2020.11.16.20232322V1.Full.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

Vulnerable-Groups-Assessment-And-Gender-Analysis-Of-Human-Trafficking-High-Risk
Monograph Series Vol. 15 ii iii Disclaimer The MADE monograph and learning series is planned to help provide information and knowledge for dissemination. We believe the information will contribute to sector dialogues and conversations around development in Nigeria. The content in the series was prepared as an account of work sponsored by the Market Development in the Niger Delta (MADE). The documents in this series is the final submission made by the engaged service provider/consultant. The series does not represent the views of MADE, the UKaid, The Department for International Development (DFiD) Development Alternatives Incorporated (DAI), nor any of their employees. MADE, DFID, UKaid and DAI do not assume any legal liability or responsibility for the accuracy, completeness, or any third party's use of any information, or process disclosed, or representation that infringes on privately owned rights. Reference herein to any specific commercial product, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favouring by MADE, DFID, UKaid and/or DAI. iv TABLE OF CONTENTS TABLE OF CONTENTS ........................................................................................................................................... iv LIST OF TABLES .................................................................................................................................................... vi LIST OF FIGURES ................................................................................................................................................. -
The Perception of Edo People on International and Irregular Migration
THE PERCEPTION OF EDO PEOPLE ON INTERNATIONAL AND IRREGULAR MIGRATION BY EDO STATE TASK FORCE AGAINST HUMAN TRAFFICKING (ETAHT) Supported by DFID funded Market Development Programme in the Niger Delta being implemented by Development Alternatives Incorporated. Lead Consultant: Professor (Mrs) K. A. Eghafona Department Of Sociology And Anthropology University Of Benin Observatory Researcher: Dr. Lugard Ibhafidon Sadoh Department Of Sociology And Anthropology University Of Benin Observatory Quality Control Team Lead: Okereke Chigozie Data analyst ETAHT Foreword: Professor (Mrs) Yinka Omorogbe Chairperson ETAHT March 2019 i List of Abbreviations and Acronyms AHT Anti-human Trafficking CDC Community Development Committee EUROPOL European Union Agency for Law Enforcement Cooperation (formerly the European Police Office and Europol Drugs Unit) ETAHT Edo State Task Force Against Human Trafficking HT Human trafficking IOM International Organization for Migration LGA Local Government Area NAPTIP National Agency For Prohibition of Traffic In Persons & Other Related Matters NGO Non-Governmental Organization SEEDS (Edo) State Economic Empowerment and Development Strategy TIP Trafficking in Persons UN United Nations UNODC United Nations Office on Drug and Crime USA United States of America ii Acknowledgements This perception study was carried out by the Edo State Taskforce Against Human Trafficking (ETAHT) using the service of a consultant from the University of Benin Observatory within the framework of the project Counter Trafficking Initiative. We are particularly grateful to the chairperson of ETAHT and Attorney General of Edo State; Professor Mrs. Yinka Omorogbe for her support in actualizing this project. The effort of Mr. Chigozie Okereke and other staff of ETAHT who provided assistance towards the actualization of this task is immensely appreciated. -

Gully Erosion Problems in Selected Areas of Edo State: Factors and Control
Nigerian Journal of Environmental Sciences and Technology (NIJEST) www.nijest.com ISSN (Print): 2616-051X | ISSN (electronic): 2616-0501 Vol 3, No. 1 March 2019, pp 161 - 173 Gully Erosion Problems in Selected Areas of Edo State: Factors and Control Kayode-Ojo N.1,*, Ikhide A. O.2 and Ehiorobo J. O.3 1,2,3Department of Civil Engineering, University of Benin, Benin City, Edo State, Nigeria Corresponding Author: *[email protected] ABSTRACT Gully erosion is a serious ecological problem in Edo State and has negative impact on agricultural productivity, lives and properties in both urban and rural environments. This paper therefore aims at identifying factors contributing to the formation of gullies and methods of controlling them so that further environmental degradation would be averted. Three gully sites were selected from the three geo-political zones of the State. Data were collected through remote sensing, field topographical survey and soil sampling on gully walls and gully beds. Meteorological and hydrological data were also collected. Slope stability analysis was also carried out. The Kerby- Kirpich equation was applied to estimate the overall time of concentration and Rational formula used to determine the peak discharge. The study revealed that the selected study areas possess all the characteristics of an erosion prone area which are: rainfall of very high intensity, steep slopes resulting in large runoff and soil with low organic content and relatively low shear strength obtained from the geotechnical investigations. Results from the studies revealed that the gully width and depth varied considerably from top to bottom. The cross section shows that the gully is U- shaped for Ekehuan gully and V-shaped for Auchi and Ewu gullies, indicating a large catchment area and a large volume of discharge passing through the gully. -

