2009 Handouts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2002 Annual Report
OF THE TOWN OFFICERS YEAR ENDING DECEMBER 2002 Burlington, Massachusetts Town of Burlington ANNUAL REPORT OF THE TOWN OFFICERS YEAR ENDING DECEMBER 2002 B URLINGTON M ASSACHUSETTS i Town of Burlington In Memoriam Frank E. Baxter, Planning Board Herman D. Graham, S. Josephine Ramsey, Planning Board School Teacher Margaret A. Burke, Election Worker Robert Guidoboni, Fire Dorothy Sousa, Town Hall Department Switchboard Operator Lincoln W. Daigle, Burlington Housing Authority Rita McKnight, School Teacher Amando Spinosa, Custodian Theresa D’Angelo, School Teacher Margaret Queen, School Teacher OF THE TOWN OFFICERS YEAR ENDING DECEMBER 2002 Burlington, Massachusetts ON THE COVER: Grandview Farm acquired by the Town in 2002. (Photo by Alan C. Nelson, cover by Peter Amirault of TYPE A) iii Town of Burlington TABLE OF CONTENTS Water Treatment Plant. 54 TOWN OF BURLINGTON OTHER DIRECTORY . vi Conservation Commission. 56 BCAT . 130 Board of Appeals . 58 Burlington Community INTRODUCTION Building Department . 58 Scholarship Foundation . 131 General Information. 1 Veterans Services . 60 Housing Authority . 134 Town Government Schedule . 1 Community Life Center . 64 Metropolitan Area Planning Council . 135 Town Offices Schedule. 2 B-Line Bus . 66 Officials Elected . 2 Council on Aging . 72 ADDENDA Treasurer/Collector. 74 GENERAL GOVERNMENT Town Meeting Members. 136 Assessors . 76 Board of Selectmen and Officials Appointed . 138 Planning Board. 77 Town Administrator . 3 Boards and Committees Recreation Department . 83 Human Resources . 7 Appointed . 138 Board of Health . 85 Town Counsel. 7 Town Meeting Minutes. 142 Health Agent/Sanitarian . 85 Town Clerk . 8 Town Accountant/ Environmental Engineer . 85 Financial Report. 159 Vital Statistics . 8 Mosquito Control Project, Voting Statistics/ East Middlesex . -
Copy 4/2/18 Template
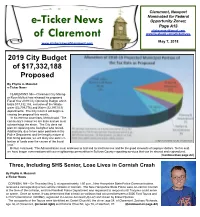
e-Ticker News of Claremont, Section A A!1 Claremont, Newport Nominated for Federal e-Ticker News Opportunity Zones; Page A13 [email protected] of Claremont www.facebook.com/etickernews May 7, 2018 www.etickernewsofclaremont.com 2019 City Budget of $17,332,188 Proposed By Phyllis A. Muzeroll e-Ticker News CLAREMONT, NH—Claremont City Manag- er Ryan McNutt has released his proposed Fiscal Year 2019 City Operating Budget which totals $17,332,188, exclusive of the Waste- water ($2,739,776) and Water ($2,197,013) departments. The City Council will begin re- viewing the proposal this month. In his letter to councilors, McNutt said, “The community’s resources are finite and we must acknowledge the strain. The City does not plan on replacing one firefighter who retired. Additionally, due to two open positions in the Police Department and the lengthy nature of that hiring process, we will likely see some re- tention of funds over the course of the fiscal Graphic provided by City of Claremont year.” McNutt continued, “The Administration must endeavor to find and fix inefficiencies and be the good stewards of taxpayer dollars. To this end, we have begun conversations with our neighboring communities in Sullivan County regarding services that can be shared and regionalized. (Continued on page A8) Three, Including SHS Senior, Lose Lives in Cornish Crash By Phyllis A. Muzeroll e-Ticker News CORNISH, NH—On Thursday May 3, at approximately 1:50 p.m., New Hampshire State Police Communications received a call regarding a two-vehicle collision in Cornish. The New Hampshire State Police were on-call for Cornish at the time of the collision, and the Plainfield Police Department was requested to respond until Troopers could arrive on scene. -

