Ferric Citrate)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Powerful Framework for the Chemical Design of Molecular Nanomagnets Yan Duan†,1,2, Joana T
Data mining, dashboards and statistics: a powerful framework for the chemical design of molecular nanomagnets Yan Duan†,1,2, Joana T. Coutinho†,*,1,3, Lorena E. Rosaleny†,*,1, Salvador Cardona-Serra1, José J. Baldoví1, Alejandro Gaita-Ariño*,1 1 Instituto de Ciencia Molecular (ICMol), Universitat de València, C/ Catedrático José Beltrán 2, 46980 Paterna, Spain 2 Department of Chemistry and the Ilse Katz Institute for Nanoscale Science & Technology, Ben-Gurion University of the Negev, Beer Sheva 84105, Israel 3 Centre for Rapid and Sustainable Product Development, Polytechnic of Leiria, 2430-028 Marinha Grande, Portugal *e-mail: [email protected], [email protected], [email protected] Abstract Three decades of intensive research in molecular nanomagnets have brought the magnetic memory in molecules from liquid helium to liquid nitrogen temperature. The enhancement of this operational temperature relies on a wise choice of the magnetic ion and the coordination environment. However, serendipity, oversimplified theories and chemical intuition have played the main role. In order to establish a powerful framework for statistically driven chemical design, we collected chemical and physical data for lanthanide-based nanomagnets to create a catalogue of over 1400 published experiments, developed an interactive dashboard (SIMDAVIS) to visualise the dataset, and applied inferential statistical analysis to it. We found that the effective energy barrier derived from the Arrhenius equation displays an excellent correlation with the magnetic memory, and that among all chemical families studied, only terbium bis-phthalocyaninato sandwiches and dysprosium metallocenes consistently present magnetic memory up to high temperature, but that there are some promising strategies for improvement. -

Coordination Chemistry (See Chapter 20, H&S 3Rd Ed.)
Coordination Chemistry (see Chapter 20, H&S 3rd Ed.) Transition metal elements, particularly ions, have a strong tendency to form compounds with Lewis bases. Why? Lewis base: electron pair donor egs. H2O, NH3 n+ Lewis acid: electron pair acceptor egs. M , BH3 ‘low lying’ empty orbitals: lower in energy than HOMO of Lewis case Lewis acidity enhanced by positive charge so TM ions are good Lewis bases 2+ 3+ familiar examples: AlCl3, BF3 from main group and M , M in TM series Type of bonding in these compounds? ‘coordinative’ or ‘dative’ bonds to form Lewis base ‘adducts’ L→M TM-Lewis base ‘adducts’ are often referred to as (i) TM ‘complexes’ OR (ii) coordination complexes NB: still polar covalent bonds – this just defines where the pair of electrons came from Some more definitions: ligand: molecule or ion that can act as a Lewis base to a metal - egs. Cl , PR3, ROR (R = generic term for an alkyl) donor atoms: atoms that are in direct contact with the metal ion O in R2O→M denticity: number of donor atoms per ligand; range from 1 to >6 unidentate bidentate tridentate O H O H2N NH2 2 O O water en diglyme N O O O N N O O N porphin 15-C-5 tetradentate pentadentate chelate: multidentate ligands forms rings; M tend to be very stable, OO especially 5 and 6 member chelate rings acac ‘bite’ or ‘bite angle’: a measure of the span or size of a chelate ligand; depends on M-L distance M OO acac coordination complex MLn generic terms commonly used: L neutral Lewis base (electron pair donor) X anionic donor (eg. -