ZONAL INTERVENTION PROJECTS Federal Goverment of Nigeria APPROPRIATION ACT
2014 APPROPRIATION ACT ZONAL INTERVENTION PROJECTS Federal Goverment of Nigeria APPROPRIATION ACT Federal Government of Nigeria 2014 APPROPRIATION ACT S/NO PROJECT TITLE AMOUNT AGENCY =N= 1 CONSTRUCTION OF ZING-YAKOKO-MONKIN ROAD, TARABA STATE 300,000,000 WORKS 2 CONSTRUCTION OF AJELE ROAD, ESAN SOUTH EAST LGA, EDO CENTRAL SENATORIAL 80,000,000 WORKS DISTRICT, EDO STATE 3 YOUTH DEVELOPMENT CENTRE, OTADA, OTUKPO, BENUE STATE (ONGOING) 150,000,000 YOUTH 4 YOUTH DEVELOPMENT CENTRE, OBI, BENUE STATE (ONGOING) 110,000,000 YOUTH 5 YOUTH DEVELOPMENT CENTRE, AGATU, BENUE STATE (ONGOING) 110,000,000 YOUTH 6 YOUTH DEVELOPMENT CENTRE-MPU,ANINRI LGA ENUGU STATE 70,000,000 YOUTH 7 YOUTH DEVELOPMENT CENTRE-AWGU, ENUGU STATE 150,000,000 YOUTH 8 YOUTH DEVELOPMENT CENTRE-ACHI,OJI RIVER ENUGU STATE 70,000,000 YOUTH 9 YOUTH DEVELOPMENT CENTRE-NGWO UDI LGA ENUGU STATE 100,000,000 YOUTH 10 YOUTH DEVELOPMENT CENTRE- IWOLLO, EZEAGU LGA, ENUGU STATE 100,000,000 YOUTH 11 YOUTH EMPOWERMENT PROGRAMME IN LAGOS WEST SENATORIAL DISTRICT, LAGOS STATE 250,000,000 YOUTH 12 COMPLETION OF YOUTH DEVELOPMENT CENTRE AT BADAGRY LGA, LAGOS 200,000,000 YOUTH 13 YOUTH DEVELOPMENT CENTRE IN IKOM, CROSS RIVER CENTRAL SENATORIAL DISTRICT, CROSS 34,000,000 YOUTH RIVER STATE (ON-GOING) 14 ELECTRIFICATION OF ALIFETI-OBA-IGA OLOGBECHE IN APA LGA, BENUE 25,000,000 REA 15 ELECTRIFICATION OF OJAGBAMA ADOKA, OTUKPO LGA, BENUE (NEW) 25,000,000 REA 16 POWER IMPROVEMENT AND PROCUREMENT AND INSTALLATION OF TRANSFORMERS IN 280,000,000 POWER OTUKPO LGA (NEW) 17 ELECTRIFICATION OF ZING—YAKOKO—MONKIN (ON-GOING) 100,000,000 POWER ADD100M 18 SUPPLY OF 10 NOS. -
States and Lcdas Codes.Cdr
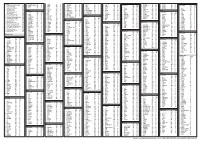
PFA CODES 28 UKANEFUN KPK AK 6 CHIBOK CBK BO 8 ETSAKO-EAST AGD ED 20 ONUIMO KWE IM 32 RIMIN-GADO RMG KN KWARA 9 IJEBU-NORTH JGB OG 30 OYO-EAST YYY OY YOBE 1 Stanbic IBTC Pension Managers Limited 0021 29 URU OFFONG ORUKO UFG AK 7 DAMBOA DAM BO 9 ETSAKO-WEST AUC ED 21 ORLU RLU IM 33 ROGO RGG KN S/N LGA NAME LGA STATE 10 IJEBU-NORTH-EAST JNE OG 31 SAKI-EAST GMD OY S/N LGA NAME LGA STATE 2 Premium Pension Limited 0022 30 URUAN DUU AK 8 DIKWA DKW BO 10 IGUEBEN GUE ED 22 ORSU AWT IM 34 SHANONO SNN KN CODE CODE 11 IJEBU-ODE JBD OG 32 SAKI-WEST SHK OY CODE CODE 3 Leadway Pensure PFA Limited 0023 31 UYO UYY AK 9 GUBIO GUB BO 11 IKPOBA-OKHA DGE ED 23 ORU-EAST MMA IM 35 SUMAILA SML KN 1 ASA AFN KW 12 IKENNE KNN OG 33 SURULERE RSD OY 1 BADE GSH YB 4 Sigma Pensions Limited 0024 10 GUZAMALA GZM BO 12 OREDO BEN ED 24 ORU-WEST NGB IM 36 TAKAI TAK KN 2 BARUTEN KSB KW 13 IMEKO-AFON MEK OG 2 BOSARI DPH YB 5 Pensions Alliance Limited 0025 ANAMBRA 11 GWOZA GZA BO 13 ORHIONMWON ABD ED 25 OWERRI-MUNICIPAL WER IM 37 TARAUNI TRN KN 3 EDU LAF KW 14 IPOKIA PKA OG PLATEAU 3 DAMATURU DTR YB 6 ARM Pension Managers Limited 0026 S/N LGA NAME LGA STATE 12 HAWUL HWL BO 14 OVIA-NORTH-EAST AKA ED 26 26 OWERRI-NORTH RRT IM 38 TOFA TEA KN 4 EKITI ARP KW 15 OBAFEMI OWODE WDE OG S/N LGA NAME LGA STATE 4 FIKA FKA YB 7 Trustfund Pensions Plc 0028 CODE CODE 13 JERE JRE BO 15 OVIA-SOUTH-WEST GBZ ED 27 27 OWERRI-WEST UMG IM 39 TSANYAWA TYW KN 5 IFELODUN SHA KW 16 ODEDAH DED OG CODE CODE 5 FUNE FUN YB 8 First Guarantee Pension Limited 0029 1 AGUATA AGU AN 14 KAGA KGG BO 16 OWAN-EAST -

