The Pathophysiology and Treatment of Malignancy-Associated Hypercalcemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Multicenter Trial of Low Dose Gallium Nitrate in Patients with Advanced Paget’S Disease of Bone
Vol. 80. No. 2 Journalof CbnicalEndocrinology and Metabolism Pr’rrnrrd ,,, IJ S.A. CopyrIght0 1995by The EndocrineSociety A Multicenter Trial of Low Dose Gallium Nitrate in Patients with Advanced Paget’s Disease of Bone RICHARD S. BOCKMAN, FRANCOIS WILHELM, ETHEL SIRIS, FREDERICK SINGER, ARTHUR CHAUSMER*, RACHELLE BITTON, JON KOTLER, BARBARA J. BOSCO, DAVID R. EYRE, AND DAVID LEVENSON Department of Medicine, Hospital for Special Surgery and Cornell University Medical College (R.S.B., B.J.B., D.L.), New York, New York 10021; Research and Development, Fujisawa Pharmaceutical Co. (F.W.), Deer-field, Illinois 60015; Columbia University College of Physicians and Surgeons (E.S.), New York, New York 10032; St. John’s Hospital and Health Center, John Wayne Cancer Institute (F.S.1, Santa Monica, California 90404; the Division of Endocrinology, Long Island Jewish Hospital (R.B.1, New Hyde Park, New York 11042; Holy Cross Hospital (J.K.), Ft. Lauderdale, Florida 33008; and the Department of Orthopaedics, University of Washington (D.R.E.), Seattle, Washington 98195 ABSTRACT treated with the 0.5 mg/kg.day dose achieved a 50% or more reduction Gallium nitrate is a potent antiresorptive drug that has been ex- in enzyme activity. The nadir value in hydraxyproline excretion oc- tensively tested in patients with accelerated bone turnover. We have curred at 10 weeks, with mean changes of +9%, -lo%, and ~ 17% for evaluated the effects of this new agent in a pilot multicenter trial of the 0.05, 0.25, and 0.5 mg/kg.day doses, respectively; the difference 49 patients with advanced Paget’s disease of bone. -

Report of the Advisory Group to Recommend Priorities for the IARC Monographs During 2020–2024
IARC Monographs on the Identification of Carcinogenic Hazards to Humans Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 CONTENTS Introduction ................................................................................................................................... 1 Acetaldehyde (CAS No. 75-07-0) ................................................................................................. 3 Acrolein (CAS No. 107-02-8) ....................................................................................................... 4 Acrylamide (CAS No. 79-06-1) .................................................................................................... 5 Acrylonitrile (CAS No. 107-13-1) ................................................................................................ 6 Aflatoxins (CAS No. 1402-68-2) .................................................................................................. 8 Air pollutants and underlying mechanisms for breast cancer ....................................................... 9 Airborne gram-negative bacterial endotoxins ............................................................................. 10 Alachlor (chloroacetanilide herbicide) (CAS No. 15972-60-8) .................................................. 10 Aluminium (CAS No. 7429-90-5) .............................................................................................. 11 -
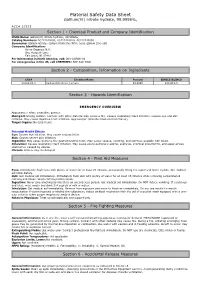
Material Safety Data Sheet
Material Safety Data Sheet Gallium(iii) nitrate hydrate, 99.9998%, ACC# 27373 Section 1 - Chemical Product and Company Identification MSDS Name: Gallium(iii) nitrate hydrate, 99.9998%, Catalog Numbers: AC212440000, AC212440010, AC212440050 Synonyms: Gallium nitrate; Gallium trinitrate; Nitric acid, gallium (3+) salt Company Identification: Acros Organics N.V. One Reagent Lane Fair Lawn, NJ 07410 For information in North America, call: 800-ACROS-01 For emergencies in the US, call CHEMTREC: 800-424-9300 Section 2 - Composition, Information on Ingredients CAS# Chemical Name Percent EINECS/ELINCS 13494-90-1 Gallium(III) nitrate hydrate 99.9998 236-815-5 Section 3 - Hazards Identification EMERGENCY OVERVIEW Appearance: white crystalline powder. Danger! Strong oxidizer. Contact with other material may cause a fire. Causes respiratory tract irritation. Causes eye and skin irritation. May cause digestive tract irritation. Hygroscopic (absorbs moisture from the air). Target Organs: No data found. Potential Health Effects Eye: Causes eye irritation. May cause conjunctivitis. Skin: Causes severe skin irritation. Ingestion: May cause burns to the gastrointestinal tract. May cause nausea, vomiting, and diarrhea, possibly with blood. Inhalation: Causes respiratory tract irritation. May cause acute pulmonary edema, asphyxia, chemical pneumonitis, and upper airway obstruction caused by edema. Chronic: Effects may be delayed. Section 4 - First Aid Measures Eyes: Immediately flush eyes with plenty of water for at least 15 minutes, occasionally lifting the upper and lower eyelids. Get medical aid imme diately. Skin: Get medical aid immediately. Immediately flush skin with plenty of water for at least 15 minutes while removing contaminated clothing and shoes. Wash clothing before reuse. Ingestion: Never give anything by mouth to an unconscious person. -

