Fungal Endophthalmitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Congo DRC, Kamwiziku. Mycoses 2021
Received: 8 April 2021 | Revised: 1 June 2021 | Accepted: 10 June 2021 DOI: 10.1111/myc.13339 REVIEW ARTICLE Serious fungal diseases in Democratic Republic of Congo – Incidence and prevalence estimates Guyguy K. Kamwiziku1 | Jean- Claude C. Makangara1 | Emma Orefuwa2 | David W. Denning2,3 1Department of Microbiology, Kinshasa University Hospital, University of Abstract Kinshasa, Kinshasa, Democratic Republic A literature review was conducted to assess the burden of serious fungal infections of Congo 2Global Action Fund for Fungal Infections, in the Democratic Republic of the Congo (DRC) (population 95,326,000). English and Geneva, Switzerland French publications were listed and analysed using PubMed/Medline, Google Scholar 3 Manchester Fungal Infection Group, The and the African Journals database. Publication dates spanning 1943– 2020 were in- University of Manchester, Manchester Academic Health Science Centre, cluded in the scope of the review. From the analysis of published articles, we estimate Manchester, UK a total of about 5,177,000 people (5.4%) suffer from serious fungal infections in the Correspondence DRC annually. The incidence of cryptococcal meningitis, Pneumocystis jirovecii pneu- Guyguy K. Kamwiziku, Department monia in adults and invasive aspergillosis in AIDS patients was estimated at 6168, of Microbiology, Kinshasa University Hospital, University of Kinshasa, Congo. 2800 and 380 cases per year. Oral and oesophageal candidiasis represent 50,470 Email: [email protected] and 28,800 HIV- infected patients respectively. Chronic pulmonary aspergillosis post- tuberculosis incidence and prevalence was estimated to be 54,700. Fungal asthma (allergic bronchopulmonary aspergillosis and severe asthma with fungal sensitiza- tion) probably has a prevalence of 88,800 and 117,200. -

Financial Supporters
FINANCIAL SUPPORTERS Care and Share Food Bank for Southern Colorado 2011-12 Financial Supporters 100% Chiropractic Lanny and Paul Adams Mr. and Mrs. Jeffrey Ahrendsen 14K Real Estate Investments LLC Ms. Laura Adams Mr. Kevin Ahrens 1882 Management Mr. and Mrs. Lon Adams Mr. and Mrs. Charles Aiken 1st Cavalry Rocky Mountain Chapter Col and Mrs. Louis Adams Ms. Laverne Ainley 221 South Oak Bistro Ms. Maggie Adams Air Academy Federal Credit Union 4-Bits 4-H Club Ms. Mary Adams Air Academy Federal Credit Union 4Clicks - Solutions, LLC Mr. Michael Adams Air Academy High School - District 20 A & L Aluminum Manufacturing Company Mr. and Mrs. Rexford Adams Mr. TJ Airhart A Handymike Home Repair Mr. and Mrs. Robert Adams Aka Wilson, LLC A to Z Realty Mr. S. Michael Adams Mr. Richard Alaniz AA “Accurate and Affordable” Striping, Inc. Mr. and Mrs. Samuel Adams Ms. Susan Alarid AAA NCNU Insurance Exchange Mr. Steve Adams Ms. Karin Alaska AAA Northern California Nevada & Utah Suzanne Adams Mr. Arturo Albanesi AARP Foundation Adams Bank & Trust Mr. and Mrs. Mac Alberico Ms. Renee Abbe Mrs. Alda Adcox Ms. Cheryl Alberto Ms. Marjory Abbott Add Staff Inc. Mr. and Mrs. Dewey Albertson Jr. Mr. and Mrs. Peyton Abbott Ms. Constance Addington Mr. W. Gary Albertson Ms. Stephanie Abbott Mr. and Mrs. D. V. Addington Albertsons LLC Ms. Brianna Abby Ms. Linda Addington Mr. and Mrs. Albert Albrandt Mr. and Mrs. Donald Abdallah Ms. Vicky Addison Mr. Gerald Albrecht Mr. Tony Abdella Ms. Deirdre Aden-Smith Ms. Patricia Albright Mr. and Mrs. William Abel Mr. -

70-2294 ALY, Raza, 1935- IMMÜNOLOGICAL RESPONSE OF
This dissertation has been microfilmed exactly as received 70-2294 ALY, Raza, 1935- IMMÜNOLOGICAL RESPONSE OF GUINEA PIGS CHRONICALLY INFECTED WITH REPEATED AND A SINGLE DOSE OF HISTOPLASMA DUBOISII. The University of Oklahoma, Ph.D., 1969 Microbiology University Microfilms, Inc., Ann Arbor, Michigan THE UNIVERSITY OF OKLAHOMA GRADUATE COLLEGE IMMUNOLOGICAL RESPONSE OF GUINEA PIGS CHRONICALLY INFECTED WITH REPEATED AND A SINGLE DOSE OF HISTOPLASMA DUBOISII A DISSERTATION SUBMITTED TO THE GRADUATE FACULTY in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY BY RAZA ALY Norman, Oklahoma 1969 IMMUNOLOGICAL RESPONSE OF GUINEA PIGS