Nanoscalar Modifications to Polymeric Tissue Engineering Scaffolds: Effect on Cellular Behavior
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary Glossary
Glossary Glossary Albedo A measure of an object’s reflectivity. A pure white reflecting surface has an albedo of 1.0 (100%). A pitch-black, nonreflecting surface has an albedo of 0.0. The Moon is a fairly dark object with a combined albedo of 0.07 (reflecting 7% of the sunlight that falls upon it). The albedo range of the lunar maria is between 0.05 and 0.08. The brighter highlands have an albedo range from 0.09 to 0.15. Anorthosite Rocks rich in the mineral feldspar, making up much of the Moon’s bright highland regions. Aperture The diameter of a telescope’s objective lens or primary mirror. Apogee The point in the Moon’s orbit where it is furthest from the Earth. At apogee, the Moon can reach a maximum distance of 406,700 km from the Earth. Apollo The manned lunar program of the United States. Between July 1969 and December 1972, six Apollo missions landed on the Moon, allowing a total of 12 astronauts to explore its surface. Asteroid A minor planet. A large solid body of rock in orbit around the Sun. Banded crater A crater that displays dusky linear tracts on its inner walls and/or floor. 250 Basalt A dark, fine-grained volcanic rock, low in silicon, with a low viscosity. Basaltic material fills many of the Moon’s major basins, especially on the near side. Glossary Basin A very large circular impact structure (usually comprising multiple concentric rings) that usually displays some degree of flooding with lava. The largest and most conspicuous lava- flooded basins on the Moon are found on the near side, and most are filled to their outer edges with mare basalts. -

Feature of the Month – January 2016 Galilaei
A PUBLICATION OF THE LUNAR SECTION OF THE A.L.P.O. EDITED BY: Wayne Bailey [email protected] 17 Autumn Lane, Sewell, NJ 08080 RECENT BACK ISSUES: http://moon.scopesandscapes.com/tlo_back.html FEATURE OF THE MONTH – JANUARY 2016 GALILAEI Sketch and text by Robert H. Hays, Jr. - Worth, Illinois, USA October 26, 2015 03:32-03:58 UT, 15 cm refl, 170x, seeing 8-9/10 I sketched this crater and vicinity on the evening of Oct. 25/26, 2015 after the moon hid ZC 109. This was about 32 hours before full. Galilaei is a modest but very crisp crater in far western Oceanus Procellarum. It appears very symmetrical, but there is a faint strip of shadow protruding from its southern end. Galilaei A is the very similar but smaller crater north of Galilaei. The bright spot to the south is labeled Galilaei D on the Lunar Quadrant map. A tiny bit of shadow was glimpsed in this spot indicating a craterlet. Two more moderately bright spots are east of Galilaei. The western one of this pair showed a bit of shadow, much like Galilaei D, but the other one did not. Galilaei B is the shadow-filled crater to the west. This shadowing gave this crater a ring shape. This ring was thicker on its west side. Galilaei H is the small pit just west of B. A wide, low ridge extends to the southwest from Galilaei B, and a crisper peak is south of H. Galilaei B must be more recent than its attendant ridge since the crater's exterior shadow falls upon the ridge. -
Feature of the Month - August 2006
RECENT BACK ISSUES: http://www.zone-vx.com/tlo_back.html A PUBLICATION OF THE LUNAR SECTION OF THE A.L.P.O. EDITED BY: William M. Dembowski, F.R.A.S. - [email protected] Elton Moonshine Observatory - http://www.zone-vx.com 219 Old Bedford Pike (Elton) - Windber, PA 15963 FEATURE OF THE MONTH - AUGUST 2006 RHEITA E Sketch and text by Robert H. Hays, Jr. - Worth, Illinois, USA March 5, 200 - 01:15 to 01:45 UT 15cm Newtonian - 170x - Seeing 7-8/10 I sketched this crater and vicinity on the evening of March 4, 2006 after observing two occultations. This feature is located amid a jumble of craters south of Mare Fecunditatis. This is an elongated crater that appears to be the result of at least three impacts. The north and south lobes are about the same size, but the southern lobe is definitely deeper. The central portion is about the size of the north and south lobes combined. There are some bits of shadow on the floor, but I saw no obvious hills or craters there. I have drawn the shadowing within and around Rheita E as I saw it. There is an obvious ridge extending westward from the south lobe. The crater Rheita F is adjacent to the south lobe of Rheita E, and has a strip of shadow parallel to the ridge from Rheita E. Rheita M is the large, shallow crater east of Rheita E's south end, and Rheita N is the small, shallow pit between them. Stevinus D is the slightly smaller, but deeper crater north of Rheita M. -