Elimination of Arthritis Pain and Inflammation for Over Two Years With
Artrite por 2 anos tratada com aplicação local por 90 minutos com nitrato de gálio a 14% Elimination of arthritis pain and inflammation for over two years with a single 90 minute, topical 14% gallium nitrate treatment: Case reports and review of actions of gallium III. - Medical Hypotheses Vol 65/6 pp 1136-1141 by George Eby Austin, Texas See abstract at Elsevier Science Direct here See PDF version of published article here Abstract Arthritis is inflammation in a joint often with joint damage, usually accompanied by pain, swelling and stiffness, resulting from infection, trauma, degenerative changes, metabolic disturbances, autoimmune or other causes. It occurs in various forms, including rheumatoid arthritis, osteoarthritis, bacterial arthritis and gout. Gallium III can inhibit the production of inflammatory cytokines, such as IL-1beta, produced by macrophage-like cells in vitro. A dose-dependent inhibition of IL-1beta and TPA stimulated MMP activity by gallium nitrate at increasing concentrations occurs, demonstrating that gallium nitrate can be a useful modulator of inflammation in arthritis. Gallium III is an inhibitor of bone resorption and is an effective treatment for hypercalcemia. Gallium III has been reported to be effective in the treatment of mycobacterium butycicum-induced arthritis in rats by antagonism of iron III. Long-term elimination of pain from arthritis by gallium III was first observed in horses primarily being treated for navicular disease. Several people treating their horses with gallium nitrate coincidentally found that arthritis pain in their fingers ended and did not return after soaking their hands in 14% gallium nitrate solution. Therefore, the severely arthritic hands of a 60-year old woman were topically treated with a 14% aqueous solution of gallium nitrate for 90 minutes. -

University of Stockholm
UNIVERSITY OF STOCKHOLM INSTITUTE OF PHYSICS NEW METALS — A study on the use of and exposure to certain metals and their compounds from a toxicological viewpoint U. BERGQVIST USIP Report 83 - 11 December 1983 NEW METALS A study on the use of and exposure to certain metals and their compounds from a toxicological viewpoint Ulf Bergqvist, with contributions from Foad Vojdani Ghamsari Theoretical Physics, University of Stockholm Vanadisvägen 9, S—113 46 Stockholm, Sweden I'm still confused - but on a higher level USIP Report 83--1 December 1983 - I - LIST OF CONTENTS (IN BRIEF) Page: List of contents (in brief) I List of contents (in details) III Acknowledgements X Disposition of this report XI Introduction 1 Section 1: Exposure to metals and metal compounds Preamble 3-6 Criteria based on total world consumption 7-13 Criteria based on probable increases in world metal consumption 1 4-22 Criteria based on exposure to metal emissions from sources other than metal consumption 23-29 Reconfirmation of metals found interesting in this section 30-33 Summary of section 1 34-38 Section 2: ' 1 e extent of toxicological knowledge and * search on metals and their compounds Preamb c 39-42 The re.://ch activity on toxic effects of metals ,nd metal compounds 43-49 Differe t organisms responses to metal compounds 50-r54 Introciu :• ,ion of new metal compounds in industrial consumption and its toxicological impli- cation 55-60 An es . mate of the quantity of toxicological infor- mation on metal and metal compounds in reviews 61-65 An evaluation of the relevance of available toxico- logical information to present and future industrial consumption of certain metals 66-72 Summar. -