CHRONICALLY INFECTED WITH REPEATED AND A SINGLE DOSE OF HISTOPLASMA DUBOISII APPROVED BY DISSERTATION COMMITTEE ACKNOWLEDGEMENT The author wishes to express his sincere thanks to Dr. Howard W. Larsh for his inspiration and continued guidance throughout this study. A special note of thanks to Dr. G. C. Cozad, Dr. J. H, Lancaster I Dr. D. 0. Cox, and Dr. L. S. Ciereszko for their assistance in the writing of this manuscript. Sincere appréciation to Dr. Peter A. Bartels for his assis tance. A special note of appreciation is also extended to Miss Janis Reeser, Miss Mary Jane Hook, and Mr. Don Wiggins for their technical assistance in this study. Also, a special note of appreciation to my wife Naheed for editing and typing the manuscript. Ill TABLE OF CONTENTS Page LIST OF TABLES ............... » . v LIST OF ILLUSTRATIONS . .............. vi Chapter I. INTRODUCTION .......... ............ 1 II. MATERIALS AND METHODS ........... .. 8 III. RESULTS ............. 22 IV. DISCUSSION ........... 42 V. SUMMARY AND CONCLUSIONS........... 48 BIBLIOGRAPHY ............. 5© IV LIST OF TABLES Table Page 1. -

Acute Disseminated Histoplasmosis of Pulmonary Origin Probably Contracted in Britain by A
Thorax: first published as 10.1136/thx.16.4.388 on 1 December 1961. Downloaded from Thorax (1961), 16, 388. ACUTE DISSEMINATED HISTOPLASMOSIS OF PULMONARY ORIGIN PROBABLY CONTRACTED IN BRITAIN BY A. A. MILLER, F. RAMSDEN, AND M. R. GEAKE From the Group Laboratory, Preston Royal Infirmary, and Sharoe Green Hospital, Preston (RECEIVED FOR PUBLICATION NOVEMBER 28, 1960) Histoplasmosis in any form is an unusual made a comprehensive study of the varied radio- finding in Great Britain. The case described in logical appearances in 28 cases of histoplasmosis; this paper is that of a man with bilateral of these cases nine showed pulmonary involve- pulmonary histoplasmosis which terminated with ment. Furcolow (1960) indicates that at least 30% an acute disseminated infection. It is believed to of positive skin test reactors have, or develop, be an example of an indigenous British infection. demonstrable lesions. Symmers (1956) made a critical analysis of the 15 cases of histoplasmosis reported in Great INDIGENOUS INFECTIONS Britain up to 1956 and found two of them The first unequivocal, mycologically proved (Limerick, 1951) unacceptable as there was instance of histoplasmosis in which the infection insufficient evidence to warrant the diagnosis of was contracted in Britain is believed to be that copyright. histoplasmosis. Earle, Highman, and Lockley reported by Symmers (1956) and was a case of (1960) described a fatal case of acute disseminated histoplasmic lymphadenitis. histoplasmosis in a man aged 62 years who had In the case described here the patient had never lived in India for 30 years and contracted the been outside Great Britain except during the disease in that country. -
Monograph on Dimorphic Fungi
Monograph on Dimorphic Fungi A guide for classification, isolation and identification of dimorphic fungi, diseases caused by them, diagnosis and treatment By Mohamed Refai and Heidy Abo El-Yazid Department of Microbiology, Faculty of Veterinary Medicine, Cairo University 2014 1 Preface When I see the analytics made by academia.edu for the visitors to my publication has reached 244 in 46 countries in one month only, this encouraged me to continue writing documents for the benefit of scientists and students in the 5 continents. In the last year I uploaded 3 monographs, namely 1. Monograph on yeasts, Refai, M, Abou-Elyazeed, H. and El-Hariri, M. 2. Monograph on dermatophytes, Refai, M, Abou-Elyazeed, H. and El-Hariri, M. 3. Monograph on mycotoxigenic fungi and mycotoxins, Refai, M. and Hassan, A. Today I am uploading the the 4th documents in the series of monographs Monograph on dimorphic fungi, Refai, M. and Abou-Elyazeed, H. Prof. Dr. Mohamed Refai, 2.3.2014 Country 30 day views Egypt 51 2 Country 30 day views Ethiopia 22 the United States 21 Saudi Arabia 19 Iraq 19 Sudan 14 Uganda 12 India 11 Nigeria 9 Kuwait 8 the Islamic Republic of Iran 7 Brazil 7 Germany 6 Uruguay 4 the United Republic of Tanzania 4 ? 4 Libya 4 Jordan 4 Pakistan 3 the United Kingdom 3 Algeria 3 the United Arab Emirates 3 South Africa 2 Turkey 2 3 Country 30 day views the Philippines 2 the Netherlands 2 Sri Lanka 2 Lebanon 2 Trinidad and Tobago 1 Thailand 1 Sweden 1 Poland 1 Peru 1 Malaysia 1 Myanmar 1 Morocco 1 Lithuania 1 Jamaica 1 Italy 1 Hong Kong 1 Finland 1 China 1 Canada 1 Botswana 1 Belgium 1 Australia 1 Argentina 4 1. -

