Inter-Observer Agreement of Computed Tomography and Magnetic Resonance Imaging on Gross Tumor Volume Delineation of Intrahepatic Cholangiocarcinoma: an Initial Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
SGS-Safeguards 04910- Minimum Wages Increased in Jiangsu -EN-10
SAFEGUARDS SGS CONSUMER TESTING SERVICES CORPORATE SOCIAL RESPONSIILITY SOLUTIONS NO. 049/10 MARCH 2010 MINIMUM WAGES INCREASED IN JIANGSU Jiangsu becomes the first province to raise minimum wages in China in 2010, with an average increase of over 12% effective from 1 February 2010. Since 2008, many local governments have deferred the plan of adjusting minimum wages due to the financial crisis. As economic results are improving, the government of Jiangsu Province has decided to raise the minimum wages. On January 23, 2010, the Department of Human Resources and Social Security of Jiangsu Province declared that the minimum wages in Jiangsu Province would be increased from February 1, 2010 according to Interim Provisions on Minimum Wages of Enterprises in Jiangsu Province and Minimum Wages Standard issued by the central government. Adjustment of minimum wages in Jiangsu Province The minimum wages do not include: Adjusted minimum wages: • Overtime payment; • Monthly minimum wages: • Allowances given for the Areas under the first category (please refer to the table on next page): middle shift, night shift, and 960 yuan/month; work in particular environments Areas under the second category: 790 yuan/month; such as high or low Areas under the third category: 670 yuan/month temperature, underground • Hourly minimum wages: operations, toxicity and other Areas under the first category: 7.8 yuan/hour; potentially harmful Areas under the second category: 6.4 yuan/hour; environments; Areas under the third category: 5.4 yuan/hour. • The welfare prescribed in the laws and regulations. CORPORATE SOCIAL RESPONSIILITY SOLUTIONS NO. 049/10 MARCH 2010 P.2 Hourly minimum wages are calculated on the basis of the announced monthly minimum wages, taking into account: • The basic pension insurance premiums and the basic medical insurance premiums that shall be paid by the employers. -

Updates on Chinese Port Information During COVID-19 Outbreak - 10.03.2020
Moir Alistair From: Harris Guy Sent: 12 March 2020 15:40 To: Group - IR Subject: FW: Huatai Info-Updates on Chinese Port Information during COVID-19 outbreak - 10.03.2020 Importance: High trProcessed: Sent From: 北京海事 <[email protected]> Sent: 10 March 2020 13:26 To: Chan Connie <[email protected]> Subject: Huatai Info-Updates on Chinese Port Information during COVID-19 outbreak. - Mar 10th, 2020 Dear Sirs/Madams, With the improvement of the epidemic situation, work resumption is taking place across China except for Hubei province, the hardest-hit region. With the increase of overseas COVID-19 cases, ports are becoming the front line of the battle against the epidemic. Most protective measures implemented by port authorities are still in force and we suggest shipowners to keep on following the notice we made in our previous Huatai Info to avoid any problems. Please note that to date our Huatai offices have come back to normal operating condition. Though some of our staff continues to work from home, they can be reached by email and mobile phone as normal. Besides the daily case handling, we shall keep collecting relevant information on COVID-19 related policy as well as latest port situation to protect Club/Members’ best interests. At the end of this Info we hereby provide the updated port information collected from local parties concerned (port authorities, survey firms, etc.) to help Club/Members make the best arrangement when your good vessel facing any potential claims during calling at Chinese ports. We really appreciate all your thoughtfulness and concern about our situation during Covid-19 epidemic. -

