Functional Medicine Approach to Identification and Management of Insulin Resistance: a Literature Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Checking Blood Sugar Levels
Checking Blood Sugar Levels People with type 1 diabetes (T1D) must check their blood sugar (glucose) levels throughout the day using a blood glucose meter. The meter tells them how much glucose is in their blood at that particular moment. Based upon the reading, they take insulin, eat, or modify activity to keep blood sugars within their target range. Regularly checking blood sugar levels is an essential part of T1D care. Methods for Checking Blood Sugar Levels Checking, or testing, involves taking a drop of blood, usually from the fingertip, and placing it on a special test strip in a glucose meter. Blood sugar meters are easy to use, and even young children often learn quickly how to do their own blood sugar checks. In order to properly manage their diabetes, individuals with T1D check their blood sugar levels several times per day. For example, they may test before eating lunch and before strenuous exercise. Blood sugar levels are measured in milligrams per deciliter (mg/dL). A normal blood sugar level is between 70 and 120 mg/dL. Keeping blood sugar levels within this range may be difficult in children with diabetes. Therefore, an individual's doctor may adjust the target range (for example, 80-180 mg/dL). However, people with diabetes can't always maintain blood sugar levels within the target range, no matter how hard they try. A person's varying schedules and eating habits, as well as the physical changes that occur as they grow, can send blood sugar levels out of range for no apparent reason. -

Decrease of Fructosamine Levels During Treatment with Adalimumab
European Journal of Endocrinology (2007) 156 291–293 ISSN 0804-4643 CASE REPORT Decrease of fructosamine levels during treatment with adalimumab in patients with both diabetes and rheumatoid arthritis I C van Eijk1, M J L Peters1,2, M T Nurmohamed1,2,3, A W van Deutekom4, B A C Dijkmans1,2 and S Simsek4 1Department of Rheumatology, Jan van Breemen Institute, Amsterdam, The Netherlands, 2Department of Rheumatology, VU University Medical Center, Amsterdam, The Netherlands, 3Department of Internal Medicine, VU University Medical Center, Amsterdam, The Netherlands and 4Department of Endocrinology/Diabetes Center, VU University Medical Center, PO Box 7057, 1007 MB, Boelelaan 1117, Amsterdam, The Netherlands (Correspondence should be addressed to S Simsek; Email: [email protected]) Abstract Tumour necrosis factor a (TNFa) is a pro-inflammatory cytokine which has been closely linked to obesity and insulin resistance. We present two cases of patients with rheumatoid arthritis (RA) and concomitant diabetes mellitus, who showed a marked decrease of fructosamine levels after initiating therapy with adalimumab, a TNFa-blocking agent, for active RA. This finding may implicate that TNFa blockade causes better glycaemic control in RA patients with concomitant diabetes, possibly by improving insulin resistance. European Journal of Endocrinology 156 291–293 Introduction Research design and methods Tumour necrosis factor a (TNFa), a pro-inflammatory A patient with known diabetes type 1 and concomitant cytokine, plays an important role in inflammatory and RA showed a marked improvement of HbA1c levels after autoimmune diseases like rheumatoid arthritis (RA). initiation of adalimumab, a recombinant human IgG1- TNFa has also been closely linked to obesity and insulin MAB, therapy for active RA when she visited the resistance (1). -

Hba1c Matters
HbA1c Matters What is HbA1c? The HbA1c reading reveals your average blood sugar level over the past three months. When blood sugar levels are high, sugar attaches to the red blood cells. The HbA1c monitors how much sugar is attached to the red blood cells, which have a lifespan of about 3 months. The HbA1c reading is therefore able to show what your average blood sugar levels have been in the last 3 months. The units we report HbA1c in are changing, and in the future you will see it reported as a whole number rather than a percentage. Both units are given below. Why does it matter? HbA1c levels are linked with risk of diabetes complications, with higher readings increasing the chance of problems. This is illustrated in the graph below. 15 13 Retinopathy 11 Nephropathy Relative 9 Risk 7 Neuropathy 5 Microalbuminuria 3 1 6 7 8 9 10 11 12 Previous method % 42 53 64 75 86 97 108 New IFCC method HbA1c The graph shows the risk of complications associated with diabetes including retinopathy (eye damage that can lead to blindness), nephropathy (kidney damage that can lead to kidney failure and a need for dialysis), neuropathy (damage to the nerves) and microalbuminuria (protein in the urine which is associated with kidney damage). When HbA1c levels are below 7.5% or 58 mmol/mol, the risk of each of these complications is very low – approximately equivalent to people who do not have diabetes. The risk of each complication rises increasingly steeply as HbA1c levels rise above 7.5% or 58 mmol/mol. -