Septic Arthritis Due to Histoplasma Capsulatum in a Leukaemic Patient
Ann Rheum Dis: first published as 10.1136/ard.44.2.128 on 1 February 1985. Downloaded from Annals of the Rheumatic Diseases, 1985, 44, 128-129 Case report Septic arthritis due to Histoplasma capsulatum in a leukaemic patient PAULA G JONES,' KENNETH ROLSTON,' AND ROY L HOPFER2 From the Section of 'Infectious Diseases, Department of Internal Medicine and 2Department of Laboratory Medicine, the University of Texas M.D. Anderson Hospital and Tumor Institute at Houston, 6723 Bertner Avenue, Houston, Texas 77030, USA SUMMARY A case of septic, histoplasmal monoarthritis of the knee in a leukaemic patient is described. Ketoconazole therapy failed to eliminate the infection, but after histoplasmosis was diagnosed prolonged therapy with amphotericin B was curative. Key words: fungi, histoplasmosis, leukaemia, myeloproliferative disorders, antifungal agents. copyright. A 29-year-old man with acute myelogenous ramycin, and trimethoprim-sulphamethoxazole, the leukaemia refractory to chemotherapy was admitted patient was given amphotericin B empirically, re- to the hospital with fever, diarrhoea, and neut- sulting in prompt defervescence. A total dose of 180 ropenia on 23 September 1983. On physical ex- mg of pamphotericin B was given over five days. amination the patient's temperature was 38-5°C. His Broad-spectrum antibiotics were given for 22 days pulse was 120/min, blood pressure, 150/60 mmHg, because of the possibility of bacterial infection. http://ard.bmj.com/ and respiratory rate 18/min. He had severe mucosi- Chest roentgenograms during this period showed an tis of the oropharynx. There were no other signifi- infiltrate in the lower left lung. The patient was cant physical findings. -
ADAPTATION of FORESTS and PEOPLE to CLIMATE Change – a Global Assessment Report
International Union of Forest Research Organizations Union Internationale des Instituts de Recherches Forestières Internationaler Verband Forstlicher Forschungsanstalten Unión Internacional de Organizaciones de Investigación Forestal IUFRO World Series Vol. 22 ADAPTATION OF FORESTS AND PEOPLE TO CLIMATE CHANGE – A Global Assessment Report Prepared by the Global Forest Expert Panel on Adaptation of Forests to Climate Change Editors: Risto Seppälä, Panel Chair Alexander Buck, GFEP Coordinator Pia Katila, Content Editor This publication has received funding from the Ministry for Foreign Affairs of Finland, the Swedish International Development Cooperation Agency, the United Kingdom´s Department for International Development, the German Federal Ministry for Economic Cooperation and Development, the Swiss Agency for Development and Cooperation, and the United States Forest Service. The views expressed within this publication do not necessarily reflect official policy of the governments represented by these institutions. Publisher: International Union of Forest Research Organizations (IUFRO) Recommended catalogue entry: Risto Seppälä, Alexander Buck and Pia Katila. (eds.). 2009. Adaptation of Forests and People to Climate Change. A Global Assessment Report. IUFRO World Series Volume 22. Helsinki. 224 p. ISBN 978-3-901347-80-1 ISSN 1016-3263 Published by: International Union of Forest Research Organizations (IUFRO) Available from: IUFRO Headquarters Secretariat c/o Mariabrunn (BFW) Hauptstrasse 7 1140 Vienna Austria Tel: + 43-1-8770151 Fax: + 43-1-8770151-50 E-mail: [email protected] Web site: www.iufro.org/ Cover photographs: Matti Nummelin, John Parrotta and Erkki Oksanen Printed in Finland by Esa-Print Oy, Tampere, 2009 Preface his book is the first product of the Collabora- written so that they can be read independently from Ttive Partnership on Forests’ Global Forest Expert each other. -

Diagnosis of Histoplasmosis