Gallium and Bone Pathology
ARTIGO DE REVISÂO O GÁLIO E A PATOLOGIA ÓSSEA GALLIUM AND BONE PATHOLOGY PETR MELNIKOV1, AUGUSTIN MALZAC2, MARLENE DE BARROS COELHO3 RESUMO SUMMARY Proposta: Revisão de trabalhos científicos referentes à incorporação Purpose: To review the literature concerning the incorporation do gálio no tecido ósseo, ao mecanismo da atividade terapêutica of gallium into bone tissue, mechanisms of therapeutic activity desse elemento, bem como a formação, crescimento e solubili- of this element, as well as the formation, growth and solubility dade da hidroxiapatita na presença dos sais de gálio.Justificativa: of hydroxiapatite in the presence of gallium salts. Justification: Diferente de outras drogas que impedem a perda de cálcio, os sais In contrast to other calcium-saving drugs, salts of trace element de elemento traço gálio são eficazes em hipercalcemia severa. O gallium are effective in severe hypercalcemias. Gallium (most gálio (geralmente na forma de nitrato) aumenta a concentração commonly in the form of its nitrate) enhances calcium and de cálcio e fósforo no osso, influindo nos osteoclastos de maneira phosphorus content of the bone and has direct, noncytotoxic direta não tóxica, em doses surpreendentemente baixas. Apesar effects on osteoclasts at markedly low doses. Although the de que os detalhes do mecanismo de ação do gálio não são bem details of gallium action on the bone are still uncertain, it is well esclarecidos, está comprovado que esse mecanismo envolve a established that the mechanism involves gallium insertion into inserção do gálio na matriz de hidroxiapatita, protegendo-a contra the hydroxiapatite matrix protecting it from resorbtion and impro- a reabsorção e melhorando as propriedades biomecânicas do ving biomechanical properties of the skeletal system. -

Uncommon Heavy Metals, Metalloids and Their Plant Toxicity: a Review
Environ Chem Lett (2008) 6:189–213 DOI 10.1007/s10311-008-0159-9 REVIEW Uncommon heavy metals, metalloids and their plant toxicity: a review Petr Babula Æ Vojtech Adam Æ Radka Opatrilova Æ Josef Zehnalek Æ Ladislav Havel Æ Rene Kizek Received: 8 April 2008 / Accepted: 29 April 2008 / Published online: 13 June 2008 Ó Springer-Verlag 2008 Abstract Heavy metals still represent a group of danger- gadolinium, holmium, lutetium, neodymium, promethium, ous pollutants, to which close attention is paid. Many heavy praseodymium, samarium, terbium, thulium and ytterbium. metals are essential as important constituents of pigments and enzymes, mainly zinc, nickel and copper. However, all Keywords Heavy metals Á Plant Á Phytoremediation metals, especially cadmium, lead, mercury and copper, are toxic at high concentration because of disrupting enzyme functions, replacing essential metals in pigments or pro- Introduction ducing reactive oxygen species. The toxicity of less common heavy metals and metalloids, such as thallium, arsenic, Fate of heavy metals in environment as well as their tox- chromium, antimony, selenium and bismuth, has been icity and other properties are still topical. This fact can be investigated. Here, we review the phytotoxicity of thallium, well documented in enhancing the count of article, where chromium, antimony, selenium, bismuth, and other rare ‘‘Plant and heavy metal’’ term has been found within article heavy metals and metalloids such as tellurium, germanium, titles, abstract and keywords (Fig. 1). The enhancement gallium, scandium, gold, platinum group metals (palladium, is probably related with concern, in ensuring sufficient platinum and rhodium), technetium, tungsten, uranium, foodstuffs. Moreover, there have been developing tech- thorium, and rare earth elements yttrium and lanthanum, and nologies to remediate environment polluted by heavy the 14 lanthanides cerium, dysprosium, erbium, europium, metals. -