Naming Coordination Compounds
Naming Coordination Compounds Author: Kit Mao Department of Chemistry, Washington University St. Louis, MO 63130 For information or comments on this tutorial, please contact K. Mao at [email protected]. Please click here for a pdf version of this tutorial. A coordination complex is a substance in which a metal atom or ion accepts electrons from (and thus associates with) a group of neutral molecules or anions called ligands. A complex can be an anion, a cation ion, or a neutral molecule. Coordination compounds are neutral substances (i.e. uncharged) in which at least one ion is present as a complex. You will learn more about coordination compounds in the lab lectures for experiment 5 in this course. The coordination compounds are named in the following way. (At the end of this tutorial, there are additional examples that demonstrate how coordination compounds are named.) A. When naming coordination compounds, always name the cation before the anion. This rule holds regardless of whether the complex ion is the cation or the anion. (This is just like naming an ionic compound.) B. In naming the complex ion: 1. Name the ligands first, in alphabetical order, and then name the metal atom or ion. Note: The metal atom or ion is written before the ligands in the chemical formula. 2. The names of some common ligands are listed in Table 1. · Anionic ligands end in “-o.” For anions that end in “-ide”(e.g. chloride, hydroxide), “-ate” (e.g. sulfate, nitrate), and “-ite” (e.g. nirite), change the endings as follows: -ide ® -o; e.g., chloride ® chloro and hydroxide ® hydroxo -ate ® -ato; e.g., sulfate ® sulfato and nitrate ® nitrato -ite ® -ito; e.g., nitrite ® nitrito · For neutral ligands, the common name of the molecule is used (e.g. -

Bridging Ligands
Chapter 9 Coordination Chemistry I: Structure and Isomers 9-1 History 9-2 Nomenclature 9-3 Isomerism 9-4 Coordination Numbers and Structure History What is coordination compound? Coordniantion compounds include compound composed of a metal atom or ion and one or more ligands that formally donate electrons to the metal. More specifically, a transition metal surrounded by neutral molecules or anions with a definite geometry. What is ligand? Ligand can be a atom, ion, and molecules. History Prussian blue (German: Preußischblau or Berliner Blau, in English Berlin blue) is a dark blueWhatpigment is coordinationused in paints and compound? formerly in blueprints. Prussian blue wasCoordination discovered complexesby accident were by pai knownnter Heinrich - although Diesbach not understood in Berlin in 1704-5,in which any sense is why - it since is also the known beginning as Berlin of chemistry, blue. (Diesbach e.g. Prussian was attempting to createblue a paint, Aureolin with ,aand red copperhue.) It vitriolhas several. different chemical names, these being iron(III) ferrocyanide, ferric ferrocyanide, iron(III) hexacyanoferrate(II), and ferricThe hexacyanoferrate. key breakthrough Commonly occurred when and c Alfredonveniently Werner it isproposed, simply called "PB. inter alia, that Co(III) bears six ligands in an octahedral geometry. Aureolin (sometimes called Cobalt Yellow) is a pigment used in oil and watercolor painting. Its color index name is PY40 (40th entry on list of yellow pigments). It was first made in 1851 and its chemical composition is potassium cobaltinitrite. Copper(II) sulfate ("sulphate" in most Commonwealth nations) is the chemical compound with the formula CuSO4. This salt exists as a series of compounds that differ in their degree of hydration. -

Complexation
FACULTY OF PHARMACEUTICAL SCIENCES, RAMAUNIVERSITY, KANPUR B.PHARM 3rd SEM PHYSICAL PHARMACEUTICS-I BP302T MR. PEEYUSH Assistant professor Rama university, kanpur Complexation Overview Classification Introduction Metal ion complexes Organic Complexes Inclusion Complexes Methods of Analysis Method of Continuous Variation PH Titration Distribution Method Solubility Method Spectroscopy Learning Objectives 1. Define the three classes of complexes with pharmaceutically relevant examples. 2. Describe chelates, their physically properties, and what differentiates them from organic molecular complexes. 3. Describe the types of forces that hold together organic molecular complexes with examples. 4. Describe the forces in polymer–drug complexes used for drug delivery. 5. Discuss the pharmaceutical applications of cyclodextrins. 6. Describe the methods of analysis of complexes and determine their stoichiometric ratios and stability constants. Classification Introduction Metal ion complexes Organic Complexes Inclusion Complexes INTRODUCTION Complexes are compounds that result from donor–acceptor mechanisms between two or more chemical species. Complexes can be divided broadly into three classes depending the type of the acceptor substance: 1. Metal ion complexes 2. Organic molecular complexes 3. Inclusion complexes Intermolecular forces involved in the formation of complexes: 1. Van der Waals forces. 2. Hydrogen bonds (important in molecular complexes). 3. Coordinate covalence (important in metal complexes). 4. Charge transfer. 5. Hydrophobic interaction. Introduction Types of Complexes Metal Ion Complexes A. Inorganic type B. Chelates C. Olefin type D. Aromatic type II. Organic Molecular Complexes A. Quinhydrone type B. Picric acid type C. Caffeine and other drug complexes D. Polymer type III. Inclusion Compounds A. Channel lattice type B. Layer type C. Clathrates D. Monomolecular type E. -