ADVERTISEMENT of APPLICANTS for LAND REGISTRATION
ADVERTISEMENT of APPLICANTS FOR LAND REGISTRATION 1. The underlisted applications have been received under the Land Use Decree of 1978 for grant of Statutory Right of Occupancy. 2. Any member of the public who may wish to object to any of the applications below should do so within 21 days of this publication. 3. Notice of objection should be accompanied with the copies of a sworn affidavit, evidence of ownership of title and a non‐refundable fee of N20,000 (Twenty thousand Naira) for each objection and addressed to the Managing Director, Edo State Geographic Information Service, 102 Sapele Road, Benin City. 4. TAKE NOTE: SHORTLY ALL PROPERTIES FOR REGISTRATION WILL TAKE PLACE ON THE EDOGIS WEBSITE: www.edogis.org Signed: Francis Evbuomwan Managing Director Edo State Geographic Information Service EDOGIS EGOR LOCAL GOVERNMENT AREA S/N Name(s) File Number Particulars of Plot 1 STELLA OBIAGERI IRUKA EDL 54795 A Parcel of Land at Ward 23l, Egua-Edaiken Quarters, Benin City, Edo State transferred from Madam Omoyemwen Erhubabodu as shown on survey plan no. SMD/EDO/2020/1129 and having an area of 495.34m2 and delineated by beacons: AA8736ZF, AA8735ZF, AA8737ZF, AA8734ZF and being RESIDENTIAL and DEVELOPED. ETSAKO WEST LOCAL GOVERNMENT AREA S/N Name(s) File Number Particulars of Plot 2 EMMANUEL ABIODUN EDL 47964 A Parcel of Land Behind Edo State University Iyamho, Edo State transferred from Mr. Peter Aduku AGBOMABINU as shown on survey plan no. APP/ED/006/20 and having an area of 998.44m2 and delineated by beacons: AA790AQ, AA791AQ, AA782AQ, AA783AQ and being RESIDENTIAL and UNDEVELOPED. -