Diabetes Is a Disease in Which the Body's Ability to Produce Or Respond
Early Signs and Symptoms of diabetes: Early symptoms of diabetes, especially type 2 diabetes, can be subtle or seemingly harmless. Over time, however, you may Diabetes is a disease in which the develop diabetes complications, even if you body’s ability to produce or respond to haven't had diabetes symptoms. In the the hormone insulin is impaired, United States alone, more than 8 million resulting in abnormal metabolism of people have undiagnosed diabetes, Treatments: carbohydrates and elevated levels of according to the American Diabetes Association. Understanding possible glucose (sugar) in the blood. • Insulin therapy diabetes symptoms can lead to early • Oral medications diagnosis and treatment and a lifetime of Diabetes can be broken down into • better health. If you're experiencing any of Diet changes two types, Type 1 and Type 2. Type 1 • Exercise diabetes involves the the following diabetes signs and symptoms, see your doctor. body attacking itself by The medications you take vary by mistake, this then the type of diabetes and how well the causes the body to stop making insulin. With medicine controls you blood glucose levels. Type 2 diabetes the Type 1 diabetics must have insulin. Type 2 body does not respond may or may not include insulin and may just like it should to the be controlled with diet and exercise alone. insulin the pancreas is If you notice any of these changes notify making. Your body tells the pancreas that it needs to make more insulin since the your health care provider. The earlier • insulin that is already there is not working. -

Deducing Serum Fructosamine Levels from the Fasting Blood Glucose Value: a Preliminary Study H
http://doi.org/10.4038/cjms.v44i2.4863 Deducing serum fructosamine levels from the fasting blood glucose value: a preliminary study H. Perns' The Ceylon Journal of Medical Science 2001; 44:25-28 Abstract However, recent studies have shown that fructosamine (glycated protein) can be used to The determination of glycated serum proteins differentiate between well and poorly stabilized (fructosamine) has become an accepted index for diabetics (1). Fructosamines are stable keto- assessing the metabolic situation in diabetic amines formed by a non-enzymatic reaction patients. The current study describes an alternative between a sugar and a protein. It has been known to measurement of fructosamine level, viz., to that a number of proteins, e.g., haemoglobin, predict the serum fructosamine based on the serum proteins, membrane proteins, protein in glucose concentration in fasting plasma. A cross- the lens of eye etc. are glycated by a non- sectional prospective study was performed on 44 enzymatic reaction and forms a stable fructo non-diabetic, 38 impaired glucose tolerance and samine (isoglucosamine) which depends on the 38 diabetic subjects attending clinics at Colombo glucose concentration. The glycated serum South Teaching Hospital. Fasting plasma glucose proteins form very quickly with changes in the and corresponding serum fructosamine glucose concentration than the glycated concentrations were determined on all subjects. haemoglobin (HbA ) formed in the erythrocytes. Fructosamine showed a positive linear correlation ]c The largest fraction, about 60-70% of glycated of r2 = 0.85 with the fasting plasma glucose serum proteins, consists of albumin with a half- concentrations. Regression equation relating to life in serum about 2-3 weeks (2). -