Gene Expression Analysis of Gallium
633 Gene expression analysis of gallium-resistant and gallium- sensitive lymphoma cells reveals a role for metal- responsive transcription factor-1, metallothionein-2A, and zinc transporter-1 in modulating the antineoplastic activity of gallium nitrate Meiying Yang,1 Steven H.Kroft, 2 gallium nitrate. Immunohistochemical staining of lympho- and Christopher R.Chitambar 1 matous tissues revealed metallothionein protein to be variably expressed in different lymphomas. Our studies 1Division of Neoplastic Diseases, Department of Medicine and show for the first time that gallium acts on pathways 2 Department of Pathology, Medical College of Wisconsin, related to zinc metabolism and that metal-responsive Milwaukee, Wisconsin transcription factor-1 activity and metallothionein expres- sion contribute to the development of gallium drug Abstract resistance. Furthermore, the endogenous level of metal- Several clinical trials have shown gallium nitrate to be lothionein in lymphoma may be an important determinant an active agent in the treatment of lymphoma. Whereas of clinical response to gallium nitrate. [Mol Cancer Ther gallium is known to target cellular iron homeostasis, the 2007;6(2):633–43] basis for lymphoma cell resistance to gallium is not known. Understanding mechanisms of resistance may Introduction suggest strategies to enhance the clinical efficacy of gallium. In the present study, we used a focused DNA Over the past two decades, several clinical studies have microarray to compare the expression of genes related shown the group IIIa metal salt gallium nitrate to have to metal metabolism in gallium-resistant and gallium- efficacy in the treatment of non-Hodgkin’s lymphoma (1–5). sensitive lymphoma cell lines developed by us. -

Investigation of Novel Nanoparticles of Gallium Ferricyanide and Gallium Lawsonate As Potential Anticancer Agents, and Nanoparti
Investigation of Novel Nanoparticles of Gallium Ferricyanide and Gallium Lawsonate as Potential Anticancer Agents, and Nanoparticles of Novel Bismuth Tetrathiotungstate as Promising CT Contrast Agent A Thesis submitted to Kent State University In partial fulfillment of the requirements for the degree of Master of Science Liu Yang August 2014 Thesis written by Liu Yang B.S. Kent State University, 2013 M.S. Kent State University, 2014 Approved by ___________________________________, Advisor, Committee member Dr. Songping Huang ___________________________________, Committee member Dr. Scott Bunge ___________________________________, Committee member Dr. Mietek Jaroniec Accepted by ___________________________________, Chair, Department of Chemistry Dr. Michael Tubergen ___________________________________, Dean, College of Arts and Sciences Dr. James L. Blank ii Table of Contents List of Figures..…………………………………………………………………........vii Acknowledgements ……………………………………………………………….….xi Chapter 1: Summary, Materials and Methods …..……………………………………1 1.1 Materials ………………………………………………………………….3 1.1.1 carboxymethyl reduced polysaccharide (CMRD) preparation….3 1.2 Methods …………………………………………………………………4 1.2.1 Atomic absorption spectroscopy (AA) …………………………4 1.2.2 Acid base treating method ……………………………………...4 1.2.3 Cell viability study ……………………………………………...5 i) MTT assay…………………………………………………..5 ii) Trypan blue assay ………………………………………….6 1.2.4 Dialysis …………………………………………………………6 1.2.5 Elementary analysis …………………………………………….7 1.2.6 Lyophilization …………………………………………………..7 iii 1.2.7 -

Sensitive Lymphoma Cells Reveals a Role for Metal- Responsive Transcr
633 Gene expression analysis of gallium-resistant and gallium- sensitive lymphoma cells reveals a role for metal- responsive transcription factor-1, metallothionein-2A, and zinc transporter-1 in modulating the antineoplastic activity of gallium nitrate Meiying Yang,1 Steven H.Kroft, 2 gallium nitrate. Immunohistochemical staining of lympho- and Christopher R.Chitambar 1 matous tissues revealed metallothionein protein to be variably expressed in different lymphomas. Our studies 1Division of Neoplastic Diseases, Department of Medicine and show for the first time that gallium acts on pathways 2 Department of Pathology, Medical College of Wisconsin, related to zinc metabolism and that metal-responsive Milwaukee, Wisconsin transcription factor-1 activity and metallothionein expres- sion contribute to the development of gallium drug Abstract resistance. Furthermore, the endogenous level of metal- Several clinical trials have shown gallium nitrate to be lothionein in lymphoma may be an important determinant an active agent in the treatment of lymphoma. Whereas of clinical response to gallium nitrate. [Mol Cancer Ther gallium is known to target cellular iron homeostasis, the 2007;6(2):633–43] basis for lymphoma cell resistance to gallium is not known. Understanding mechanisms of resistance may Introduction suggest strategies to enhance the clinical efficacy of gallium. In the present study, we used a focused DNA Over the past two decades, several clinical studies have microarray to compare the expression of genes related shown the group IIIa metal salt gallium nitrate to have to metal metabolism in gallium-resistant and gallium- efficacy in the treatment of non-Hodgkin’s lymphoma (1–5). sensitive lymphoma cell lines developed by us. -