Organized Crime Facts Edo State
ORGANIZED CRIME FACTS • EDO STATE GEOPOLITICAL INTELLIGENCE CRIME INTELLIGENCE MARITIME INTELLIGENCE SPECIAL INVESTIGATION BREAKING NEWS INCIDENT ALERT SYSTEM Location: Lagos, Nigeria [email protected] +2349083588787 Being inundated with fears over the rising spate Gifting the delegation as we sat to deliberate on of insecurity in the nation, I always find solace the reason for our visit from their variety of in working from the comfort of my office's natural resources, we could not help but blot bounded walls. Therefore my dismay came to a out:what went wrong that the nation's crescendo when my organization nominated heartbeat has transformed into the nightmare me as part of a high profiled delegation to of travellers and residents alike? investigate the accelerated spate of the insecurity situation in Edo State. Recall that #ENDSARS protest hijacked by hoodlums resulted in a prison break within the Benin City is the state capital and largest urban state. Anticipation became rife that hoodlums centre, tilting more than 1,800feet in the north wreak of terror in Edo state would abate with while lying at elevations between 500 feet in time. However, the magnitude and intensity the south. Edo state bounded by Kogi to the took a turn for the worse. The gravity has northeast and east, Anambra to the degenerated to an equilibrium where Edo state east, Delta to the southeast and south, sends jitters. and Ondo to the west and northwest; is famous for its unique bronze, brass and ivory works of Kidnapping, armed robbery and cultism have arts which are found all over the world in recently reached its peak within and around the museums. -

Conflict Incident Monthly Tracker
Conflict Incident Monthly Tracker Edo State: February - M arch 2 01 8 B a ck gro und The incident led to heightened tensions in Arson: In February, a man reportedly set the area. ablaze the house he inherited from his father This monthly tracker is designed to update over payment of rent in Oredo LGA. Over 20 Peace Agents on patterns and trends in Violence Affecting Women and Girls shops were destroyed. The man resisted conflict risk and violence, as identified by the (VAWG): In January, two brothers attempts by neighbors to stop the fire, Integrated Peace and Development Unit reportedly killed their grandmother for claiming it is better for him to burn down the (IPDU) early warning system, and to seek ritualistic purposes in Ikpoba-Okha LGA. house than to allow tenants stay for free. feedback and input for response to mitigate Separately, a retired female military officer areas of conflict. was reportedly killed and set ablaze in her Recent Incidents or house by her security guard in Benin City, Patterns and Trends the state capital. Also, in January, a Issues, March 2018 herdsman reportedly inflicted a fatal injury D ec 2 01 7 -Fe b 20 1 8 Incidents reported during the month mainly on a woman at her farm in Akoko-Edo LGA. According to Peace Map data (see Figure 1), related to communal tensions, and reported incidents during this period Violent Protest: In February, four people criminality. including a policeman were reported dead included criminality, communal tensions, Communal Tensions: Residents of Odighi during a protest over the dead of a 26-year protests, and violence affecting women and and Odiguetue communities in Oredo LGA old commercial driver in Benin City, Oredo girls. -

