DIABETES MELLITUS Connie J
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary of Common Diabetes Terms
Glossary of Common Diabetes Terms A1C: a test that reveals exactly how well your blood sugar (glucose) has been controlled over the previous three months Beta cells: cells found in the pancreas that make insulin Blood glucose: also known as blood sugar, glucose comes from food and is then carried through the blood to deliver energy to cells Blood glucose meter: a small medical device used to check blood glucose levels Blood glucose monitoring: the simple blood test used to check the amount of glucose in the blood; a tiny drop of blood, taken by pricking a finger, is placed on a test strip and inserted in the meter for reading Diabetes: the shortened name for diabetes mellitus, the condition in which the pancreas doesn’t produce enough insulin or your body is unable to use insulin to move glucose into cells of the body Diabetic retinopathy: the eye disease that occurs in someone with diabetes when the small blood vessels of the retina become swollen and leak liquid into the retina, blurring vision; it can sometimes lead to blindness Gestational diabetes: the diabetes some women develop during pregnancy; it typically subsides after the baby is delivered, but many women who have had gestational diabetes may develop type 2 diabetes later in life Glucagon: the hormone that is injected into a person with diabetes to raise their blood glucose level when it’s very low (hypoglycemia) Glucose: blood sugar that gives energy to cells Hyperglycemia: also known as high blood glucose, this condition occurs when your blood glucose level is too high; -

Country-Specific Glucose Monitor List
Country-Specific Glucose Monitor List Country Name: Middle East and Africa (Bahrain, Iran, Iraq, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia (KSA), Sudan, U.A.E.) Important Information This is a non-comprehensive list, current as of November 2016. Absence of a specific glucose monitor or test strips from this list does NOT imply compatibility or incompatibility with EXTRANEAL (Icodextrin) PD solution. Similarly, other glucose-measuring technologies which are not listed below (such as continuous glucose monitoring systems) may or may not be compatible with EXTRANEAL. Always contact the device manufacturer for current information. If the manufacturer cannot provide information regarding compatibility of the device with icodextrin and maltose, Baxter does NOT recommend that EXTRANEAL patients use the product. Baxter reserves the right to change this list without notice and does not represent that it includes all potentially incompatible products. The glucose monitor manufacturers listed have certified to Baxter that they have tested (as per ISO 15197) their monitors with maltose and icodextrin to Baxter’s recommended limits: 278 mg/dL (maltose) and 1094 mg/dL (icodextrin). The manufacturers certified that their “green” monitors, below, showed no interference of blood glucose readings under these conditions, with the exception of the “green” monitors specifically notated 4 for which certification of testing to Baxter’s recommended limits has not yet been received. Please note that the compatibility list below is only for brand-name monitors used with the corresponding brand-name test strip. If a brand-name monitor is used with another manufacture’s test strip, always contact the test strip manufacturer for current information. -

Blood Glucose Meters
BLOOD GLUCOSE METERS BLOOD DROP SIZE Meters specify how much blood, in microliters, is needed to get an accurate reading. Some meters allow you to reapply blood within a few seconds if your sample size was too small, so you don’t waste a strip. 1.5 1.0 0.8 0.7 FREESTYLE PRECISION NEO Blood Drop Size Blood Drop 0.6 0.5 0.4 0.3 FEATURES: BLOOD SAMPLE SIZE*: 0.6 BATTERY: 2 CR2032 KEY MSRP: $24.99 = audio capability = port light STRIP MSRP: 44¢/strip = backlight = logs insulin dose ($21.99/50 strips) BP = measures both blood + = calculates insulin dose glucose and blood = meter program offers Strips are compatible with the pressure access to certified meter built into the FreeStyle = wireless Bluetooth diabetes educators Libre reader capability = app compatible ADVOCATE = requires user coding * = microliters C advocatemeters.com = can save data to the ** = sold only with 888-469-3579 cloud without having insulin pump to push the data to MSRP = manufacturer’s suggested ADVOCATE REDI-CODE another device retail price. These are PLUS SPEAKING METER = computer download over-the-counter retail FEATURES: capability prices; check with your BLOOD SAMPLE SIZE*: 1.0 K = also tests blood ketones insurance plan for specific BATTERY: 2 AAA P = communicates with coverage and out-of- MSRP: $29.99 insulin pump pocket costs. STRIPS MSRP: 50¢/strip ($24.99/50 strips) ABBOTT DIABETES CARE AGAMATRIX myfreestyle.com agamatrix.com 888-522-5226 866-906-4197 FREESTYLE FREEDOM LITE JAZZ WIRELESS 2 FEATURES: FEATURES: BLOOD SAMPLE SIZE*: 0.3 BLOOD SAMPLE SIZE*: 0.5 -