Liquid QC™ Bilirubin Control
Hemoglobin A1C Reagent ® INTENDED USE FOR IN VITRO DIAGNOSTIC USE No special additives or preservatives other than anticoagulants are required. Collect Hemoglobin A1c (HbA1c) Reagent is intended for the quantitative determination of venous blood with EDTA using aseptic technique. Hemoglobin A1c in human blood. INTERFERING SUBSTANCES SUMMARY Bilrubin to 50 mg/dl, ascorbic acid to 50 mg/dl, triglycerides to 2000 mg/dl, The determination of HbA1c is most commonly performed for the evaluation of carbamylated Hb to 7.5 mmol/L and acetylated Hb to 5.0 mmol/L do not interfere with glycemic control in diabetes mellitus. HbA1c values provide an indication of glucose this assay. See also the LIMITATION SECTION. levels over the preceding 4-8 weeks. A higher HbA1c value indicates poorer glycemic control. PROCEDURE Throughout the circulatory life of the red cell, HbA1c is formed continuously by the Materials provided adduction of glucose to the N-terminal of the hemoglobin beta chain. This process, 85621 R1 1 x 30 mL which is non-enzymatic, reflects the average exposure of hemoglobin to glucose over R2A 1 x 9.5 mL an extended period. In a classical study, Trivelli, et al, (10.1) showed HbA1c in diabetic subjects to be elevated 2-3 fold over the levels found in normal individuals. R2B 1 x 0.5 mL Several investigators have recommended HbA1c serve as an indicator of metabolic R3 1 x 200 mL control of the diabetic, since HbA1c levels approach normal levels for diabetics in metabolic control. (10.2,10.3,10.4) HBA1c has been defined operationally as the “fast Materials required but not provided fraction” hemoglobins (HbA , A , A ) that elute first during column chromatography 1a 1b 1c 1. -

Prediabetes: What Is It and What Can I Do?
Prediabetes: What Is It and What Can I Do? What is prediabetes? Weight loss can delay or prevent diabetes. Prediabetes is a condition that comes before Reaching a healthy weight can help you a lot. diabetes. It means your blood glucose levels are If you’re overweight, any weight loss, even higher than normal but aren’t high enough to be 7 percent of your weight (for example, losing called diabetes. about 15 pounds if you weigh 200), may lower your risk for diabetes. There are no clear symptoms of prediabetes. You can have it and not know it. If I have prediabetes, what does it mean? It means you might get type 2 diabetes soon or down the road. You are also more likely to get heart disease or have a stroke. The good news is that you can take steps to delay or prevent type 2 diabetes. How can I delay or prevent type 2 diabetes? You may be able to delay or prevent type 2 diabetes with: Daily physical activity, such as walking. Weight loss, if needed. Losing even a few pounds will help. Medication, if your doctor prescribes it. If you have prediabetes, these steps may bring your blood glucose to a normal range. But you are still at a higher risk for type 2 diabetes. Regular physical activity can delay or prevent diabetes. Being active is one of the best ways to delay or prevent type 2 diabetes. It can also lower your weight and blood pressure, and improve cholesterol levels. Ask your health care team about activities that are safe for you. -

Insulin Sensitivity and Resistin Levels in Gestational Diabetes Mellitus And
European Journal of Endocrinology (2008) 158 173–178 ISSN 0804-4643 CLINICAL STUDY Insulin sensitivity and resistin levels in gestational diabetes mellitus and after parturition Ana Megia, Joan Vendrell, Cristina Gutierrez, Modest Sabate´1, Montse Broch, Jose´-Manuel Ferna´ndez-Real2 and Inmaculada Simo´n Endocrinology and Diabetes Research Department, University Hospital of Tarragona ‘Joan XXIII’, ‘Pere Virgili’ Institute, ‘Rovira i Virgili’ University, 43007, Tarragona, Spain, 1Laboratory Department, Hospital ‘ St Pau i Sta. Tecla’, 43003, Tarragona, Spain and 2Endocrinology and Diabetes Unit, University Hospital ‘Josep Trueta’, 17007, Girona, Spain (Correspondence should be addressed to A Megia who is now at Seccio´ d’endocrinologı´a, Hospital Universitari ‘Joan XXIII’ de Tarragona, c/Mallafre´ Guasch, 4.43007 Tarragona, Spain; Email: [email protected]) Abstract Context: Resistin is expressed and secreted by the placenta during pregnancy. Increased serum resistin levels have been found in the second half of normal pregnancy, but its role in the pathogenesis of the insulin resistance of pregnancy is undetermined. Objective: The objective of the study was to assess the relationship between circulating resistin levels and insulin sensitivity in gestational diabetes mellitus (GDM). Design and setting: A case (nZ23)–control (nZ35) study was performed at the obstetrics and endocrinology clinic of a university hospital. Patients: In total, 58 Caucasian women with a singleton pregnancy who had been referred for a 100 g oral glucose tolerance test were enrolled between the weeks 26 and 30, and 22 women with GDM were also evaluated after pregnancy. Main outcome measures: Serum resistin and insulin sensitivity in GDM during and after pregnancy. The relationship of resistin to metabolic abnormalities was evaluated. -