Brazilian Journal of Microbiology (2006) 37:1-13 ISSN 1517-8382 DIAGNOSIS OF HISTOPLASMOSIS Allan Jefferson Guimarães1,2; Joshua D. Nosanchuk2; Rosely Maria Zancopé-Oliveira1* 1Serviço de Micologia, Departamento de Micro-Imuno-Parasitologia, Instituto de Pesquisa Evandro Chagas, Fundação Oswaldo Cruz, Rio de Janeiro, Brasil; 2Department of Medicine (Division of Infectious Diseases) & Microbiology and Imunology, Albert Einstein College of Medicine of Yeshiva University, Bronx, New York Submitted: January 31, 2006; Approved: February 13, 2006 ABSTRACT Endemic mycoses can be challenging to diagnose and accurate interpretation of laboratory data is important to ensure the most appropriate treatment for the patients. Although the definitive diagnosis of histoplasmosis (HP), one of the most frequent endemic mycoses in the world, is achieved by direct diagnosis performed by micro and/or macroscopic observation of Histoplasma capsulatum (H. capsulatum), serologic evidence of this fungal infection is important since the isolation of the etiologic agents is time-consuming and insensitive. A variety of immunoassays have been used to detect specific antibodies to H. capsulatum. The most applied technique for antibody detection is immunodiffusion with sensitivity between 70 to 100 % and specificity of 100%, depending on the clinical form. The complement fixation (CF) test, a methodology extensively used on the past, is less specific (60 to 90%). Detecting fungal antigens by immunoassays is valuable in immunocompromised individuals where such assays achieve positive predictive values of 96-98%. Most current tests in diagnostic laboratories still utilize unpurified antigenic complexes from either whole fungal cells or their culture filtrates. Emphasis has shifted, however, to clinical immunoassays using highly purified and well-characterized antigens including recombinant antigens. -
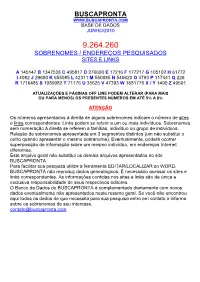
Buscapronta Base De Dados Junho/2010
BUSCAPRONTA WWW.BUSCAPRONTA.COM BASE DE DADOS JUNHO/2010 9.264.260 SOBRENOMES / ENDEREÇOS PESQUISADOS SITES E LINKS A 145147 B 1347538 C 495817 D 276690 E 17216 F 177217 G 105102 H 61772 I 4082 J 29600 K 655085 L 42311 M 550085 N 540620 O 4793 P 117441 Q 226 R 1716485 S 1089982 T 71176 U 35625 V 47393 W 1681776 X / Y 1490 Z 49591 ATUALIZAÇÕES E PÁGINAS OFF LINE PODEM ALTERAR (PARA MAIS OU PARA MENOS) OS PRESENTES NÚMEROS EM ATÉ 5% A 8% ATENÇÃO Os números apresentados à direita de alguns sobrenomes indicam o número de sites e links correspondentes. Links podem se referir a um ou mais indivíduos. Sobrenomes sem numeração à direita se referem a famílias, indivíduo ou grupo de indivíduos. Relação de sobrenomes apresentada em 3 segmentos distintos (um não substitui o outro quando apresentar o mesmo sobrenome). Eventualmente, poderá ocorrer superposição de informação sobre um mesmo indivíduo, em endereços Internet diferentes. Este arquivo geral não substitui os demais arquivos apresentados no site BUSCAPRONTA. Para facilitar sua pesquisa utilize a ferramenta EDITAR/LOCALIZAR so WORD. BUSCAPRONTA não reproduz dados genealógicos. È necessário acessar os sites e links correspondentes. As informações contidas nos sites e links são de única e exclusiva responsabilidade de seus respectivos editores. O Banco de Dados do BUSCAPRONTA é complementado diariamente com novos dados eventualmente não apresentados neste resumo geral. Se você não encontrou aqui todos os dados de que necessita para sua pesquisa entre em contato e informe sobre os sobrenomes -

Luciano Polonelli
Luciano Polonelli Department of Biomedical, Biotechnological and Translational Sciences, Unit of Microbiology and Virology, University of Parma, Parma, Italy Tel.: +39 0521 903429; Fax: +39 0521 993620; e-mail: [email protected] History of Medical Mycology File 2 (1895-1950) 1895 Giuseppe Marconi (1862-1940), born in Naples, Italy, Professor of Veterinary Pathology and Clinic in the Royal University of Pisa, Italy, isolated and cultivated for the first time Cryptococcus farciminosum, the agent of epizootic lymphangitis, in the form of sterile mycelium (1895). Piero Redaelli and Raffaele Ciferri transferred (1934) C. farciminosum to the genus Histoplasma, as H. farciminosum (Rivolta and Micellone 1883, Redaelli and Ciferri 1934), mainly because of its dimorphic nature that made it similar to the tissue form of H. capsulatum var. capsulatum Darling 1906. Robert J. Weeks, Arvind A. Padhye and Libero Ajello, at the Division of Mycotic Diseases, Center for Infectious Diseases, Centers for Disease Control (C.D.C.) Atlanta, Georgia, U.S.A. (1985), observed that this fungus generated macro- and microconidia resembling those of the capsulatum and duboisii varieties of H. capsulatum when incubated at room temperature, thus reducing the fungus to a varietal status as H. capsulatum var. farciminosum (Rivolta, 1873) Weeks, Padhye & Ajello, 1985. Raffaele Ciferri (1960) reduced Histoplasma duboisii (Vanbreuseghem, 1992) to varietal status as H. capsulatum var. duboisii (Vanbreuseghem, 1992), Ciferri, 1960 [Ajello, 1998; Marcone, 1895; Redaelli and Ciferri, 1934; Weeks et al., 1985]. 1 1896 The American surgeon Emmet Rixford (1865-1938), born in Bedford, Canada, first graduated in engineering and then Doctor in Medicine (1891), and Thomas C. -

WO 2013/038197 Al 21 March 2013 (21.03.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2013/038197 Al 21 March 2013 (21.03.2013) P O P C T (51) International Patent Classification: Geir [NO/NO]; Bj0rndalen 81, N-7072 Heimdal (NO). A01N 43/16 (2006.01) A01N 43/653 (2006.01) MYRVOLD, Rolf [NO/NO]; 0vre Gjellum vei 28, N- A61K 31/734 (2006.01) A01P 3/00 (2006.01) 1389 Heggedal (NO). A01N 43/90 (2006.01) (74) Agent: DEHNS; St Bride's House, 10 Salisbury Square, (21) International Application Number: London EC4Y 8JD (GB). PCT/GB20 12/052274 (81) Designated States (unless otherwise indicated, for every (22) International Filing Date kind of national protection available): AE, AG, AL, AM, 14 September 2012 (14.09.2012) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, (25) English Filing Language: DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (26) Publication Language: English HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (30) Priority Data: ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 1116010.8 15 September 201 1 (15.09.201 1) GB NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, (71) Applicant (for all designated States except US): AL- RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, GIPHARMA AS [NO/NO]; Industriveien 33, N-1337 TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, Sandvika (NO). -

Astronautics and Aeronautics, 1966
NASA SP-4007 ASTRONAUTICS AND AERONAUTICS, 1966 Chronology on Science, Technology, and Policy Text by Science and Technology Division Library of Congress Sponsored by NASA Historical Staff Office of Policy Screntrfic and Technrcal Information Divisron 1967 NATIONAL AERONAUTICS AND SPACE ADMINISTRATION WaJhington, D.C. For Sale by the Superintendent of Documents, U.S. Government Printing Office, Washington, D.C. 20402 Price 8.50 (paper cover) Library of Congrcss Catalog Card Nmbcr 66-60096 Foreword . .. At the opening of the tenth year in the era of man’s mobility in outer space, we can look back on 1966 as offering convincing evidence that the United States had gained great competence. This evidence included: five orbital space flights by ten Gemini astronauts; four lunar missions under- taking the orbiting of and softlanding on the moon; numerous contributions to scientific knowledge by unmanned spacecraft and sounding rockets; and further demonstrations of the practical utility of operational space systems, including weather and communications satellites. During 1966, a record 100 American spacecraft were placed into earth orbit or on escape trajectories. Thousands of revealing and useful pictures of the earth were taken from space and of the moon from lunar orbit and on its surface. The Gemini program ended with rendezvous and docking experiments and extravehicular activity by the Gemini test pilots as the Apollo R&D test flights leading to the manned lunar mission came into the schedule. Thirty-five major scientific, technological, and operational mile- stones were cited for 1966 by the President in his Report to the Congress on aeronautical and space activities of the United States.