Checking Blood Sugar Levels
Checking Blood Sugar Levels People with type 1 diabetes (T1D) must check their blood sugar (glucose) levels throughout the day using a blood glucose meter. The meter tells them how much glucose is in their blood at that particular moment. Based upon the reading, they take insulin, eat, or modify activity to keep blood sugars within their target range. Regularly checking blood sugar levels is an essential part of T1D care. Methods for Checking Blood Sugar Levels Checking, or testing, involves taking a drop of blood, usually from the fingertip, and placing it on a special test strip in a glucose meter. Blood sugar meters are easy to use, and even young children often learn quickly how to do their own blood sugar checks. In order to properly manage their diabetes, individuals with T1D check their blood sugar levels several times per day. For example, they may test before eating lunch and before strenuous exercise. Blood sugar levels are measured in milligrams per deciliter (mg/dL). A normal blood sugar level is between 70 and 120 mg/dL. Keeping blood sugar levels within this range may be difficult in children with diabetes. Therefore, an individual's doctor may adjust the target range (for example, 80-180 mg/dL). However, people with diabetes can't always maintain blood sugar levels within the target range, no matter how hard they try. A person's varying schedules and eating habits, as well as the physical changes that occur as they grow, can send blood sugar levels out of range for no apparent reason. -

Patient Satisfaction and Clinical Efficacy of Novel Blood Glucose Meters Featuring Color Range Indicators in Patients with Type 2 Diabetes: a Prospective Study
Open Access Original Article DOI: 10.7759/cureus.11195 Patient Satisfaction and Clinical Efficacy of Novel Blood Glucose Meters Featuring Color Range Indicators in Patients With Type 2 Diabetes: A Prospective Study Ayman Al Hayek 1 , Asirvatham Alwin Robert 1 , Mohamed Al Dawish 1 1. Department of Endocrinology and Diabetes, Prince Sultan Military Medical City, Riyadh, SAU Corresponding author: Ayman Al Hayek, [email protected] Abstract Introduction Self-monitoring of blood glucose (SMBG) plays an important role in diabetes management. The Contour®Next One glucometer is a recent glucometer that delivers blood glucose results by an immediate color indicator to aware users when blood glucose is at a critical high or low. The main purpose of the study was to assess the impact of an application of a blood glucose meter (BGM) having a color range indicator on clinical characteristics and glucose monitoring satisfaction (GMS) among patients having type 2 diabetes (T2D). Methods A total of 85 (male 42 and female 43) patients with T2D were switched to a BGM having smartLIGHT™ target range indicator (blood glucose meters featuring color range indicator) using Contour®Next One glucometer. Demographic data, as well as glycemic control, were collected at baseline and 12 weeks. At the time of the baseline and 12 weeks of the study, a trained interviewer gave the GMS survey questionnaire to every patient in order to collect the glucose monitoring satisfaction. In addition to GMS, a patient’s perceptions of smartLIGHT™ feature satisfaction survey responses were also collected from the patients at the end of the study (12 weeks). -