A Report of the House of Bishops' Working Party on Women in the Episcopate Church Ho
Women Bishops in the Church of England? A report of the House of Bishops’ Working Party on Women in the Episcopate Church House Publishing Church House Great Smith Street London SW1P 3NZ Tel: 020 7898 1451 Fax: 020 7989 1449 ISBN 0 7151 4037 X GS 1557 Printed in England by The Cromwell Press Ltd, Trowbridge, Wiltshire Published 2004 for the House of Bishops of the General Synod of the Church of England by Church House Publishing. Copyright © The Archbishops’ Council 2004 Index copyright © Meg Davies 2004 All rights reserved. No part of this publication may be reproduced or stored or transmitted by any means or in any form, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system without written permission, which should be sought from the Copyright Administrator, The Archbishops’ Council, Church of England, Church House, Great Smith Street, London SW1P 3NZ. Email: [email protected]. The Scripture quotations contained herein are from the New Revised Standard Version Bible, copyright © 1989, by the Division of Christian Education of the National Council of the Churches of Christ in the USA, and are used by permission. All rights reserved. Contents Membership of the Working Party vii Prefaceix Foreword by the Chair of the Working Party xi 1. Introduction 1 2. Episcopacy in the Church of England 8 3. How should we approach the issue of whether women 66 should be ordained as bishops? 4. The development of women’s ministry 114 in the Church of England 5. Can it be right in principle for women to be consecrated as 136 bishops in the Church of England? 6. -

Lisible Et Risible
LISIBLE ET RISIBLE Les noms et les titres sarcastiques dans une traduction anglaise de La Préférence Nationale de Fatou Diome par ©Sarah Martin Mémoire soumis à l’École des Études supérieures en vue des exigences partielles du diplôme de Maîtrise ès Lettres en Études françaises Département d’Études françaises et hispaniques Université Memorial Mai 2014 Saint-Jean Terre-Neuve ABRÉGÉ Ce mémoire se propose d’étudier le sarcasme: son usage, son lien fort avec la culture et sa traduisibilité. En traduisant La Préférence Nationale de Fatou Diome, nous examinons la difficulté de transmettre le sarcasme sous-entendu dans les noms et dans les titres de ce livre. Le traducteur comme médiateur linguistique et culturel doit jauger l’importance des éléments qui entrent en jeu pendant l’acte traduisant. Comme cette traduction anglaise nous le démontre, le traducteur doit souvent prendre la décision soit d’amener son lectorat vers l’écrivain soit d’amener l’écrivain vers son lectorat- un choix qui, entre autres, pourrait mettre en question la fidélité du traducteur. ABSTRACT This thesis proposes to study sarcasm: its use, its strong link to culture and its translatability. By translating Fatou Diome’s La Préférence Nationale, we examine the difficulty in conveying the implicit sarcasm in the names and the titles of this book. As both a linguistic and cultural intermediary, the translator has to gauge the importance of the elements that come into play during the translation process. As this English translation attempts to show, the translator must often make the decision to either steer his or her readership towards the author or to steer the author towards his or her readership- a choice that, amongst other things, might call into question the faithfulness of the translator. -

10Th Grade World History, Culture, and Geography: the Modern World
The Los Angeles Unified School District 10th Grade World History, Culture, and Geography: The Modern World Secondary Instructional Support Services History/Social Science Branch B INDER TITLE District Los Angeles Unified Schol 10TH GRADE W ORLD HISTORY, CULTURE, AND G EOGRAPHY: THE MODERN WORLD Table of Contents Preface Page A. Acknowledgements iii B. Mission/Vision Statement v C. Goals of the Instructional Guide vi D. History/Social Science Instructional Guide Overview vii E. Graphic Organizer of History/Social Science Instructional Guide ix Section I. Overview of Major District Initiatives A. Secondary Literacy Plan 1-1 B. The Nine Principles of Learning 1-3 C. Culturally Relevant Teaching Methods to Close the Achievement Gap 1-5 D. Small Learning Communities 1-6 Section II. Overview of State of California Documents A. California Content Standards 2-1 B. History/Social Science Framework for California Public Schools 2-1 C. California Standards for the Teaching Profession 2-2 Section III. History/Social Science Pedagogy A. Philosophy 3-1 B. Disciplinary Literacy 3-1 C. Thinking, Reading, and Writing Historically 3-3 D. The Use of Primary Sources 3-5 E. Strategies Used in the Instructional Guide 3-6 F. Student Engagement 3-7 G. Academic Skills Grade 10 3-8 Section IV. Overview of Assessment A. The Role of Assessment 4-1 B. The Use of Common Assessments 4-1 C. Scoring 4-2 D. Intervention 4-2 E. Sample Periodic Assessment 4-3 F. Sample Short Constructed Response 4-4 Section V. Instructional Component One A. Introduction to the Curricular Map 5-1 B. -