Results Announcement for the Year Ended December 31, 2020
(GDR under the symbol "HTSC") RESULTS ANNOUNCEMENT FOR THE YEAR ENDED DECEMBER 31, 2020 The Board of Huatai Securities Co., Ltd. (the "Company") hereby announces the audited results of the Company and its subsidiaries for the year ended December 31, 2020. This announcement contains the full text of the annual results announcement of the Company for 2020. PUBLICATION OF THE ANNUAL RESULTS ANNOUNCEMENT AND THE ANNUAL REPORT This results announcement of the Company will be available on the website of London Stock Exchange (www.londonstockexchange.com), the website of National Storage Mechanism (data.fca.org.uk/#/nsm/nationalstoragemechanism), and the website of the Company (www.htsc.com.cn), respectively. The annual report of the Company for 2020 will be available on the website of London Stock Exchange (www.londonstockexchange.com), the website of the National Storage Mechanism (data.fca.org.uk/#/nsm/nationalstoragemechanism) and the website of the Company in due course on or before April 30, 2021. DEFINITIONS Unless the context otherwise requires, capitalized terms used in this announcement shall have the same meanings as those defined in the section headed “Definitions” in the annual report of the Company for 2020 as set out in this announcement. By order of the Board Zhang Hui Joint Company Secretary Jiangsu, the PRC, March 23, 2021 CONTENTS Important Notice ........................................................... 3 Definitions ............................................................... 6 CEO’s Letter .............................................................. 11 Company Profile ........................................................... 15 Summary of the Company’s Business ........................................... 27 Management Discussion and Analysis and Report of the Board ....................... 40 Major Events.............................................................. 112 Changes in Ordinary Shares and Shareholders .................................... 149 Directors, Supervisors, Senior Management and Staff.............................. -
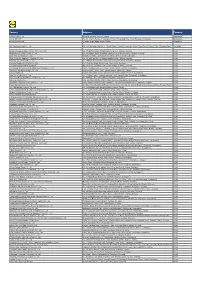
Factory Address Country
Factory Address Country Durable Plastic Ltd. Mulgaon, Kaligonj, Gazipur, Dhaka Bangladesh Lhotse (BD) Ltd. Plot No. 60&61, Sector -3, Karnaphuli Export Processing Zone, North Potenga, Chittagong Bangladesh Bengal Plastics Ltd. Yearpur, Zirabo Bazar, Savar, Dhaka Bangladesh ASF Sporting Goods Co., Ltd. Km 38.5, National Road No. 3, Thlork Village, Chonrok Commune, Korng Pisey District, Konrrg Pisey, Kampong Speu Cambodia Ningbo Zhongyuan Alljoy Fishing Tackle Co., Ltd. No. 416 Binhai Road, Hangzhou Bay New Zone, Ningbo, Zhejiang China Ningbo Energy Power Tools Co., Ltd. No. 50 Dongbei Road, Dongqiao Industrial Zone, Haishu District, Ningbo, Zhejiang China Junhe Pumps Holding Co., Ltd. Wanzhong Villiage, Jishigang Town, Haishu District, Ningbo, Zhejiang China Skybest Electric Appliance (Suzhou) Co., Ltd. No. 18 Hua Hong Street, Suzhou Industrial Park, Suzhou, Jiangsu China Zhejiang Safun Industrial Co., Ltd. No. 7 Mingyuannan Road, Economic Development Zone, Yongkang, Zhejiang China Zhejiang Dingxin Arts&Crafts Co., Ltd. No. 21 Linxian Road, Baishuiyang Town, Linhai, Zhejiang China Zhejiang Natural Outdoor Goods Inc. Xiacao Village, Pingqiao Town, Tiantai County, Taizhou, Zhejiang China Guangdong Xinbao Electrical Appliances Holdings Co., Ltd. South Zhenghe Road, Leliu