Hba1c Matters
HbA1c Matters What is HbA1c? The HbA1c reading reveals your average blood sugar level over the past three months. When blood sugar levels are high, sugar attaches to the red blood cells. The HbA1c monitors how much sugar is attached to the red blood cells, which have a lifespan of about 3 months. The HbA1c reading is therefore able to show what your average blood sugar levels have been in the last 3 months. The units we report HbA1c in are changing, and in the future you will see it reported as a whole number rather than a percentage. Both units are given below. Why does it matter? HbA1c levels are linked with risk of diabetes complications, with higher readings increasing the chance of problems. This is illustrated in the graph below. 15 13 Retinopathy 11 Nephropathy Relative 9 Risk 7 Neuropathy 5 Microalbuminuria 3 1 6 7 8 9 10 11 12 Previous method % 42 53 64 75 86 97 108 New IFCC method HbA1c The graph shows the risk of complications associated with diabetes including retinopathy (eye damage that can lead to blindness), nephropathy (kidney damage that can lead to kidney failure and a need for dialysis), neuropathy (damage to the nerves) and microalbuminuria (protein in the urine which is associated with kidney damage). When HbA1c levels are below 7.5% or 58 mmol/mol, the risk of each of these complications is very low – approximately equivalent to people who do not have diabetes. The risk of each complication rises increasingly steeply as HbA1c levels rise above 7.5% or 58 mmol/mol. -

Country-Specific Glucose Monitor List Kazahhstan 2017
Список мониторов глюкозы для страны Страна : Казахстан (Kazakhstan) Важная информация Это неполный список , действующий по состоянию на 20 декабря 2017 года . Отсутствие определенного монитора глюкозы или тест -полосок в этом списке НЕ указывает совместимость или несовместимость ПД - раствором препарата EXTRANEAL ( Икодекстрин ). Аналогично , другие технологии измерения глюкозы , которые не перечислены ниже ( например , системы для непрерывного мониторинга глюкозы ), могут или не могут быть совместимы с препаратом EXTRANEAL. Всегда обращайтесь к производителю устройства за актуальной информацией . Если производитель не может предоставить информацию о совместимости устройства с икодекстрином и мальтозой , компания Baxter НЕ рекомендует пациентам , принимающим EXTRANEAL, использовать этот продукт . Baxter оставляет за собой право изменять этот список без предварительных уведомлений и не гарантирует включение в него всех потенциально несовместимых продуктов . Перечисленные производители мониторов глюкозы сертифицированы , то есть компания «Baxter» проверила (согласно ISO 15197) работу их мониторов в присутствии мальтозы и икодекстрина в пределах рекомендованных компанией «Baxter» концентраций : 278 мг / дл (мальтоза ) и 1094 мг / дл (икодекстрин ). Подтверждено , что при таких условиях перечисленные ниже « зеленые » мониторы этих производителей не мешают определению уровня глюкозы в крови , за исключением « зеленых » мониторов , обозначенных специальным значком 4, которые еще не еще проверены на соответствие рекомендованным лимитам компании -

Deducing Serum Fructosamine Levels from the Fasting Blood Glucose Value: a Preliminary Study H
http://doi.org/10.4038/cjms.v44i2.4863 Deducing serum fructosamine levels from the fasting blood glucose value: a preliminary study H. Perns' The Ceylon Journal of Medical Science 2001; 44:25-28 Abstract However, recent studies have shown that fructosamine (glycated protein) can be used to The determination of glycated serum proteins differentiate between well and poorly stabilized (fructosamine) has become an accepted index for diabetics (1). Fructosamines are stable keto- assessing the metabolic situation in diabetic amines formed by a non-enzymatic reaction patients. The current study describes an alternative between a sugar and a protein. It has been known to measurement of fructosamine level, viz., to that a number of proteins, e.g., haemoglobin, predict the serum fructosamine based on the serum proteins, membrane proteins, protein in glucose concentration in fasting plasma. A cross- the lens of eye etc. are glycated by a non- sectional prospective study was performed on 44 enzymatic reaction and forms a stable fructo non-diabetic, 38 impaired glucose tolerance and samine (isoglucosamine) which depends on the 38 diabetic subjects attending clinics at Colombo glucose concentration. The glycated serum South Teaching Hospital. Fasting plasma glucose proteins form very quickly with changes in the and corresponding serum fructosamine glucose concentration than the glycated concentrations were determined on all subjects. haemoglobin (HbA ) formed in the erythrocytes. Fructosamine showed a positive linear correlation ]c The largest fraction, about 60-70% of glycated of r2 = 0.85 with the fasting plasma glucose serum proteins, consists of albumin with a half- concentrations. Regression equation relating to life in serum about 2-3 weeks (2). -

