Anatomy of Immune Responses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
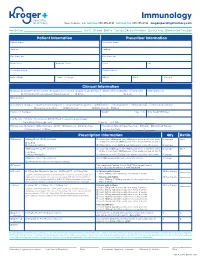
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

CCL19-Igg Prevents Allograft Rejection by Impairment of Immune Cell Trafficking
CCL19-IgG Prevents Allograft Rejection by Impairment of Immune Cell Trafficking Ekkehard Ziegler,* Faikah Gueler,† Song Rong,† Michael Mengel,‡ Oliver Witzke,§ Andreas Kribben,§ Hermann Haller,† Ulrich Kunzendorf,* and Stefan Krautwald* *Department of Nephrology and Hypertension, University of Kiel, Kiel, †Department of Internal Medicine and ‡Institute for Pathology, Hannover Medical School, Hannover, and §Department of Nephrology, School of Medicine, University of Duisburg-Essen, Essen, Germany An adaptive immune response is initiated in the T cell area of secondary lymphoid organs, where antigen-presenting dendritic cells may induce proliferation and differentiation in co-localized T cells after T cell receptor engagement. The chemokines CCL19 and CCL21 and their receptor CCR7 are essential in establishing dendritic cell and T cell recruitment and co- localization within this unique microenvironment. It is shown that systemic application of a fusion protein that consists of CCL19 fused to the Fc part of human IgG1 induces effects similar to the phenotype of CCR7؊/؊ animals, like disturbed accumulation of T cells and dendritic cells in secondary lymphoid organs. CCL19-IgG further inhibited their co-localization, which resulted in a marked inhibition of antigen-specific T cell proliferation. The immunosuppressive potency of CCL19-IgG was tested in vivo using murine models for TH1-mediated immune responses (delayed-type hypersensitivity) and for transplantation of different solid organs. In allogeneic kidney transplantation as well as heterotopic allogeneic heart transplantation in different strain combinations, allograft rejection was reduced and organ survival was significantly prolonged by treatment with CCL19-IgG compared with controls. This shows that in contrast to only limited prolongation of graft survival in CCR7 knockout models, the therapeutic application of a CCR7 ligand in a wild-type environment provides a benefit in terms of immunosuppression. -

Regulate CD4 T Cell Responses Dependent Red Pulp Macrophages − CSF-1
CSF-1−Dependent Red Pulp Macrophages Regulate CD4 T Cell Responses Daisuke Kurotaki, Shigeyuki Kon, Kyeonghwa Bae, Koyu Ito, Yutaka Matsui, Yosuke Nakayama, Masashi Kanayama, This information is current as Chiemi Kimura, Yoshinori Narita, Takashi Nishimura, of September 29, 2021. Kazuya Iwabuchi, Matthias Mack, Nico van Rooijen, Shimon Sakaguchi, Toshimitsu Uede and Junko Morimoto J Immunol published online 14 January 2011 http://www.jimmunol.org/content/early/2011/01/14/jimmun Downloaded from ol.1001345 Supplementary http://www.jimmunol.org/content/suppl/2011/01/14/jimmunol.100134 Material 5.DC1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on September 29, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2011 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published January 14, 2011, doi:10.4049/jimmunol.1001345 The Journal of Immunology CSF-1–Dependent Red Pulp Macrophages Regulate CD4 T Cell Responses Daisuke Kurotaki,*,† Shigeyuki Kon,† Kyeonghwa Bae,† Koyu Ito,† Yutaka Matsui,* Yosuke Nakayama,† Masashi Kanayama,† Chiemi Kimura,† Yoshinori Narita,‡ Takashi Nishimura,‡ Kazuya Iwabuchi,x Matthias Mack,{ Nico van Rooijen,‖ Shimon Sakaguchi,# Toshimitsu Uede,*,† and Junko Morimoto† The balance between immune activation and suppression must be regulated to maintain immune homeostasis. -