July 2020 in This Issue Online Readers, ALPO Conference November 6-7, 2020 2 Lunar Calendar July 2020 3 Click on Images an Invitation to Join ALPO 3 for Hyperlinks
A publication of the Lunar Section of ALPO Edited by David Teske: [email protected] 2162 Enon Road, Louisville, Mississippi, USA Recent back issues: http://moon.scopesandscapes.com/tlo_back.html July 2020 In This Issue Online readers, ALPO Conference November 6-7, 2020 2 Lunar Calendar July 2020 3 click on images An Invitation to Join ALPO 3 for hyperlinks. Observations Received 4 By the Numbers 7 Submission Through the ALPO Image Achieve 4 When Submitting Observations to the ALPO Lunar Section 9 Call For Observations Focus-On 9 Focus-On Announcement 10 2020 ALPO The Walter H. Haas Observer’s Award 11 Sirsalis T, R. Hays, Jr. 12 Long Crack, R. Hill 13 Musings on Theophilus, H. Eskildsen 14 Almost Full, R. Hill 16 Northern Moon, H. Eskildsen 17 Northwest Moon and Horrebow, H. Eskildsen 18 A Bit of Thebit, R. Hill 19 Euclides D in the Landscape of the Mare Cognitum (and Two Kipukas?), A. Anunziato 20 On the South Shore, R. Hill 22 Focus On: The Lunar 100, Features 11-20, J. Hubbell 23 Recent Topographic Studies 43 Lunar Geologic Change Detection Program T. Cook 120 Key to Images in this Issue 134 These are the modern Golden Days of lunar studies in a way, with so many new resources available to lu- nar observers. Recently, we have mentioned Robert Garfinkle’s opus Luna Cognita and the new lunar map by the USGS. This month brings us the updated, 7th edition of the Virtual Moon Atlas. These are all wonderful resources for your lunar studies. -

Lick Observatory Records: Photographs UA.036.Ser.07
http://oac.cdlib.org/findaid/ark:/13030/c81z4932 Online items available Lick Observatory Records: Photographs UA.036.Ser.07 Kate Dundon, Alix Norton, Maureen Carey, Christine Turk, Alex Moore University of California, Santa Cruz 2016 1156 High Street Santa Cruz 95064 [email protected] URL: http://guides.library.ucsc.edu/speccoll Lick Observatory Records: UA.036.Ser.07 1 Photographs UA.036.Ser.07 Contributing Institution: University of California, Santa Cruz Title: Lick Observatory Records: Photographs Creator: Lick Observatory Identifier/Call Number: UA.036.Ser.07 Physical Description: 101.62 Linear Feet127 boxes Date (inclusive): circa 1870-2002 Language of Material: English . https://n2t.net/ark:/38305/f19c6wg4 Conditions Governing Access Collection is open for research. Conditions Governing Use Property rights for this collection reside with the University of California. Literary rights, including copyright, are retained by the creators and their heirs. The publication or use of any work protected by copyright beyond that allowed by fair use for research or educational purposes requires written permission from the copyright owner. Responsibility for obtaining permissions, and for any use rests exclusively with the user. Preferred Citation Lick Observatory Records: Photographs. UA36 Ser.7. Special Collections and Archives, University Library, University of California, Santa Cruz. Alternative Format Available Images from this collection are available through UCSC Library Digital Collections. Historical note These photographs were produced or collected by Lick observatory staff and faculty, as well as UCSC Library personnel. Many of the early photographs of the major instruments and Observatory buildings were taken by Henry E. Matthews, who served as secretary to the Lick Trust during the planning and construction of the Observatory. -
