Active Video Gaming Compared to Unstructured, Outdoor Play In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

University of Bath Research Portal
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Bath Research Portal Citation for published version: Mackintosh, KA, Standage, M, Staiano, AE, Lester, L & McNarry, MA 2016, 'Investigating the Physiological and Psychosocial Responses of Single- and Dual-Player Exergaming in Young Adults', Games for Health Journal, vol. 5, no. 6, pp. 375-381. https://doi.org/10.1089/g4h.2016.0015 DOI: 10.1089/g4h.2016.0015 Publication date: 2016 Document Version Peer reviewed version Link to publication Final publication is available from Mary Ann Liebert, Inc., publishers http://dx.doi.org/10.1089/g4h.2016.0015 Copyright©2016 Mary Ann Liebert, Inc. publishers. University of Bath General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 13. May. 2019 1 Running Title: Single- and Dual-player exergaming in adults 2 3 4 5 Investigating the Physiological and Psychosocial Responses of Single- and Dual-Player 6 Exergaming in Young Adults 7 8 Kelly Mackintosh,1 Martyn Standage,2 Amanda E. Staiano,3 Leanne Lester,4 Melitta McNarry1 9 1 College of Engineering, Swansea University, Wales, UK, 2 Department for Health, University of 10 Bath, England, UK, 3 Pennington Biomedical Research Center, 4 School of Sport Science, Exercise 11 and Health, University of Western Australia 12 13 Corresponding Author: Kelly Mackintosh 14 15 1 Abstract 2 Objective: 3 This study investigated the effect of acute exergaming on the physiological and psychosocial responses 4 of young adults and the modulatory effect of a single- or dual-player game play situation. -

Assessment of Enjoyment and Intensity of Physical Activity In
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 12 August 2019 doi:10.20944/preprints201908.0146.v1 Peer-reviewed version available at Int. J. Environ. Res. Public Health 2019, 16, 3673; doi:10.3390/ijerph16193673 1 Article 2 Assessment of enjoyment and intensity of physical 3 activity in immersive virtual reality on the 4 omni-directional Omni treadmill and Icaros flight 5 simulator in the context of recommendations for 6 health 7 Małgorzata Dębska1, Jacek Polechoński1,*, Arkadiusz Mynarski1, Piotr Polechoński2 8 1 Institute of Sport Sciences, The Jerzy Kukuczka Academy of Physical Education in Katowice, 43-512 9 Katowice, Poland; [email protected] (M.D.), [email protected] (J.P.), 10 [email protected] (A.M.) 11 2 Faculty of Physiotherapy, The Jerzy Kukuczka Academy of Physical Education in Katowice, 43-512 12 Katowice, Poland; [email protected] (P.P.) 13 * Correspondence: [email protected]; Tel.: +48-32-207-5358 14 15 Abstract: The aim of the study is to assess enjoyment and intensity of physical exercise while 16 practicing physical activity (PA) in immersive virtual reality (IVR) using innovative training 17 devices (omni-directional Omni treadmill and Icaros Pro flight simulator). The study also contains 18 the results of subjective research on the usefulness of such a form of PA in the opinion of users. In 19 total, 61 adults (10 women and 50 men) took part in the study. To assess the enjoyment level (EL) 20 Interest/Enjoyment subscale of Intrinsic Motivation Inventory (IMI) was used. Exercise intensity 21 was assessed during 10-minute sessions of active video games (AVGs) in IVR based on heart rate 22 (HR). -