Liquid QC™ Bilirubin Control
Hemoglobin A1C Reagent ® INTENDED USE FOR IN VITRO DIAGNOSTIC USE No special additives or preservatives other than anticoagulants are required. Collect Hemoglobin A1c (HbA1c) Reagent is intended for the quantitative determination of venous blood with EDTA using aseptic technique. Hemoglobin A1c in human blood. INTERFERING SUBSTANCES SUMMARY Bilrubin to 50 mg/dl, ascorbic acid to 50 mg/dl, triglycerides to 2000 mg/dl, The determination of HbA1c is most commonly performed for the evaluation of carbamylated Hb to 7.5 mmol/L and acetylated Hb to 5.0 mmol/L do not interfere with glycemic control in diabetes mellitus. HbA1c values provide an indication of glucose this assay. See also the LIMITATION SECTION. levels over the preceding 4-8 weeks. A higher HbA1c value indicates poorer glycemic control. PROCEDURE Throughout the circulatory life of the red cell, HbA1c is formed continuously by the Materials provided adduction of glucose to the N-terminal of the hemoglobin beta chain. This process, 85621 R1 1 x 30 mL which is non-enzymatic, reflects the average exposure of hemoglobin to glucose over R2A 1 x 9.5 mL an extended period. In a classical study, Trivelli, et al, (10.1) showed HbA1c in diabetic subjects to be elevated 2-3 fold over the levels found in normal individuals. R2B 1 x 0.5 mL Several investigators have recommended HbA1c serve as an indicator of metabolic R3 1 x 200 mL control of the diabetic, since HbA1c levels approach normal levels for diabetics in metabolic control. (10.2,10.3,10.4) HBA1c has been defined operationally as the “fast Materials required but not provided fraction” hemoglobins (HbA , A , A ) that elute first during column chromatography 1a 1b 1c 1. -

89 Abstract a Study of Gamma
89 A STUDY OF GAMMA-GLUTAMYLTRANSFERASE (GGT) IN TYPE 2 DIABETES MELLITUS AND ITS RISK FACTORS Shrawan Kumar Meena1, Alka Meena2, Jitendra Ahuja3, Vishnu Dutt Bohra1 1Dept. of Biochemistry, Jhalawar Medical College, And Hospital, Jhalawar (Raj) ijcrr 2Dept. of Biochemistry, Lady Harding medical college and hospital, New Delhi Vol 04 issue 11 3Dept. of Biochemistry, Geetanjali Medical College and Hospital, Udaipur (Raj) Category: Research Received on:18/04/12 Revised on:29/04/12 E-mail of Corresponding Author: [email protected] Accepted on:09/05/12 ABSTRACT Objective — To study the Serum gamma-glutamyltransferase (GGT), other liver derived enzymes and lipid profile in patients of type 2 Diabetes mellitus (DM) and find out the any correlation of liver derived enzymes with diabetic related risk factor and association between enzyme level and blood sugar level in diabetic and non diabetic subjects. Research Design and Methods— This is a cross-sectional prospective study in 60 cases of type 2 DM randomly selected from medical wards of a tertiary care hospital and 30 age, sex matched controls. Blood sugar, Serum gamma-glutamyl transferase (GGT), other liver enzymes like SGOT, SGPT, ALP, Lipid profile, BMI, waist circumference and prevalence of obesity and hypertension were assessed. To define the type 2 Diabetes mellitus (DM) we used revised criteria of ADA, 1997. Results— GGT, Fasting Blood glucose and BMI increased statistically significant (p<0.00l) in type 2 DM subjects when compared with the control subjects. Statistically significant difference (p<0.05) in SGPT was found in subjects of type 2 DM. Comparison of other parameters like BP, alkaline phosphates, PL, TG and VLDL were also found Statistically significant difference (p<0.01). -