Journal of the Association of Lunar & Planetary Observers
ISSN-0039-2502 Journal of the Association of Lunar & Planetary Observers The Strolling Astronomer Volume 44, Number 1, Winter 2002 Now in Portable Document Format (PDF) for MacIntosh and PC-Compatible Computers Inside . Doings on Jupiter . In these remarkable CCD images taken by Antonio Cidadao (of Portugal), the amazing activity occurring in Jupiter's north equatorial belt (NEB) during 2002 January is easily apparent. At present, several bright rifts and a number of dark condensations can be seen, even visually, in the NEB at several locations around the planet. In the 2002 January 17 image (at left), note the two dark condensa- tions, or "barges," with a white oval between them, near the pre- ceding limb (right side of the image) of the planet. Also, note the bright rift in the NEB near the central meridian (CM). These barges are somewhat unusual in that they are usually seen on the northern edge of the NEB. In the 2002 January 18 image (right), the two barges and the bright oval are in generally the same position relative to each other; however, the bright rift has overtaken them and expanded. In fact, the two barges have drifted 4 and 5 degrees in increasing longitude and, the white oval has drifted 3 degrees in increas- ing longitude. By contrast, the bright rift has expanded from a length of 22 degrees to 35 degrees, with its preceding edge drifting 20 degrees in decreasing longitude. Also note the small, bright ovals on the northern edge of the NEB, reminiscent of the south south temperate belt (SSTB) ovals. -

Robert T Downs
Curriculum Vitae – Robert T. Downs 1 Field of Specialization: The crystallography and spectroscopy of minerals, with emphasis on crystal chemistry, bonding, temperature and pressure effects, characterization and identification. Contact Information: Dr Robert T Downs Department of Geosciences Voice: 520-626-8092 Gould-Simpson Building Lab: 520-626-3845 University of Arizona Fax: 520-621-2672 Tucson Arizona 85721-0077 [email protected] Education: University of British Columbia 1986 B.S. Mathematics Virginia Tech 1989 M.S. Geological Sciences Virginia Tech 1992 Ph.D. Geological Sciences Graduate Advisors: G.V. Gibbs (Mineralogy) and M.B. Boisen, Jr. (Mathematics) Carnegie Institution of Washington, Geophysical Laboratory, 1993 – 1996 Post-doc Advisors: R.M. Hazen and L.W. Finger Academic and Professional Appointments: Assistant Professor, Department of Geosciences, University of Arizona, August 1996 – 2002 Associate Professor, Department of Geosciences, University of Arizona, 2002 – 2008 Professor, Department of Geosciences, University of Arizona, 2008 – present Assistant to curator Joe Nagel: University of British Columbia, 1985 Assistant to curator Gary Ansell: National Mineral Collections of Canada, 1986 Assistant to curator Susan Eriksson: Virginia Tech Museum of Geological Sciences, 1990 Graduate teaching assistant: Virginia Tech, 1988 – 1992 Pre-doctoral Fellowship: Carnegie Institution of Washington, Geophysical Laboratory, 1991 Post-doctoral Fellowship: CIW, Geophysical Laboratory, February 1993 – July 1996 Visiting Professor, -

Inside: Housing 1978 Page 3 Innervisions Page 9
Inside: Housing 1978 Page 3 Innervisions Page 9 Friday, February 3, 1978 Bryant Coliege, Smithfield, Rhode Island Volume 43 Number 2 UPIUPDATE Trustees Increase Resident Rates Compiled by Jay Metzger By Ron Bunce The Board of Trustees has Part of the 12% increase will Under the new rates, and given the addition of furniture in each approved increases in dormi be absorbed by rising the same dormitory enrollments of the tripled suites. Each person tory, townhouse and meal plan maintenance expenses. Costs as this year, the added '78-'79 will have a bed (no cots). a INDIAN LAND? costs to students for the '78-'79 (for materials only) to repair or revenues for room and board bureau, and a desk. school year. In addition, a new replace glass, screens, ceiling will be $245,500. The rate increases intended to fe e for triple rooms in tiles, doors, carpets, and The rate increases will not absorb inflationary pressures are (UPI-WASH.)