Impact of Nintendo Wii Games on Physical Literacy in Children: Motor Skills, Physical Fitness, Activity Behaviors, and Knowledge
sports Article Impact of Nintendo Wii Games on Physical Literacy in Children: Motor Skills, Physical Fitness, Activity Behaviors, and Knowledge Amanda M. George, Linda E. Rohr *,† and Jeannette Byrne † Received: 5 November 2015; Accepted: 11 January 2016; Published: 15 January 2016 Academic Editor: Eling de Bruin School of Human Kinetics and Recreation, Memorial University, St. John’s, NL A1C 5S7, Canada; [email protected] (A.M.G.); [email protected] (J.B.) * Correspondence: [email protected]; Tel.: +1-709-864-6202; Fax: +1-709-864-7531 † These authors contributed equally to this work. Abstract: Physical literacy is the degree of fitness, behaviors, knowledge, and fundamental movement skills (agility, balance, and coordination) a child has to confidently participate in physical activity. Active video games (AVG), like the Nintendo Wii, have emerged as alternatives to traditional physical activity by providing a non-threatening environment to develop physical literacy. This study examined the impact of AVGs on children’s (age 6–12, N = 15) physical literacy. For six weeks children played one of four pre-selected AVGs (minimum 20 min, twice per week). Pre and post measures of motivation, enjoyment, and physical literacy were completed. Results indicated a near significant improvement in aiming and catching (p = 0.06). Manual dexterity significantly improved in males (p = 0.001), and females felt significantly less pressured to engage in PA (p = 0.008). Overall, there appears to be some positive impact of an AVG intervention on components of physical literacy. Keywords: physical literacy; children; active video games; motivation 1. Introduction Physical literacy is an important factor in child development. -

Games for Rehabilitation Sheryl Flynn PT, Phd Belinda Lange Physio, Phd Tuesday, June 29 from 3:00-4:15Pm
Games for Rehabilitation Sheryl Flynn PT, PhD Belinda Lange Physio, PhD Tuesday, June 29 from 3:00-4:15pm. Sheryl Flynn is a consultant and researcher in the VRPSYCH Lab at the Institute for Creative Technologies, University of Southern California and she is the founder and CEO of Blue Marble Game Company, Altadena, CA. ([email protected]) Belinda Lange Bsc., Ph.D is a senior research associate in the VRPSYCH Lab at the Institute for Creative Technologies. Institute for Creative Technologies, University of Southern California, 13274 Fiji Way, Marina Del Rey, CA 90292 ([email protected]). Using video games for rehabilitation purposes combines innovative computer technology with contemporary rehabilitation and neuroplasticity theories. With technological advances video games can now be played with little active movement and minimal fine motor control. These games are motivating and fun while simultaneously pushing the brain and body to recover. The purpose of this presentation is to provide the audience with 1) provide a review of relevant literature in support of video games for rehabilitation, 2) discuss current off the shelf video games and controllers appropriate for rehabilitation, and 3) provide explicit examples of use of games in the clinic. I. Review of relevant literature in support of video games for rehabilitation 1. Video Games for Rehabilitation Reviews a. Weiss P, et al. JNER. 2004;1(1):12. b. Sveistrup H. JNER. 2004;1:10-18. c. Deutsch & Mirelman Topics in Stroke Rehab 2007 d. Henderson et al Topics in Stroke Rehab 2007 e. Adamovich et al, Neurorehabilitation 2009 f. Special Issue of Physical Therapy Reviews (PTR) October 2009 2. -

Enjoyment and Intensity of Physical Activity in Immersive Virtual Reality Performed on Innovative Training Devices in Compliance with Recommendations for Health
International Journal of Environmental Research and Public Health Article Enjoyment and Intensity of Physical Activity in Immersive Virtual Reality Performed on Innovative Training Devices in Compliance with Recommendations for Health Małgorzata D˛ebska 1, Jacek Polecho ´nski 1,* , Arkadiusz Mynarski 1 and Piotr Polecho ´nski 2 1 Institute of Sport Sciences, The Jerzy Kukuczka Academy of Physical Education in Katowice, 43-512 Katowice, Poland; [email protected] (M.D.); [email protected] (A.M.) 2 Faculty of Physiotherapy, The Jerzy Kukuczka Academy of Physical Education in Katowice, 43-512 Katowice, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-32-207-5358 Received: 8 August 2019; Accepted: 27 September 2019; Published: 30 September 2019 Abstract: The aim of the study is to assess the enjoyment and intensity of physical exercise while practicing physical activity (PA) in immersive virtual reality (IVR) using innovative training devices (omni-directional Omni treadmill and Icaros Pro flight simulator). The study also contains the results of subjective research on the usefulness of such a form of PA in the opinion of users. In total, 61 adults (10 women and 51 men) took part in the study. To assess the enjoyment level (EL) Interest/Enjoyment subscale of Intrinsic Motivation Inventory (IMI) was used. Exercise intensity was assessed during 10-min sessions of active video games (AVGs) in IVR based on heart rate (HR). The average enjoyment level during physical exercise in IVR on the tested training devices was high (Omni 5.74 points, Icaros 5.60 points on a 1–7 Likert scale) and differed significantly in favor of PA on Omni. -