89 Abstract a Study of Gamma
89 A STUDY OF GAMMA-GLUTAMYLTRANSFERASE (GGT) IN TYPE 2 DIABETES MELLITUS AND ITS RISK FACTORS Shrawan Kumar Meena1, Alka Meena2, Jitendra Ahuja3, Vishnu Dutt Bohra1 1Dept. of Biochemistry, Jhalawar Medical College, And Hospital, Jhalawar (Raj) ijcrr 2Dept. of Biochemistry, Lady Harding medical college and hospital, New Delhi Vol 04 issue 11 3Dept. of Biochemistry, Geetanjali Medical College and Hospital, Udaipur (Raj) Category: Research Received on:18/04/12 Revised on:29/04/12 E-mail of Corresponding Author: [email protected] Accepted on:09/05/12 ABSTRACT Objective — To study the Serum gamma-glutamyltransferase (GGT), other liver derived enzymes and lipid profile in patients of type 2 Diabetes mellitus (DM) and find out the any correlation of liver derived enzymes with diabetic related risk factor and association between enzyme level and blood sugar level in diabetic and non diabetic subjects. Research Design and Methods— This is a cross-sectional prospective study in 60 cases of type 2 DM randomly selected from medical wards of a tertiary care hospital and 30 age, sex matched controls. Blood sugar, Serum gamma-glutamyl transferase (GGT), other liver enzymes like SGOT, SGPT, ALP, Lipid profile, BMI, waist circumference and prevalence of obesity and hypertension were assessed. To define the type 2 Diabetes mellitus (DM) we used revised criteria of ADA, 1997. Results— GGT, Fasting Blood glucose and BMI increased statistically significant (p<0.00l) in type 2 DM subjects when compared with the control subjects. Statistically significant difference (p<0.05) in SGPT was found in subjects of type 2 DM. Comparison of other parameters like BP, alkaline phosphates, PL, TG and VLDL were also found Statistically significant difference (p<0.01). -