Our 2020 Annual Report! Download It Here!
2020 ANNUAL REPORT Your hardest times often lead to the greatest moments of your life. Keep going. Tough situations build strong people in the end. - Roy T. Bennett Photo by DeVane Webster of Beulah, ND, StoneyLonesomePhotos.com About Our Year NDCF Board of Directors ............................................................................................ 4 Mission Statement Letter from our Chair & CEO ...................................................................................... 5 The mission of the North Dakota Community Foundation is to improve the quality of life for North Dakota’s citizens through charitable giving and promoting philanthropy. 2020 At-A-Glance .......................................................................................................... 6 Our Community Foundations ..................................................................................... 8 About the North Dakota Community Foundation The North Dakota Community Foundation was incorporated in 1976. NDCF is an IRS designated Our Statewide Greatest Needs Fund .........................................................................10 501(c)(3) statewide, public, nonprofit, tax-exempt corporation that receives and distributes New Funds in 2020 ......................................................................................................12 charitable funds to support a wide range of programs that benefit North Dakotans. NDCF was formed by a group of concerned citizens who were looking for a general charitable vehicle ..............................................................................................15 -

Foreign Students As Members for Senior Class Presidency
SERVING THE STORRS COMMUNITY Established Weather 1896 Cloudy and Cool Member Of The United Press (ftmmwttntf (SamjntH Vol. XL Storrs, Connecticut. Thursday. October 22. 1953 No 24 International House Organization!^^ \A/jns \$Q Nomination Now Numbers Over Sixty j Foreign students As Members For Senior Class Presidency Uy Joan Lee Bradshaw n Miniature' After one year's absence from International House is the Carradine To Present name of an organization recently campus politics the Independent formed on this campus with 0 Students Organization returned membership of 60 students from Dramatic Selections to activity last Tuesday night by foreign lands. As yet they real- nominating Harold Hook for ly have no house to call their At Third Convocation president of the Senior Class. own, but their president, Emman- uel (Manos) Marcoglou, says: John Carradine, well-known George Zondiros, president of "For the time being we will be Shakespearean actor, will present the Student Senate, made an ap- satisfied to have a permanent a drar latic program of "Gnat pearance at the primary and wel- room."' Scenes from Great Literature," comed the party back to campus At its second meeting last on Oct. 29 in the HUB ballroom politics, wishing it "every possi- week the group ratified a con- at 8 p. m. This will be the third stitution and elected officers and convocation in the 1953-54 series. ble success." three committee chairmen. En- In his program, Mr. Carradine Nominees for the other offices thusiastic about their objective will present some of the best of the Senior Class are Patricia "to promote cultural exchange known scenes from Shakespeare Moriarty, vice president; Rudy between Americans and foreign and will include selections from students," the members are al- other great English poets, as well Favretti, treasurer; Ann Jaku- ready preparing to participate in as several readings from Abra- bauskas, secretary; Kenneth Les- a campus program on the United ham Lincoln's addresses. -
2017-Annual-Report-Printer-Final-3
969 E. Swedesford Road, Exton, PA 19341 Phone: 610-647-4940 Fax: 610-240-7268 - [email protected] www.homeofthesparrow.org The Artful Framer Mark Delowery Bajeerah LaCava Red Hat Ladies of Hillview The Grand Opera House Tricia DeMarini Cindy Laudato Debbie Reif The Institutes Jack Dembow Robbi Lee Susan & Samuel Reisbord Dear Friends, The Master’s Baker Janice Detweiler Levin Luminais Chronister Cindy, Tim, Garrett & Justin The McKee Group Devon Tile Eye Associates Roach What an exciting year of changes it has been here at Home of the Sparrow! A new CEO, a new The Media Theatre Rosemary DiGiandomenico Christy Levy Elisa Rodgers venue for Jazz on the Main Line and, of course, so many new wonderful friends who have joined Sue Thomas Karen DiVincenzo Bridget Lininger Stephanie Rodriguez Ashley Thompson Barbara Dougherty Lionville Storage Jennifer Rosback us in our mission to change the lives of women and children in our community. Suzanne Graham Thurman Downingtown UM Church Cara Locke Stephanie Roth Topiary Claire Dukes Kaitlin Lore Kristina Rowshan Thanks to your support, we were able to help nearly 550 women and children through our programs Urban Air Trampoline Park Adrianna Duranti Kathy Lovell Bonnie Sabbi this year. Our amazing team works extremely hard every day to prevent and end homelessness in USLI Linda Durkin Jessica Luff Sabic Chester County. But, unfortunately, the numbers of those in need are increasing at an alarming rate. Aileen Vaughan Barbara Ellixson Alicia Luke Joan & Mike Sabrick Michelle Venema Cleo Elkinton Ashley MacIntyre Rene Sacco It’s difficult to grasp that, in our beautiful county, nearly 600 people are homeless on any given night. -