Relationship Between Diabetes Mellitus and Serum Uric Acid Levels
Int. J. Pharm. Sci. Rev. Res., 39(1), July – August 2016; Article No. 20, Pages: 101-106 ISSN 0976 – 044X Review Article Relationship between Diabetes Mellitus and Serum Uric Acid Levels J. Sarvesh Kumar*, Vishnu Priya V1, Gayathri R2 *B.D.S I ST YEAR, Saveetha Dental College, 162, P.H road, Chennai, Tamilnadu, India. 1Associate professor, Department of Biochemistry, Saveetha Dental College, 162, P.H Road, Chennai, Tamilnadu, India. 2Assistant professor, Department of Biochemistry, Saveetha Dental College, 162, P.H Road, Chennai, Tamilnadu, India. *Corresponding author’s E-mail: [email protected] Accepted on: 03-05-2016; Finalized on: 30-06-2016. ABSTRACT The aim of the study is to review the association between diabetes Mellitus and serum uric acid levels. The objective is to review how uric acid level is related to diabetes Mellitus. Diabetes is an increasingly important disease globally. New data from IDF showed that there are 336 million people with diabetes in 2011 and this is expected to rise to 552 million by 2030. It has been suggested that, diabetic epidemic will continue even if the level of obesity remains constant. The breakdown of foods high in protein into chemicals known as purines is responsible for the production of uric acid in the body. If there is too much of uric acid in the body it causes variety of side effects. Thus identifying risk factors of serum uric acid is required for the prevention of diabetes. The review was done to relate how serum uric acid level is associated with the risk of diabetes. -
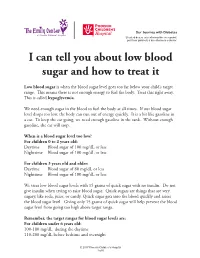
I Can Tell You How the Donor Will Be Determined
Our Journey with Diabetes Si usted desea esta información en español, por favor pídasela a su enfermero o doctor. I can tell you about low blood sugar and how to treat it Low blood sugar is when the blood sugar level goes too far below your child’s target range. This means there is not enough energy to fuel the body. Treat this right away. This is called hypoglycemia. We need enough sugar in the blood to fuel the body at all times. If our blood sugar level drops too low, the body can run out of energy quickly. It is a bit like gasoline in a car. To keep the car going, we need enough gasoline in the tank. Without enough gasoline, the car will stop. When is a blood sugar level too low? For children 0 to 2 years old: Daytime Blood sugar of 100 mg/dL or less Nighttime Blood sugar of 100 mg/dL or less For children 3 years old and older: Daytime Blood sugar of 80 mg/dL or less Nighttime Blood sugar of 100 mg/dL or less We treat low blood sugar levels with 15 grams of quick sugar with no insulin. Do not give insulin when trying to raise blood sugar. Quick sugars are things that are very sugary, like soda, juice, or candy. Quick sugar gets into the blood quickly and raises the blood sugar level. Giving only 15 grams of quick sugar will help prevent the blood sugar level from going too high above target range. Remember, the target ranges for blood sugar levels are: For children under 6 years old: 100-180 mg/dL during the daytime 110-200 mg/dL before bedtime and overnight © 2017 Phoenix Children’s Hospital 1 of 6 For children between 6 and 12 years old: 90-180 mg/dL during the daytime 100-180 mg/dL before bedtime and overnight For teens between 13 and 19 years old: 90-130 mg/dL during the daytime 90-150 mg/dL before bedtime and overnight The levels for blood sugars at night are slightly higher because it can be hard to feel and respond to symptoms of low blood sugar when we are sleeping.