- Senator dormitories was established. The furniture in the Dorm Village result in new services or facilities in the following table. William Hathaway uys increases were attributed to the· reached $4(·000 in the '76-'77 in the dorms. The change will be President Carter may make a energy situation and an "overall fiscal year. recommendation to resolve the e scalation of operating The meal plan increase is in Double Room, Dormitory Increase of $100 per occupant Maine Indians Land Claims expenses." . anticipation of price increases in Triple Room, Dormitory New Fee - $600 per occupant Case next week, just prior to his The most recent dormitory the contract renewal with SAGA Townhouse, All Rooms I ncrease of $150 per occupant scheduled February 17th-18th rate increases were two years in September. -
January 2021 Click on Images in This Issue for Hyperlinks
A publication of the Lunar Section of ALPO Edited by David Teske: [email protected] 2162 Enon Road, Louisville, Mississippi, USA Back issues: http://www.alpo-astronomy.org/ Online readers, January 2021 click on images In This Issue for hyperlinks Announcements 2 Lunar Calendar October 2020 3 An Invitation to Join ALPO 3 Observations Received 4 By the Numbers 6 Submission Through the ALPO Image Achieve 7 When Submitting Observations to the ALPO Lunar Section 8 page 83 Call For Observations Focus-On 8 Focus-On Announcement 9 Schickard Sunrise Patch, S. Berté 10 Another Dome Home, R. Hill 11 Some Wonders on the Shores of Mare Crisium, A. Anunziato 12 Lunar Topographic Studies Program: Banded Craters 14 A Fleet Vision of Posidonius Y on Dorsa Smirnov, A. Anunziato 20 Aristarchus Plateau Region, H. Eskildsen 21 Focus On: The Lunar 100, Features 41-50, J. Hubbell 22 Lunar 41-50, a Personal View, A. Anunziato 25 Wargentin, R. Hays, Jr. 37 Recent Topographic Studies 79 Lunar Geologic Change Detection Program, T. Cook 119 page 84 Key to Images in this Issue 131 A very Happy New Year to all. We look forward to a good year ahead. Thank you contributors for your many contributions to this issue of The Lunar Observer. Your excellent submissions is what makes this newsletter possible. If you are reading this issue, welcome aboard! Perhaps you would like to contribute your own lunar observations to us. You can contribute observations if you are not a member of ALPO, but we sure would like you to consider becoming a member (yearly rates start at only $18.00, a great deal!). -

Lunar Domes Classification and Physical Properties by Raffaello Lena ………………………………………………..62
Selenology Today is devoted to the publication of contributions in the field of lunar studies. Editor-in-Chief: Manuscripts reporting the results of new research concerning the R. Lena astronomy, geology, physics, chemistry and other scientific Editors: aspects of Earth’s Moon are welcome. M.T. Bregante Selenology Today publishes C. Kapral papers devoted exclusively to the Moon. F. Lottero Reviews, historical papers J. Phillips and manuscripts describing observing or spacecraft P. Salimbeni instrumentation are considered. C. Wöhler C. Wood The Selenology Today Editorial Office [email protected] Selenology Today # 5 April 2007 SELENOLOGY TODAY #5 April 2007 Cover : Image taken by Gerardo Sbarufatti, Schmidt Cassegrain 200 mm f/10. Selenology Today websites http://digilander.libero.it/glrgroup/ http://www.selenologytoday.com/ Messier, Messier A and surrounding Mare Fecunditatis by Alexander Vandenbohede …………………………………..1 Crater depths from the Apollo era to the present by Kurt Allen Fisher …………………………………………….17 Lunar domes classification and physical properties by Raffaello Lena ………………………………………………..62 Selenology Today # 5 April 2007 TOPOGRAPHY SELENOLOGY TODAY # 5 Messier, Messier A and clusters, nebulae, galaxies etc. Charles surrounding Mare Fecunditatis Messier (1730 – 1817). Messier A has a by Alexander Vandenbohede diameter of 11 x 13 km and a depth of Association for Lunar and Planetary 2250 m. Both craters fall in the category Observers – Lunar Section of small craters (less than 15 – 20 km). However, their shape is atypical for these small and in most cases simple Abstract bowl shaped craters. Also atypical is the shape of the ejecta deposits, which is Messier and Messier A (formerly called highly asymmetrical. Messier features a Pickering) form an interesting crater pair butterfly-type of ray system with situated on the western part of Mare Fe- deposits towards the north and south of cunditatis. -
