people of the area in which it is located. The company should spare its doctors, managers to advice the people of the village and supervise near development undertaken by co-operative effort between them and the company. - JRD Tata The above quote not only illustrates the ethos, but also summarizes the guidelines laid down by founder, Jamsetji Nusserwanji Tata. The facet of the Founder’s remarkable breadth of conception was his recognition that, corporate social responsibility was fundamental to India’s drive for industrialization, one of his defining tenets being, ‘the wealth which comes from the people must as far as possible go back to the people’. Tata Chemicals Limited (TCL) for last 70 years has been associated with a scalable, sustainable and integrated development of communities in and around the environment where we operate. This is not just a social responsibility but also a cornerstone for the existence of our business and hence has been incorporated in our corporate philosophy. TCL is one of the pioneering corporate sectors, to evolve the concept of social responsibility, established Tata Chemical Society for Rural Development (TCSRD) in 1970 to share its resources with the communities and geographies within which the company operates its business.