Primer the Complement System
View metadata, citation and similar papers at core.ac.uk brought to you by CORE providedMagazine by ElsevierR259 - Publisher Connector vascular permeability and the infection. The second category Primer extravasation of plasma. This is in which there is persistent accompanied by the adhesion of formation of immune complexes is leukocytes to vascular endothelium autoimmune disease, in which, by The complement and their emigration into definition, the antigen is a system surrounding tissue. Complement permanent feature of the host. plays an important part in An understanding of how immune Philip Taylor, Marina inflammation, in helping to recruit complexes cause tissue injury effector cells and in promoting the developed from study of such Botto and Mark Walport killing and clearance of pathogens. diseases in humans and animals, and But complement can be both from the induction of experimental The system of plasma proteins called friend and foe. In some immune complex disease. In these complement was so-named because circumstances the activation of situations, immune complexes were it complements the activity of complement in response to immune shown to cause tissue injury through antibody in the lysis of bacteria. It complexes may cause harm: acutely activation of complement, as opsonin has a central role in host defence in the context of massive (binding to complement receptors on against many micro-organisms and in complement activation occurring in leukocytes) and as the source of the modulation of inflammatory patients with overwhelming Gram- anaphylatoxins (stimulating leukocyte reactions, an activity that has been negative bacterial sepsis, and chemotaxis and degranulation). But illuminated by the study of humans chronically, when an antibody the development of gene-targeted with naturally occurring deficiencies response develops in the context of mice with deficiencies of complement of complement. -

Cells Effects on the Activation and Apoptosis of T Induces Opposing
Fibronectin-Associated Fas Ligand Rapidly Induces Opposing and Time-Dependent Effects on the Activation and Apoptosis of T Cells This information is current as of September 28, 2021. Alexandra Zanin-Zhorov, Rami Hershkoviz, Iris Hecht, Liora Cahalon and Ofer Lider J Immunol 2003; 171:5882-5889; ; doi: 10.4049/jimmunol.171.11.5882 http://www.jimmunol.org/content/171/11/5882 Downloaded from References This article cites 40 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/171/11/5882.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 28, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2003 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Fibronectin-Associated Fas Ligand Rapidly Induces Opposing and Time-Dependent Effects on the Activation and Apoptosis of T Cells1 Alexandra Zanin-Zhorov, Rami Hershkoviz, Iris Hecht, Liora Cahalon, and Ofer Lider2 Recently, it has been shown that Fas ligand (FasL) interacts with the extracellular matrix (ECM) protein fibronectin (FN), and that the bound FasL retains its cytotoxic efficacy. -

We Work at the Intersection of Immunology and Developmental Biology
Development and Homeostasis of Mucosal Tissues U934/UMR3215 – Genetics and Developmental Biology Pedro Hernández Chef d'équipe [email protected] We work at the intersection of immunology and developmental biology. Our primary goal is to understand how immune responses impact the development, integrity and function of mucosal tissue layers, such as the intestinal epithelium, during homeostasis and upon different types of stress, including infections. To study these questions we exploit the advantages of the zebrafish model such as ex utero and rapid development, transparency, large progeny, and simple genetic manipulation. We combine live imaging, flow cytometry, single-cell transcriptomics, and models inducing mucosal stress, including pathogenic challenges. Our research can be subdivided into three main topics: 1) Protection of intestinal epithelial integrity since early development: Epithelial cells are at the core of intestinal organ function. They are in charge of absorbing nutrients and water, and at the same time constitute a barrier for potential pathogens and harmful molecules. Epithelial cells perform all these functions before full development of the immune system, which promotes epithelial barrier function upon injury. We study how robust epithelial integrity is achieved prior and after maturation of the intestinal immune system, with a focus on the function of mucosal cytokines. 2) Epithelial-leukocyte crosstalk throughout development: Intestines become vastly populated by leukocytes after exposure to external cues from diet and colonization by the microbiota. We have recently reported the existence and diversity of zebrafish innate lymphoid cells (ILCs), a key component of the mucosal immune system recently discovered in mice and humans. ILCs mediate immune responses by secreting cytokines such as IL-22 which safeguards gut epithelial integrity. -