Exergames Experience in Physical Education: a Review
PHYSICAL CULTURE AND SPORT. STUDIES AND RESEARCH DOI: 10.2478/pcssr-2018-0010 Exergames Experience in Physical Education: A Review Authors’ contribution: Cesar Augusto Otero Vaghetti1A-E, Renato Sobral A) conception and design 2A-E 1A-E of the study Monteiro-Junior , Mateus David Finco , Eliseo B) acquisition of data Reategui3A-E, Silvia Silva da Costa Botelho 4A-E C) analysis and interpretation of data D) manuscript preparation 1Federal University of Pelotas, Brazil E) obtaining funding 2State University of Montes Carlos, Brazil 3Federal University of Rio Grande do Sul, Brazil 4Federal University of Rio Grande, USA ABSTRACT Exergames are consoles that require a higher physical effort to play when compared to traditional video games. Active video games, active gaming, interactive games, movement-controlled video games, exertion games, and exergaming are terms used to define the kinds of video games in which the exertion interface enables a new experience. Exergames have added a component of physical activity to the otherwise motionless video game environment and have the potential to contribute to physical education classes by supplementing the current activity options and increasing student enjoyment. The use of exergames in schools has already shown positive results in the past through their potential to fight obesity. As for the pedagogical aspects of exergames, they have attracted educators’ attention due to the large number of games and activities that can be incorporated into the curriculum. In this way, the school must consider the development of a new physical education curriculum in which the key to promoting healthy physical activity in children and youth is enjoyment, using video games as a tool. -
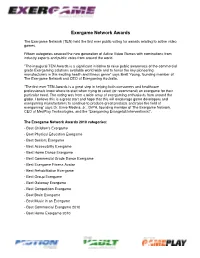
Exergame Network Awards
Exergame Network Awards The Exergame Network (TEN) held the first ever public voting for awards relating to active video games. Fifteen categories covered the new generation of Active Video Games with nominations from industry experts and public votes from around the world. ”The inaugural TEN Awards is a significant initiative to raise public awareness of the commercial grade Exergaming solutions available world wide and to honor the key pioneering manufacturers in this exciting health and fitness genre” says Brett Young, founding member of The Exergame Network and CEO of Exergaming Australia. ”The first ever TEN Awards is a great step in helping both consumers and healthcare professionals know where to start when trying to select (or recommend) an exergame for their particular need. The voting was from a wide array of exergaming enthusiasts from around the globe. I believe this is a great start and hope that this will encourage game developers and exergaming manufacturers to continue to produce great products and raise the field of exergaming” says Dr. Ernie Medina, Jr., DrPH, founding member of The Exergame Network, CEO of MedPlay Technologies, and the “Exergaming Evangelist/Interventionist”. The Exergame Network Awards 2010 categories: - Best Children's Exergame - Best Physical Education Exergame - Best Seniors Exergame - Best Accessibility Exergame - Best Home Dance Exergame - Best Commercial Grade Dance Exergame - Best Exergame Fitness Avatar - Best Rehabilitation Exergame - Best Group Exergame - Best Gateway Exergame - Best Competition Exergame - Best Brain Exergame - Best Music in an Exergame - Best Commercial Exergame 2010 - Best Home Exergame 2010 1. Best Children’s Exergame Award that gets younger kids moving with active video gaming - Dance Dance Revolution Disney Grooves by Konami - Wild Planet Hyper Dash - Atari Family Trainer - Just Dance Kids by Ubisoft - Nickelodeon Fit by 2K Play Dance Dance Revolution Disney Grooves by Konami 2. -