Universidade De São Paulo Escola De Comunicações E
UNIVERSIDADE DE SÃO PAULO! ESCOLA DE COMUNICAÇÕES E ARTES! PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIAS DA COMUNICAÇÃO JOAQUIM CARDIA GHIROTTI Frank Miller e os quadrinhos: pelo que vale a pena morrer SÃO PAULO 2017 JOAQUIM CARDIA GHIROTTI Frank Miller e os quadrinhos: pelo que vale a pena morrer Tese apresentada ao Programa de Pós-Graduação em Ciências da Comunicação da Escola de Comunicações e Artes da Universidade de São Paulo para a obtenção do título de Doutor em Ciências da Comunicação Área de Concentração: Interfaces sociais da Comunicação Linha de Pesquisa: Comunicação, Cultura e Cidadania Orientador: Prof. Dr. Waldomiro de Castro Santos Vergueiro SÃO PAULO 2017 Autorizo a reprodução e a divulgação parcial deste trabalho, por qualquer meio convencional ou eletrônico, para fins de estudo e pesquisa, desde que citada a fonte. GHIROTTI, J. C. Frank Miller e os quadrinhos: pelo que vale a pena morrer. Tese apresentada à Escola de Comunicações e Artes da Universidade de São Paulo para a obtenção do título de Doutor em Ciências da Comunicação. Aprovado em: Banca examinadora Prof. Dr. Waldomiro de Castro Santos Vergueiro (orientador) Julgamento:________________________________Assinatura:__________________ Julgamento:________________________________Assinatura:__________________ Julgamento:________________________________Assinatura:__________________ Julgamento:________________________________Assinatura:__________________ Julgamento:________________________________Assinatura:__________________ “Worth dying for. Worth killing for. Worth going to hell for. Amen.” - Frank Miller, Sin City. Agradeço ao professor Waldomiro Vergueiro, por ter aceitado o desafio desta pesquisa, e me dado a oportunidade e o privilégio de ter sua orientação, sua liderança sempre certeira, criteriosa, clarificadora, que foi fundamental para a lapidação, o desenvolvimento e a maturação deste trabalho. Acima de tudo, pela inspiração. -

Projeto Expocom 2011 Roteiro
Intercom – Sociedade Brasileira de Estudos Interdisciplinares da Comunicação XVI Congresso de Ciências da Comunicação na Região Sudeste – São Paulo - SP – 12 a 14 de maio de 2011 TRANSTORNO 1 Antonio GRELLA 2 Caio SENICATO 3 Guilherme GHISI4 Leandro de CARVALHO 5 Orlando BRANDÃO 6 Fernando BISCALCHIN 7 Universidade Metodista de Piracicaba – UNIMEP, Piracicaba, SP RESUMO Realizado como trabalho de conclusão de curso (TCC) e baseado na monografia “Convergência Midiática e Transmídia: Novas maneiras de produção 8”, o curta-metragem TRANSTORNO é composto por um roteiro transmidiático, que foge da plataforma vídeo e se complementa nas plataformas rádio e internet. Na trama, um psicólogo que perdeu mulher, filha e o movimento das pernas em um assalto, revive os reflexos desse fato quando um radialista transmite o som do assalto, registrado em uma câmera de vídeo. PALAVRAS-CHAVE: TRANSTORNO; transmidia; Ouvindo a Morte; INTRODUÇÃO O curso de rádio e televisão da UNIMEP não tem como objetivo apenas formar profissionais na área de comunicação, traz como base também a formação de divulgadores da cultura local e/ou regional, provando assim, que as produções audiovisuais de qualidade e profissionalismo não estão localizadas apenas nos grandes centros. A facilidade tecnológica e com o apoio de empresas locais, o interior do Brasil tem muito a mostrar e muitas pessoas para fazê-lo. A Filma Nóis Produções, produtora sem fins lucrativos formada pelos alunos formados do curso de rádio e TV para a execução dos projetos curriculares e se dividiu em duas equipes 1 Trabalho submetido ao XVIII Prêmio Expocom 2011, na Categoria Cinema e Audiovisual , modalidade Roteiro (avulso). -