Complement Recognition Pathways in Renal Transplantation
BRIEF REVIEW www.jasn.org Complement Recognition Pathways in Renal Transplantation Christopher L. Nauser, Conrad A. Farrar, and Steven H. Sacks Medical Research Council Centre for Transplantation, Division of Transplantation Immunology and Mucosal Biology, King’s College London, National Health Service Guy’s and St. Thomas’ Trust, London, United Kingdom ABSTRACT The complement system, consisting of soluble and cell membrane–bound compo- weigh its effect on organ injury and nents of the innate immune system, has defined roles in the pathophysiology of renal rejection with dampening the antimi- allograft rejection. Notably, the unavoidable ischemia-reperfusion injury inherent to crobial functions of the complement sys- transplantation is mediated through the terminal complement activation products tem, such as opsonisation, cell lysis, and C5a and C5b-9. Furthermore, biologically active fragments C3a and C5a, produced recruitment of neutrophils and other in- during complement activation, can modulate both antigen presentation and T cell flammatory cells.7 It is our belief that priming, ultimately leading to allograft rejection. Earlier work identified renal tubule therapeutic strategies can be designed cell synthesis of C3, rather than hepatic synthesis of C3, as the primary source of C3 to specificallytargetthekeyinitiators driving these effects. Recent efforts have focused on identifying the local triggers of of complement activation at the relevant complement activation. Collectin-11, a soluble C-type lectin expressed in renal tis- location, such as complement-binding sue, has been implicated as an important trigger of complement activation in renal anti-HLA antibodies in the vascular tissue. In particular, collectin-11 has been shown to engage L-fucose at sites of compartment or the initiator(s) of local ischemic stress, activating the lectin complement pathway and directing the innate complement activation in the extravas- immune response to the distressed renal tubule. -
Characterization of Murine Macrophages from Bone Marrow
Wang et al. BMC Immunology 2013, 14:6 http://www.biomedcentral.com/1471-2172/14/6 RESEARCH ARTICLE Open Access Characterization of murine macrophages from bone marrow, spleen and peritoneum Changqi Wang1*†, Xiao Yu1,2†, Qi Cao1, Ya Wang1, Guoping Zheng1, Thian Kui Tan1, Hong Zhao1,3, Ye Zhao1, Yiping Wang1 and David CH Harris1 Abstract Background: Macrophages have heterogeneous phenotypes and complex functions within both innate and adaptive immune responses. To date, most experimental studies have been performed on macrophages derived from bone marrow, spleen and peritoneum. However, differences among macrophages from these particular sources remain unclear. In this study, the features of murine macrophages from bone marrow, spleen and peritoneum were compared. Results: We found that peritoneal macrophages (PMs) appear to be more mature than bone marrow derived macrophages (BMs) and splenic macrophages (SPMs) based on their morphology and surface molecular characteristics. BMs showed the strongest capacity for both proliferation and phagocytosis among the three populations of macrophage. Under resting conditions, SPMs maintained high levels of pro-inflammatory cytokines expression (IL-6, IL-12 and TNF-α), whereas BMs produced high levels of suppressive cytokines (IL-10 and TGF-β). However, SPMs activated with LPS not only maintained higher levels of (IL-6, IL-12 and TNF-α) than BMs or PMs, but also maintained higher levels of IL-10 and TGF-β. Conclusions: Our results show that BMs, SPMs and PMs are distinct populations with different biological functions, providing clues to guide their further experimental or therapeutic use. Keywords: Macrophage, Bone marrow, Spleen, Peritoneum Background macrophage populations could be attributed to their het- Macrophages play an essential role in both innate and erogeneity [4]. -