Coordination Chemistry
P r i m e r Coordination Chemistry Bonds in introductory chemistry are typically classified Ligands can be monodentate or multidentate. according to whether they are ionic or covalent in Monodentate ligands like ammonia would coordinate to character. Coordinate covalent bonds are a third the metal via one coordination point while a mulitdentate classification. In this type of bond, a lone pair of electrons ligand would coordinate to the metal via two or more from one chemical species is donated to an empty orbital points. Ethylene diamine (NH2CH2CH2NH2) is an example on another chemical species to form the new bond. This of a bidentate ligand because it coordinates to the metal is different from a covalent bond because both electrons through each of the two amine groups (-NH2). come from one atom or molecule but are shared as in a typical covalent bond. Unlike an ionic bond, a coordinate The number of coordination points in a complex is covalent bond does not rely on formal electrostatic referred to as the coordination number. Coordination attraction between a cation and an anion to form. numbers of six and four are the most common and result Ammonia-borane complexes are an example of this type in geometries that are octahedral (6), tetrahedral (4), or of bonding (Figure 1). square planar (4) (Figure 3). Figure 1: Ammonia-borane complexes contain a Figure 3: Common geometries of coordination complexes coordinate covalent bond where the lone pair of with coordination numbers of 6 and 4. electrons on ammonia (NH ) are donated to an empty p 3 Coordination numbers and geometries vary dramatically, orbital on borane (BH ) to give NH BH . -
Coordination Complexes
Coordination Complexes Chapter 20 What we learn from Chap 20 • We begin the chapter with what is among the most important coordination complexes of all, iron in hemoglobin (magnesium in chlorophyll might be another). In Section 20.1, we introduce the coordinate covalent bond and reintroduce Lewis acids (central atom) and bases (ligands) as the bonding species in coordination complexes. We also discuss how carbon monoxide can replace oxygen in hemoglobin. Copyright © Houghton Mifflin Company. All rights reserved. 20 | 2 Copyright © Houghton Mifflin Company. All rights reserved. 20 | 3 CHAPTER OUTLINE I. Bonding in Coordination Complexes II. Ligands III. Coordination Number IV. Structure V. Isomers VI. Formulas and Names A. Formulas B. Nomenclature VII. Color and Coordination Compounds A. Transition Metals and Color B. Crystal-Field Theory C. Orbital Occupancy D. The Result of d Orbital Splitting E. Magnetism VIII. Chemical Reactions A. Ligand Exchange Reactions B. Electron Transfer Reactions Copyright © Houghton Mifflin Company. All rights reserved. 20 | 4 20.1 Coordination Complex • Central metal atom – transition metal. • Coordinate covalent bond • Ligand – anion or neutral compound ·· such as H2O: or :NH3. 2+ [Cu(NH3)] 3- [Fe(CN)6] Copyright © Houghton Mifflin Company. All rights reserved. 20 | 5 Complexes Protein Ferrodoxin Plastocyanin Wilkin’s catalysyst Copyright © Houghton Mifflin Company. All rights reserved. 20 | 6 20.2 Ligands • Lewis bases having a lone pair of e- to donate. • Bidentate ligands form two bonds to the metal. • Chelates are polydentate ligands. Copyright © Houghton Mifflin Company. All rights reserved. 20 | 7 Ligand Names Copyright © Houghton Mifflin Company. All rights reserved. 20 | 8 Ligands Copyright © Houghton Mifflin Company. -