Executive Branch
CHAPTER 2 EXECUTIVE BRANCH Walter Stollmeyer proudly stands next to his brand new Ford Touring Car, purchased in Herman, Missouri for $585.00 in 1919. (photo courtesy of Norma Maier) 32 OFFICIAL MANUAL Jeremiah W. (Jay) Nixon Governor Elected November 4, 2008 Term expires January 2013 JAY NIXON (Democrat) is serving his fi rst term as governor of Missouri. Garnering the highest margin of victory for a non- incumbent governor in 44 years, Nixon was overwhelmingly elected by Missourians as their 55th governor to create jobs and move the state forward. Governor Nixon has put forward an agenda to make govern- ment more effi cient, effective and responsive to the needs of Missouri families. He is committed to fi ghting every day to create jobs in Missouri, holding the line on taxes and placing a college education within reach for more Missouri students. As he did in the state Senate and during four terms as attor- ney general, Governor Nixon is reaching across the aisle to put Missouri families fi rst. He successfully worked with the legislature to pass several jobs initiatives to put Missourians back to work, including a bill to bring next-generation automotive production to Missouri. Nixon’s call to reform Missouri’s drunk-driving laws resulted in changes to keep repeat offenders off the road. Governor Nixon has led the fi ght for families with children with special needs, including the successful push to require insurance companies to cover proven treatments for autism disorders, as well as the creation of Partnership for Hope, which is helping provide community-based services to those with developmental disabilities. -

A Path Toward Racial Equity
A PATH TOWARD RACIAL EQUITY A printed companion to FORWARDTHROUGHFERGUSON.ORG as of September 14TH #STLFwdThru CONTENTS INTRODUCTION THE CONTEXT OF THE FERGUSON COMMISSION REPORT . 6 ABOUT THIS REPORT. 8 ABOUT THE FERGUSON COMMISSION . 12 THE PROCESS OF CHANGE . 18 NEXT STEPS . 20 SIGNATURE PRIORITIES JUSTICE FOR ALL . 24 YOUTH AT THE CENTER . 38 OPPORTUNITY TO THRIVE . 48 RACIAL EQUITY . 59 CALLS TO ACTION ALL JUSTICE FOR ALL CALLS . 61 ALL YOUTH AT THE CENTER CALLS . 101 ALL OPPORTUNITY TO THRIVE CALLS . 127 ALL RACIAL EQUITY CALLS . 151 SUMMARY OF TERMS . 155 ACKNOWLEDGEMENTS CONTENT EXPERTS . 170 WORKING GROUP MEMBERS . 172 COMMISSIONERS . 174 COMMISSION RESOURCES AND SUPPORT . 175 DEMOGRAPHICS RECAP . 179 INTRODUCTION THE CONTEXT OF THE FERGUSON COMMISSION REPORT CLARIFYING OUR TERMS are the answer. We can’t. But they are what we believe to be the best starting point, the beginning of a path toward The title of this report is “Forward Through Ferguson: a better St. Louis. A Path Toward Racial Equity.” We want to take a few moments to explain what we mean. We expect that as we travel, the path will change, and we’ll find ourselves navigating places we couldn’t have “FORWARD THROUGH FERGUSON” imagined. That is the nature of efforts like this. But there must be a starting point, and we believe, based on the As with any organization that works closely together on work we have done, that this is the right starting point. serious issues, the Ferguson Commission has found itself coming back to several phrases again and again. One We are certainly open to the idea that we will uncover of those phrases has been, “The only way forward is new routes and unexpected roadblocks.