[email protected] +1-703-527-3887 (International) Website
Date of Issue: 14 May 2014 SAFETY DATA SHEET 1. SUBSTANCE AND SOURCE IDENTIFICATION Product Identifier SRM Number: 3119a SRM Name: Gallium (Ga) Standard Solution Other Means of Identification: Not applicable. Recommended Use of This Material and Restrictions of Use This Standard Reference Material (SRM) is intended for use as a primary calibration standard for the quantitative determination of gallium. A unit of SRM 3119a consists of five 10 mL sealed borosilicate glass ampoules of an acidified aqueous solution prepared gravimetrically to contain a known mass fraction of gallium. The solution contains nitric acid at a volume fraction of approximately 10 %. Company Information National Institute of Standards and Technology Standard Reference Materials Program 100 Bureau Drive, Stop 2300 Gaithersburg, Maryland 20899-2300 Telephone: 301-975-2200 Emergency Telephone ChemTrec: FAX: 301-948-3730 1-800-424-9300 (North America) E-mail: [email protected] +1-703-527-3887 (International) Website: http://www.nist.gov/srm 2. HAZARDS IDENTIFICATION Classification Physical Hazard: Not classified. Health Hazard: Skin Corrosion/Irritation Category 1B Serious Eye Damage/Eye Irritation Category 1 Label Elements Symbol Signal Word DANGER Hazard Statement(s) H314 Causes severe skin burns and eye damage. Precautionary Statement(s) P260 Do not breathe fumes, mists, vapors, or spray. P264 Wash hands thoroughly after handling. P280 Wear protective gloves, protective clothing, and eye protection. P301 + P330 + P331 If swallowed: Rinse mouth. Do NOT induce vomiting. P303 + P361 + P353 If on skin (or hair): Remove immediately all contaminated clothing. Rinse skin with water. P304 + P340 If inhaled: Remove person to fresh air and keep comfortable for breathing. -

Gallium Arsenide
pp 163-196.qxp 31/05/2006 10:18 Page 163 GALLIUM ARSENIDE 1. Exposure Data 1.1 Chemical and physical data 1.1.1 Nomenclature Chem. Abstr. Serv. Reg. No.: 1303-00-0 Deleted CAS Reg. No.: 12254-95-4, 106495-92-5, 116443-03-9, 385800-12-4 Chem. Abstr. Serv. Name: Gallium arsenide (GaAs) IUPAC Systematic Name: Gallium arsenide Synonyms: Gallium monoarsenide 1.1.2 Molecular formula and relative molecular mass GaAs Relative molecular mass: 144.6 1.1.3 Chemical and physical properties of the pure substance (a) Description: Grey, cubic crystals (Lide, 2003) (b) Melting-point: 1238 °C (Lide, 2003) (c) Density: 5.3176 g/cm3 (Lide, 2003) (d) Solubility: Insoluble in water (Wafer Technology Ltd, 1997); slightly soluble in 0.1 M phosphate buffer at pH 7.4 (Webb et al., 1984) (e) Stability: Decomposes with evolution of arsenic vapour at temperatures above 480 °C (Wafer Technology Ltd, 1997) (f) Reactivity: Reacts with strong acid reducing agents to produce arsine gas (Wafer Technology Ltd, 1997) 1.1.4 Technical products and impurities Purity requirements for the raw materials used to produce gallium arsenide are stringent. For optoelectronic devices (light-emitting diodes (LEDs), laser diodes, photo- detectors, solar cells), the gallium and arsenic must be at least 99.9999% pure; for –163– pp 163-196.qxp 31/05/2006 10:18 Page 164 164 IARC MONOGRAPHS VOLUME 86 integrated circuits, a purity of 99.99999% is required. These purity levels are referred to by several names: 99.9999%-pure gallium is often called 6-nines, 6N or optoelectronic grade, while 99.99999%-pure gallium is called 7-nines, 7N, semi-insulating (SI) or integrated circuit (IC) grade.