Relationship Between Diabetes Mellitus and Serum Uric Acid Levels
Int. J. Pharm. Sci. Rev. Res., 39(1), July – August 2016; Article No. 20, Pages: 101-106 ISSN 0976 – 044X Review Article Relationship between Diabetes Mellitus and Serum Uric Acid Levels J. Sarvesh Kumar*, Vishnu Priya V1, Gayathri R2 *B.D.S I ST YEAR, Saveetha Dental College, 162, P.H road, Chennai, Tamilnadu, India. 1Associate professor, Department of Biochemistry, Saveetha Dental College, 162, P.H Road, Chennai, Tamilnadu, India. 2Assistant professor, Department of Biochemistry, Saveetha Dental College, 162, P.H Road, Chennai, Tamilnadu, India. *Corresponding author’s E-mail: [email protected] Accepted on: 03-05-2016; Finalized on: 30-06-2016. ABSTRACT The aim of the study is to review the association between diabetes Mellitus and serum uric acid levels. The objective is to review how uric acid level is related to diabetes Mellitus. Diabetes is an increasingly important disease globally. New data from IDF showed that there are 336 million people with diabetes in 2011 and this is expected to rise to 552 million by 2030. It has been suggested that, diabetic epidemic will continue even if the level of obesity remains constant. The breakdown of foods high in protein into chemicals known as purines is responsible for the production of uric acid in the body. If there is too much of uric acid in the body it causes variety of side effects. Thus identifying risk factors of serum uric acid is required for the prevention of diabetes. The review was done to relate how serum uric acid level is associated with the risk of diabetes. -
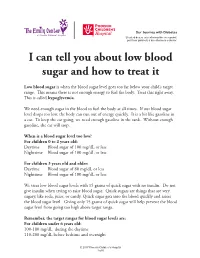
I Can Tell You How the Donor Will Be Determined
Our Journey with Diabetes Si usted desea esta información en español, por favor pídasela a su enfermero o doctor. I can tell you about low blood sugar and how to treat it Low blood sugar is when the blood sugar level goes too far below your child’s target range. This means there is not enough energy to fuel the body. Treat this right away. This is called hypoglycemia. We need enough sugar in the blood to fuel the body at all times. If our blood sugar level drops too low, the body can run out of energy quickly. It is a bit like gasoline in a car. To keep the car going, we need enough gasoline in the tank. Without enough gasoline, the car will stop. When is a blood sugar level too low? For children 0 to 2 years old: Daytime Blood sugar of 100 mg/dL or less Nighttime Blood sugar of 100 mg/dL or less For children 3 years old and older: Daytime Blood sugar of 80 mg/dL or less Nighttime Blood sugar of 100 mg/dL or less We treat low blood sugar levels with 15 grams of quick sugar with no insulin. Do not give insulin when trying to raise blood sugar. Quick sugars are things that are very sugary, like soda, juice, or candy. Quick sugar gets into the blood quickly and raises the blood sugar level. Giving only 15 grams of quick sugar will help prevent the blood sugar level from going too high above target range. Remember, the target ranges for blood sugar levels are: For children under 6 years old: 100-180 mg/dL during the daytime 110-200 mg/dL before bedtime and overnight © 2017 Phoenix Children’s Hospital 1 of 6 For children between 6 and 12 years old: 90-180 mg/dL during the daytime 100-180 mg/dL before bedtime and overnight For teens between 13 and 19 years old: 90-130 mg/dL during the daytime 90-150 mg/dL before bedtime and overnight The levels for blood sugars at night are slightly higher because it can be hard to feel and respond to symptoms of low blood sugar when we are sleeping. -

Low Blood Glucose (Hypoglycemia)
Low Blood Glucose (Hypoglycemia) Hypoglycemia, also known as low blood Hunger, nausea glucose (blood sugar), is when your blood Color draining from skin (pallor) glucose levels have fallen low enough that you need to take action to bring them back Feeling sleepy to your target range. This is usually when your blood glucose is less than 70 mg/dL. However, Feeling weak, having no energy talk to your doctor about your own blood Blurred/impaired vision glucose targets, and what level is too low for you. Tingling or numbness in lips, tongue, cheeks Headaches When can it happen? Coordination problems, clumsiness Low blood glucose can happen if you’ve skipped a meal or snack, eaten less than usual, or been Nightmares or crying out in sleep more physically active than usual. If you don’t Seizures take steps to bring glucose levels back to normal, you could even pass out. What should you do? What are the symptoms? The 15-15 rule—have 15 grams of carbohydrate to raise your blood glucose and check it after Each person’s reaction to low blood glucose is 15 minutes. If it’s still below 70 mg/dL, have different. It’s important that you learn your own another serving. signs and symptoms when your blood glucose is low. Repeat these steps until your blood glucose is at least 70 mg/dL. Once your blood glucose is back Signs and to normal, eat a meal or snack to make sure it symptoms of doesn’t lower again. low blood glucose include: This may be: Feeling shaky Glucose tablets (see instructions) Being nervous Gel tube (see instructions) or anxious 4 ounces (1/2 cups) of juice or regular soda Sweating, chills, (not diet) clamminess 1 tablespoon of sugar, honey, or corn syrup Mood swings, irritability, impatience 8 ounces of nonfat or 1% milk Confusion Hard candies, jellybeans, or gumdrops—see Fast heartbeat food label for how many to consume Feeling light-headed or dizzy Continued » Visit diabetes.org or call 800-DIABETES (800-342-2383) for more resources from the American Diabetes Association.