Lecture Based Modules for Bridge Course in Chemistry
Lecture Based Modules for Bridge Course in Chemistry All India Council for Technical Education Nelson Mandela Marg, Vasant Kunj, New Delhi 110 070 www.aicte-india.org I ALL INDIACOUNAL FAR TECI]NI'AL EOU'JlfION ph$ics, . rD _; L dute bosed Modules lot Bidae cou$es in Chenistto ond Mothendti.. PREFACE Globalization of the world economy and higher education are driving profound changes in cngincering education system. Worldwide adaptation of Outcome Based Education framework and enhanced focus on higher order learning and professional skills necessitates paradigm shift in traditional practices ofcurriculum design, education delivery and assessment. AICTE has also taken various quality initiatives for strengthening the technical education system in lndia. These initiatives are essential for promoting quality education in our institutions in the country so that our students passing out from these institutions may match the pace with global standards. A quality initiative by AICTE is 'Reyision of Curriculum'. Recently, AIC'I'E has released an outcome based Model Curriculum for various Undergraduate degree courses in Engineering & Technology which are available on AlCl'E website. A thrce-week mandatory induction program is developed as a part of the model curriculum for the first year UG Engineering students which helps students ,oining the first year of the college from diverse backgrounds to get adjusted in the new environment ofthe institution. Education is primarily conceived by students as one simple remembering facts by rote. However, Science education also requires clear understanding ofscience concepts and a proper logical thinking or a constructive thinking by students. We all know that the students seeking admission in an undergraduate degree engineering program have passed their 10+2 in science but it was felt that a student joining an engineering program after 10+2 require rein[orccment of fundamental science concepts i.e. -
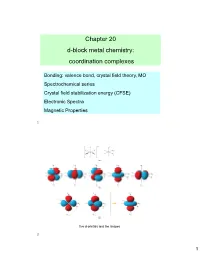
Chapter 20 D-Block Metal Chemistry: Coordination Complexes
Chapter 20 d-block metal chemistry: coordination complexes Bonding: valence bond, crystal field theory, MO Spectrochemical series Crystal field stabilization energy (CFSE) Electronic Spectra Magnetic Properties 1 five d-orbitals and the shapes 2 1 Hybridization schemes for the σ-bonding frameworks of different geometrical configurations 3 Limitations of VB Theory Vacant orbitals available to accept ligand electrons 3d 4s 4p Vacant orbitals available to accept ligand electrons 3d 2 3 Cr(III) d sp 3d d2sp3 Fe(III) For Fe(III), the two d orbitals in the sp3d2 hybrid orbitals would need to be from the 4d orbitals, which is not favorable because the 4d orbitals are much higher in energy than the 3d orbitals. 4 2 Crystal Field Theory (CFT) - - e - - e e e - - e e Mn+ e- e- e- e- - e- ∞ e Mn+ 12 e- rM-L Spherical Shell of e- density at rM-L 5 Crystal Field Stabilization Energy (CFSE) 2 3 3 o 2 o 5 5 6 3 The electronic absorption spectrum 3 of [Ti(OH2)6] in aqueous solution. 3d 7 Values of oct for some d-block metal complexes. 8 4 The trend in values of oct for 3 the complexes [M(NH3)6] where M = Co, Rh, Ir. Field strength increases as one proceeds down a column. oct Mn(II) < Ni(II) < Co(II) < Fe(II) < Cr(III) < Co(III) < Ru(III) < Mo(III) < Rh(III) < Pd(II) < Ir(III) < Pt(IV) 9 Factors affecting the CFSE First, note that the pairing energies for first-row transition metals are relatively constant. -

Synthesis, Properties, and Coordination Chemistry of T-Bu-Xantphos Ligands
Synthesis, Properties, and Coordination Chemistry of t-Bu-Xantphos Ligands by Melanie Ruth Maria Nelson A thesis submitted to the Victoria University of Wellington in fulfilment of the requirements for the degree of Doctor of Philosophy in Chemistry. Victoria University of Wellington 2015 Abstract This thesis provides an account of research into a group of diphosphine ligands with a rigid xanthene backbone and tert-butyl substituents on the phosphorus atoms. The three ligands have different groups in the bridgehead position of the backbone (CMe2, SiMe2, or S) which change the natural (calculated) bite-angle of the ligand. The coordination chemistry of these t-Bu-xantphos ligands with late-transition metals has been investigated with a focus on metal complexes that may form in catalytic reactions. The three t-Bu-xantphos ligands were synthesised by lithiation of the backbone t using sec-butyllithium/TMEDA and treatment with P Bu2Cl. The natural bite- angles of the Ph-xantphos (111.89–114.18◦) and t-Bu-xantphos (126.80–127.56◦) ligands were calculated using DFT. The bite-angle of the t-Bu-xantphos ligands is larger due to the increased steric bulk of the tert-butyl substituents. The elec- tronic properties of the t-Bu-xantphos ligands were also investigated by synthesis 1 of their phosphine selenides. The values of J PSe (689.1–698.5 Hz) indicate that the t-Bu-xantphos ligands have a higher basicity than Ph-xantphos between PPh2Me and PMe3. The silver complexes, [Ag(t-Bu-xantphos)Cl] and [Ag(t-Bu-xantphos)]BF4 were synthesised with the t-Bu-xantphos ligands. -