Please Scroll Down for Article
DIGITAL CULTURE & EDUCATION, 3(2) Copyright © 2011, ISSN 1836-8301 Digital Culture & Education (DCE) Publication details, including instructions for authors http://www.digitalcultureandeducation.com/ Active gaming: A new paradigm in childhood physical activity Lisa Witherspoon Hansen Stephen W. Sanders University of South Florida Online Publication Date: 15 December 2011 To cite this Article: Hansen, L. & Sanders, S. W. (2011). Active gaming: A new paradigm in childhood physical activity. Digital Culture & Education, 3:2, 123-139. URL: http://www.digitalcultureandeducation.com/cms/wp-content/uploads/2011/12/dce1040_hansen_2011.pdf PLEASE SCROLL DOWN FOR ARTICLE Active gaming Active gaming: The new paradigm in children’s physical activity Lisa Witherspoon Hansen and Stephen W. Sanders Abstract Childhood obesity is on the rise and children’s participation in physical activity is struggling to maintain the same velocity. Technology often blamed for creating this increase in sedentary lifestyles, however it may also provide the cure. Active gaming is a contemporary approach to exercise that can provide children much needed daily physical activity. The use of active gaming equipment and creation of new facilities for active gaming is increasing throughout the United States. More research is certainly welcome in defining this new movement. However, active gaming appears to be aligned with adolescent culture and makes available a fun alternative to traditional exercise by allowing children to play the digital games they enjoy and also receive the benefits of physical exercise. Benefits as well as concerns and considerations of this movement are discussed in order to clearly appreciate the impact active gaming is currently asserting on daily physical activity patterns of children and adolescents. -

Active Gaming: the Future of Play? S Lisa Witherspoon John P
Active Gaming: The Future of Play? s Lisa Witherspoon John P. Manning The authors examine technology-driven games—especially active gaming—as an evolving form of children’s play. They offer an overview of play and its devel- opmental benefits, describe the literature on the emergence of technology-driven play, and reflect on the diminishment of physical play in contemporary culture. They suggest that active gaming, which they describe in detail, not only meets the research-based definition of play, but also may fill the role of traditional play whose growing absence has left behind a vacuum. Keywords: active gaming; play; physical activity; technology; young children Introduction Today’s children engage infrequently in physical play for a number of reasons. Parents feel uncomfortable allowing their children to play outside after dark—and in some cases during the day—without adult supervision. Play- grounds are not maintained and are often inaccessible. Schools frequently sup- press play by eliminating recess and physical education in favor of more time for academics. In addition, contemporary society’s immersion in technology has become more than an enthralling trend. In today’s high-tech, commercialized world, the outdoor pick-up games once common in neighborhoods have been replaced with digital video games played on computers, iPods, and cell phones. Why this lack of physical play is significant lies in the very nature of play. Children engage in play because it is natural and they find joy in the expe- rience. Children all over the world play regardless of the culture in which they reside. Children engage in play whenever the opportunity exists (Rogers and Sawyers 1988). -
Time Spent in MVPA During Exergaming with Xbox Kinect in Sedentary College Students
Original Research Time Spent in MVPA during Exergaming with Xbox Kinect in Sedentary College Students CHIE YANG*1, ZACHARY WICKERT*1, SAMANTHA ROEDEL*1, ALEXANDRIA BERG*1, ALEX ROTHBAUER*1, MARQUELL JOHNSONǂ1 and DON BREDLEǂ1 1University of Wisconsin-Eau Claire *Denotes undergraduate student author, ‡Denotes professional author ABSTRACT International Journal of Exercise Science 7(4) : 286-294, 2014. The primary purpose of this study was to determine the amount of time spent in moderate-to-vigorous physical activity (MVPA) during a 30-minute bout of exergaming with the Xbox Kinect game console in sedentary college-aged students. A secondary purpose was to examine enjoyment level of participation in the selected exergame. Twenty college-aged students (14 females and 6 males) who self-reported being physically inactive and having no prior experience with the Xbox Kinect game “Your Shape Fitness Evolved 2012” Break a Sweat activity participated in the study. Participants came into the lab on two separate occasions. The first visit involved baseline testing and an 11 minute familiarization session with the game and physical activity (PA) assessment equipment. On the second visit, participants wore the same equipment and completed two 15 minute sessions of the full game. After the first 15 minute session, participants rested for 5 minutes before beginning the next 15 minute session. A 5 minute warm-up and cool-down was completed before and after the testing sessions on a treadmill. Time spent in MVPA was determined via portable indirect calirometry and accelerometry worn at the wrist and waist. 30 minutes, 29.95±.22, and 27.90±1.37 minutes of the 30 minutes of exergaming were spent in MVPA according to activity monitors and indirect calirometry, respectively. -
Games for Health for Children—Current Status and Needed Research
GAMES FOR HEALTH JOURNAL: Research, Development, and Clinical Applications Volume 4, Number 6, 2015 White Paper ª Mary Ann Liebert, Inc. DOI: 10.1089/g4h.2015.0026 Games for Health for Children—Current Status and Needed Research Institute of Digital Media and Child Development Working Group on Games for Health: Tom Baranowski, PhD,1,*,{ Fran Blumberg, PhD,2 Richard Buday, FAIA,3 Ann DeSmet, PhD,4 Lynn E. Fiellin, MD,5 C. Shawn Green, PhD,6 Pamela M. Kato, PhD,7 Amy Shirong Lu, PhD,8 Ann E. Maloney, MD,9 Robin Mellecker, PhD,10 Brooke A. Morrill, PhD,11 Wei Peng, PhD,12 Ross Shegog, PhD,13 Monique Simons, MSc,14 Amanda E. Staiano, PhD,15 Debbe Thompson, PhD,1 and Kimberly Young, PhD16 Abstract Videogames for health (G4H) offer exciting, innovative, potentially highly effective methods for increasing knowledge, delivering persuasive messages, changing behaviors, and influencing health outcomes. Although early outcome results are promising, additional research is needed to determine the game design and behavior change procedures that best promote G4H effectiveness and to identify and minimize possible adverse effects. Guidelines for ideal use of different types of G4H by children and adolescents should be elucidated to enhance effectiveness and minimize adverse effects. G4H stakeholders include organizational implementers, policy makers, players and their families, researchers, designers, retailers, and publishers. All stakeholders should be involved in G4H development and have a voice in setting goals to capitalize on their insights to enhance effectiveness and use of the game. In the future, multiple targeted G4H should be available to meet a population’s diverse health needs in developmentally appropriate ways. -