Effects of Climate Change on Irrigation Activities: a Case Study of the Benin-Owena River Basin Irrigation Projects
Water Resources Systems—Hydrological Risk, Memagement and Development (Proceedings of symposium IIS02b held during 1UGG2003 at Sapporo, July 2003). IAHS Publ. no. 281, 2003. 287 Effects of climate change on irrigation activities: a case study of the Benin-Owena River basin irrigation projects CATHERINE I. IKHILE Department of Geography and Regional Planning, University of Benin, PMB 1154, Benin City, Nigeria [email protected] GEORGE U. IKHILE c/o Scripture Union (Nigeria), PO Box 743, Benin City, Nigeria Abstract The effects of climate change on irrigation activities in the Benin- Owena River Basin (BORB), southwestern Nigeria, were investigated, using rainfall and temperature data from 1961 to 2000 with irrigation activity data from 1990 to 2000. Climate records showed a large variation in annual rainfall between 1961-1980. The rainfall variation between 1980-2000 was less pronounced, and rainfall was much lower. The period 1982-1986 exhibited the greatest downward trend in rainfall. The decadal range of temperature showed a gradual warming of the environment. Increasing temperatures and decreasing rainfall, coupled with an increasing population, led farmers and policy makers in Nigeria to embark on massive irrigation activities from the 1990s to 2000. Farm productivity levels and irrigations activities in Edo State are discussed. Key words Benin-Owena River basin; climate change; irrigation; Nigeria; rainfall; temperature INTRODUCTION Over the years, the Federal Government of Nigeria has launched several agricultural programmes (Sanda et ai, 1994; Imoudu et al., 2001) to adopt irrigation agriculture as a means of achieving the government's objective of self-sufficiency in food and fibre production. The history of irrigation activities in Edo State is attributable to the sub- Saharan West African drought and desertification of the late 1970s and early 1980s (Oyebande et al., 1978; Nicolson, 1980; Lamb, 1982; Olaniran et al, 1991). -

Conflict Incident Monthly Tracker
Conflict Incident Monthly Tracker Edo State: October - November 2018 B a ck gro und patent medicine dealer was reportedly killed Violence Affecting Women and Girls during a clash between members of the (VAWG): In addition to the impact of This monthly tracker is designed to update Black Axe and Aiye confraternities in Auchi, criminality on women and girls listed above, Peace Agents on patterns and trends in Etsako West LGA. In another incident, six domestic violence against women was also conflict risk and violence, as identified by the students were reportedly killed by cultists reported during this period. In October, for Integrated Peace and Development Unit during a graduation ceremony in Ekpoma, instance, a 35-year old man was reportedly (IPDU) early warning system, and to seek Esan West LGA. In October, over 20 people arrested by the police for impregnating his feedback and input for response to mitigate were reportedly killed in renewed rival cult 13-year old daughter in Ologbo community, areas of conflict. clashes in Benin City and its environs in Ikpoba Okha LGA. Separately, a 75-year old Patterns and Trends Oredo LGA. man was reportedly sentenced to seven A u gust -October 2018 Political Violence: In October, sporadic years imprisonment for raping a 10-year old shooting was reported at the premises of the girl in Igarra town, Akoko Edo LGA. According to Peace Map data (see Figure 1), Edo State House of Assembly as the Deputy there was an increase in lethal violence in Recent Incidents, Speaker was reportedly impeached in Benin Edo state in October 2018. -

Conflict Bulletin: Edo State
The Fund for Peace Conflict Bulletin: Edo State July 2014 of six governors affiliated with the Action Congress of Nigeria Party (ACN). LGA Level Summary Edo was one of the Niger Delta’s more January 2012 - June 2014 violent states on a per-capita basis from 2012 to mid 2014, with about 113 incidents Oredo claiming the lives of over 250 people. Reported incidents of violence and Home to the state’s capital, Benin City, associated fatalities have increased since Oredo LGA experienced collective violence 2012. Issues in Edo ranged from protests, between gangs, cult groups, religious criminality, abductions and domestic groups, political groups and communities violence to clashes between gangs, cults, during this period. In January 2012, a cult political groups and communities. Over half clash between Eiye and Black Axe of these incidents were reported in the confraternities reportedly killed eight over Oredo Local Government Area (LGA), home the course of a week, while two similar andlocked between Ondo, Kogi and to Benin City, although violence was also clashes in June and July 2012 led to the Delta States, Edo is home to about reported further north, notably in the Esan deaths of three and four respectively. The 3.2 million people (2006 census), West, Uhunmwonde, and Etsako Central, same Eiye Confraternity also lost some of its predominantly of Edo, Bini, Owan, East and West LGAs. members through an intra-cult clash in Esan, and Afemai background. Edo’s November 2013. Violence between the Eiye economy centers around agriculture, This Conflict Bulletin provides a brief and Aye (Black Axe) confraternities including food crops such as yams, cassava, snapshot of the trends and patterns of continued in 2014, killing four in January.