The Coordination Chemistry of Solvated Metal Ions in DMPU
The Coordination Chemistry of Solvated Metal Ions in DMPU A Study of a Space-Demanding Solvent Daniel Lundberg Faculty of Natural Resources and Agricultural Sciences Department of Chemistry Uppsala Doctoral thesis Swedish University of Agricultural Sciences Uppsala 2006 Acta Universitatis Agriculturae Sueciae 2006: 23 ISSN 1652-6880 ISBN 91-576-7072-2 © 2006 Daniel Lundberg, Uppsala Tryck: SLU Service/Repro, Uppsala 2006 Abstract Lundberg, D., 2006, The Coordination Chemistry of Solvated Metal Ions in DMPU – A Study of a Space-Demanding Solvent. Doctor’s dissertation. ISSN 1652-6880, ISBN 91-576-7072-2 This thesis summarizes and discusses the results of several individual studies on the solvation of metal ions in the solvent N,N’-dimethylpropyleneurea, DMPU, including the iron(II), iron(III), zinc(II), cadmium(II), and lanthanoid(III) ions. These studies have shown that the solvation process in DMPU is sometimes very different to those in corresponding aqueous systems. This is due to the the space-demanding properties the DMPU molecule has when coordinating to metal ions, with its two methyl groups close to the coordinating oxygen atom. The methyl groups effectively hinder/hamper the metal ion from reaching the coordination numbers present in hydrate and solvate complexes with solvent molecules with much lower spatial demands. The investigations were performed with different X-ray techniques, including extended X-ray absorption fine structure (EXAFS), large angle X-ray scattering (LAXS), and single crystal X-ray diffraction (XRD) and included both studies in solution (EXAFS and LAXS) and solid state (EXAFS and XRD). A coordination number reduction, compared to the corresponding hydrates, was found in all of the studied systems, except cadmium(II). -

Emergence of On-Surface Magnetochemistry § ‡ ‡ † ‡ Nirmalya Ballav,*, Christian Wackerlin,̈ Dorota Siewert, Peter M
Perspective pubs.acs.org/JPCL Emergence of On-Surface Magnetochemistry § ‡ ‡ † ‡ Nirmalya Ballav,*, Christian Wackerlin,̈ Dorota Siewert, Peter M. Oppeneer, and Thomas A. Jung*, § Department of Chemistry, Indian Institute of Science Education and Research (IISER), Pashan, Pune 411 008, India ‡ Laboratory for Micro and Nanotechnology, Paul Scherrer Institute, 5232 Villigen PSI, Switzerland † Department of Physics and Astronomy, Uppsala University, Box 516, S-751 20 Uppsala, Sweden ABSTRACT: The control of exchange coupling across the molecule−substrate interface is a key feature in molecular spintronics. This Perspective reviews the emerging field of on-surface magnetochemistry, where coordination chemistry is applied to surface-supported metal porphyrins and metal phthalocyanines to control their magnetic properties. The particularities of the surface as a multiatomic ligand or “surface ligand” are introduced. The asymmetry involved in the action of a chemical ligand and a surface ligand on the same planar complexes modifies the well-established “trans effect” to the notion of the “surface-trans effect”. As ad-complexes on ferromagnetic substrates are usually exchange-coupled, the magnetochemical implications of the surface-trans effect are of particular interest. The combined action of the different ligands allows for the reproducible control of spin states in on-surface supramolecular architectures and opens up new ways toward building and operating spin systems at interfaces. Notably, spin-switching has been demonstrated to be controlled collectively via the interaction with a ligand (chemical selectivity) and individually via local addressing at the interface. century ago, Alfred Werner laid the foundation of modern Emerging evidence shows that A coordination chemistry, an achievement for which he was awarded the Nobel Prize in Chemistry in 1913.