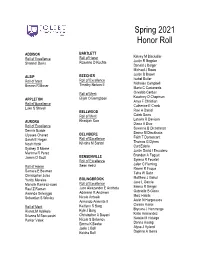
Spring 2021 Honor Roll
Spring 2021 Honor Roll ADDISON BARTLETT Kelsey M Blackaller Roll of Excellence Roll of Honor Justin R Bogdan Shannel Davis Roxanne D Kuchta Donald J Bolger Michael J Bowe Justin B Brown ALSIP BEECHER Isabel Butler Roll of Merit Roll of Excellence Nicholas Campbell Breann R Moser Timothy Nelson II Maria C Castaneda Osvaldo Cerdas Roll of Merit Kourtney D Chapman APPLETON Elijah O Bamgbose Anya F Christian Roll of Excellence Catherine E Cronk Luke S Stovall Ravi A Daniel BELLWOOD Caleb Davis Roll of Merit Latavia R Davison AURORA Khadijah Sain Diana A Diaz Roll of Excellence Savanna B Dicostanzo Dennis Budde Emma M Dieckhaus Ulysses Chavez BELVIDERE Faith T Domercant Sarah E Hogan Roll of Excellence Thomas G Dynes Noah Hook Kristina M Sartori Curt Ederle Sydney D Moore Justin David I Escudero Marinna R Perez Brandon A Fagust James D Scott BENSENVILLE Syrena R Feustel Roll of Excellence Jalen C Fleming Roll of Honor Sean Heinz Raven R Fuqua Samara E Bosman Taha W Gabr Christopher Jules Matthew J Gahol Yuritzi Morales BOLINGBROOK Jose L Garcia Menelik Ramirez-rowe Roll of Excellence Emma R Geiger Raul Z Roman Jace Alexzander E Ancheta Gabrielle B Glees Amanda Selvaggio Adrienne R Andrews Moiz Habibi Sebastian S Wesley Nicole Antosik Aislin N Hargreaves Armando Armenta II Carson Harris Roll of Merit Kaitlynn R Barg Brycara J Hemmings Rianat M Adekola Kyle J Barg Katie Hernandez Brianna M Boccassini Christopher A Bayani Natalie M Hidalgo Parker Valek Nicole S Bebenov Donna Huang Emma K Beebe Alysa J Hyland Josie L Bell Keisha Bell Daphne A -

Clark, Mardi Alphonsus Topographical
2006 TITLE PRINCIPAL AUTHOR FEATURE CATEGORY June Alphonsus: Nectarian or Pre-Nectarian? Clark, Mardi Alphonsus Topographical Studies Aug Brief History of the Alpine Valley Longshaw, Nigel Alpine Valley Topographical Studies Jan Arago & Environs Ebdon, Colin Arago Topographical Studies Jan Rima Archytas Eskildsen, Howard Archytas, Rima Topographical Studies Oct Lunar Drawing with a PDA Grego, Peter Atlas Sept Focus On: Atlas & Hercules Dembowski, William Atlas & Hercules Topographical Studies May Copernican Volcanoes Clark, Mardi Copernicus Domes July Bright Craterlet - Northern Mare Crisium Eskildsen, Howard Crisium, Mare Topographical Studies Dec Feature of the Month - Deslisle & Diophantus Hays, Robert H. Deslisle & Diophantus Topographical Studies Mar Focus On: Eratosthenes Dembowski, William Eratosthenes Topographical Studies Nov Feature of the Month - Hortensius Hays, Robert H. Hortensius Topographical Studies Mar Lava Flows in Mare Imbrium Braga, Raffaello Imbrium, Mare Topographical Studies Jan Feature of the Month - Kunowsky Hays, Robert H. Kunowsky Topographical Studies Feb Region East of Langrenus Ebdon, Colin Langrenus Topographical Studies May Feature of the Month - Madler Hays, Robert H. Madler Topographical Studies Oct Feature of the Month - Messier & Messier A Hays, Robert H. Messier & Messier A Topographical Studies Aug Tale of Brothers and Craters: Pickering and Messier A Clark, Mardi Messier A Topographical Studies Jan Focus On: Mare Nectaris Dembowski, William Nectaris, Mare Topographical Studies Jan Color Study of Mare Nectaris Vandenbohede, Alexander Nectaris, Mare Colorimetric July Feature of the Month - Parrot C Hays, Robert H. Parrot C Topographical Studies May Focus On: Pitatus Dembowski, William Pitatus Topographical Studies Sept Feature of the Month - Pontecoulant Hays, Robert H. Pontecoulant Topographical Studies Aug Feature of the Month - Rheita E Hays, Robert H.