Exergames in Childhood Obesity Treatment: a Systematic Review
International Journal of Environmental Research and Public Health Review Exergames in Childhood Obesity Treatment: A Systematic Review Federica Valeriani 1, Carmela Protano 2 , Daniela Marotta 2, Giorgio Liguori 3, Vincenzo Romano Spica 1 , Giuliana Valerio 3 , Matteo Vitali 2 and Francesca Gallè 3,* 1 Department of Movement, Human, and Health Sciences, University of Rome “Foro Italico”, 00135 Rome, Italy; [email protected] (F.V.); [email protected] (V.R.S.) 2 Department of Public Health and Infectious Diseases, “Sapienza” University of Rome, 00185 Rome, Italy; [email protected] (C.P.); [email protected] (D.M.); [email protected] (M.V.) 3 Department of Movement Sciences and Wellbeing, University of Naples “Parthenope”, 80133 Naples, Italy; [email protected] (G.L.); [email protected] (G.V.) * Correspondence: [email protected] Abstract: In the last decade, active video games (exergames) have been proposed in obesity pre- vention and treatment as a potential tool to increase physical activity. This review was aimed to assess the possible role of exergames in reducing weight-related outcomes among overweight/obese children and/or adolescents. The databases PubMed, Scopus, Web of Science and SPORTDiscus were interrogated to detect controlled studies involving healthy overweight/obese children and adolescents in interventions based exclusively on exergames. Out of a total of 648 articles found, 10 met the inclusion criteria and were included in the review. The included studies differ for duration, setting and type of intervention, frequency of active game sessions, and outcomes considered. Seven out of ten studies reported better outcomes in children/adolescents involved in the interventions, Citation: Valeriani, F.; Protano, C.; with significant differences between groups in four, while three studies found better outcomes in con- Marotta, D.; Liguori, G.; Romano Spica, V.; Valerio, G.; Vitali, M.; Gallè, trol groups.