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

CXCL13/CXCR5 Interaction Facilitates VCAM-1-Dependent Migration in Human Osteosarcoma
International Journal of Molecular Sciences Article CXCL13/CXCR5 Interaction Facilitates VCAM-1-Dependent Migration in Human Osteosarcoma 1, 2,3,4, 5 6 7 Ju-Fang Liu y, Chiang-Wen Lee y, Chih-Yang Lin , Chia-Chia Chao , Tsung-Ming Chang , Chien-Kuo Han 8, Yuan-Li Huang 8, Yi-Chin Fong 9,10,* and Chih-Hsin Tang 8,11,12,* 1 School of Oral Hygiene, College of Oral Medicine, Taipei Medical University, Taipei City 11031, Taiwan; [email protected] 2 Department of Orthopaedic Surgery, Chang Gung Memorial Hospital, Puzi City, Chiayi County 61363, Taiwan; [email protected] 3 Department of Nursing, Division of Basic Medical Sciences, and Chronic Diseases and Health Promotion Research Center, Chang Gung University of Science and Technology, Puzi City, Chiayi County 61363, Taiwan 4 Research Center for Industry of Human Ecology and Research Center for Chinese Herbal Medicine, Chang Gung University of Science and Technology, Guishan Dist., Taoyuan City 33303, Taiwan 5 School of Medicine, China Medical University, Taichung 40402, Taiwan; [email protected] 6 Department of Respiratory Therapy, Fu Jen Catholic University, New Taipei City 24205, Taiwan; [email protected] 7 School of Medicine, Institute of Physiology, National Yang-Ming University, Taipei City 11221, Taiwan; [email protected] 8 Department of Biotechnology, College of Health Science, Asia University, Taichung 40402, Taiwan; [email protected] (C.-K.H.); [email protected] (Y.-L.H.) 9 Department of Sports Medicine, College of Health Care, China Medical University, Taichung 40402, Taiwan 10 Department of Orthopedic Surgery, China Medical University Beigang Hospital, Yunlin 65152, Taiwan 11 Department of Pharmacology, School of Medicine, China Medical University, Taichung 40402, Taiwan 12 Chinese Medicine Research Center, China Medical University, Taichung 40402, Taiwan * Correspondence: [email protected] (Y.-C.F.); [email protected] (C.-H.T.); Tel.: +886-4-2205-2121-7726 (C.-H.T.); Fax: +886-4-2233-3641 (C.-H.T.) These authors contributed equally to this work. -

The Unexpected Role of Lymphotoxin Β Receptor Signaling
Oncogene (2010) 29, 5006–5018 & 2010 Macmillan Publishers Limited All rights reserved 0950-9232/10 www.nature.com/onc REVIEW The unexpected role of lymphotoxin b receptor signaling in carcinogenesis: from lymphoid tissue formation to liver and prostate cancer development MJ Wolf1, GM Seleznik1, N Zeller1,3 and M Heikenwalder1,2 1Department of Pathology, Institute of Neuropathology, University Hospital Zurich, Zurich, Switzerland and 2Institute of Virology, Technische Universita¨tMu¨nchen/Helmholtz Zentrum Mu¨nchen, Munich, Germany The cytokines lymphotoxin (LT) a, b and their receptor genesis. Consequently, the inflammatory microenviron- (LTbR) belong to the tumor necrosis factor (TNF) super- ment was added as the seventh hallmark of cancer family, whose founder—TNFa—was initially discovered (Hanahan and Weinberg, 2000; Colotta et al., 2009). due to its tumor necrotizing activity. LTbR signaling This was ultimately the result of more than 100 years of serves pleiotropic functions including the control of research—indeed—the first observation that tumors lymphoid organ development, support of efficient immune often arise at sites of inflammation was initially reported responses against pathogens due to maintenance of intact in the nineteenth century by Virchow (Balkwill and lymphoid structures, induction of tertiary lymphoid organs, Mantovani, 2001). Today, understanding the underlying liver regeneration or control of lipid homeostasis. Signal- mechanisms of why immune cells can be pro- or anti- ing through LTbR comprises the noncanonical/canonical carcinogenic in different types of tumors and which nuclear factor-jB (NF-jB) pathways thus inducing cellular and molecular inflammatory mediators (for chemokine, cytokine or adhesion molecule expression, cell example, macrophages, lymphocytes, chemokines or proliferation and cell survival.