Town, Shunde District, Foshan, Guangdong China Yangzhou Juli Sports Articles Co., Ltd. Fudong Village, Xiaoji Town, Jiangdu District, Yangzhou, Jiangsu China Eyarn Lighting Ltd. Yaying Gang, Shixi Village, Shishan Town, Nanhai District, Foshan, Guangdong China Lipan Gift & Lighting Co., Ltd. No. 2 Guliao Road 3, Science Industrial Zone, Tangxia Town, Dongguan, Guangdong China Zhan Jiang Kang Nian Rubber Product Co., Ltd. No. 85 Middle Shen Chuan Road, Zhanjiang, Guangdong China Ansen Electronics Co. Ning Tau Administrative District, Qiao Tau Zhen, Dongguan, Guangdong China Changshu Tongrun Auto Accessory Co., Ltd. -

Spatial Distribution Pattern of Minshuku in the Urban Agglomeration of Yangtze River Delta
The Frontiers of Society, Science and Technology ISSN 2616-7433 Vol. 3, Issue 1: 23-35, DOI: 10.25236/FSST.2021.030106 Spatial Distribution Pattern of Minshuku in the Urban Agglomeration of Yangtze River Delta Yuxin Chen, Yuegang Chen Shanghai University, Shanghai 200444, China Abstract: The city cluster in Yangtze River Delta is the core area of China's modernization and economic development. The industry of Bed and Breakfast (B&B) in this area is relatively developed, and the distribution and spatial pattern of Minshuku will also get much attention. Earlier literature tried more to explore the influence of individual characteristics of Minshuku (such as the design style of Minshuku, etc.) on Minshuku. However, the development of Minshuku has a cluster effect, and the distribution of domestic B&Bs is very unbalanced. Analyzing the differences in the distribution of Minshuku and their causes can help the development of the backward areas and maintain the advantages of the developed areas in the industry of Minshuku. This article finds that the distribution of Minshuku is clustered in certain areas by presenting the overall spatial distribution of Minshuku and cultural attractions in Yangtze River Delta and the respective distribution of 27 cities. For example, Minshuku in the central and eastern parts of Yangtze River Delta are more concentrated, so are the scenic spots in these areas. There are also several concentrated Minshuku areas in other parts of Yangtze River Delta, but the number is significantly less than that of the central and eastern regions. Keywords: Minshuku, Yangtze River Delta, Spatial distribution, Concentrated distribution 1. -

Next Tier 3 Suppliers 2020
TIER 3 SUPPLIER SITES - Produced March 2021 SUPPLIER NAME ADDRESS SPINNING KNITTING WEAVING DYEING PRINTING Bangladesh A One Polar Ltd Vulta, Rupgonj, Nrayangonj ✓ ✓ ✓ AA Spinning Mill Ltd Nagar Howla, Sreepur, Gazipur District, Dhaka ✓ Aaron Denim Ltd Sukran, Mirzanagar, Nobinagar, Savar, Dhaka 1347 ✓ ✓ Abanti Colour Tex Ltd S A-646, Shashongaon, Enayetnagar, Fatullah, Narayanganj 1400 ✓ ✓ ✓ ACS Textiles Ltd Tetlabo, Rupgonj, Ward 3, Narayangonj, Dhaka 1400 ✓ ✓ ✓ Adury Knit Composite Ltd Karadi, Shibpur, Narsingdi Narshingdi Dhaka ✓ ✓ ✓ Akij Textile Mills Ltd Golora, Charkhanda, Manikgonj ✓ ✓ ✓ Al Haj Karim Textiles Ltd Kalampur, Dhamrai, Savar, Dhaka 1351 ✓ Alim Knit BD Ltd Nayapara, Kashimpur, Zitar Moor, Gazipur ✓ ✓ ✓ Alliance Knit Composite Ltd 8/118, Pukurpar, Zirabo, Ashulia, Savar, Dhaka-1341 ✓ ✓ ✓ Aman Spinning Mills Ltd Ashulia Highway, Zirabo, Ashulia, Savar, Dhaka ✓ Amantex Limited Boiragi Challa, Shreepur, Gazipur 1740, Dhaka ✓ ✓ ✓ Amber Cotton Mills Ltd Banglabazar, Bahadurpur, Razendrapur, Gazipur, Dhaka ✓ Amber Denim Mills Ltd (Unit 2) Unit 2, Banglabazar, Bahadurpur, Razendrapur, Gazipur, Dhaka ✓ ✓ Anjum Textile Mills Birampur, Madhobdi, Norshingd ✓ ✓ Anwar Silk Mills Ltd 186 Tongi Industrial Area, Tongi, Gazipur ✓ Apex Weaving and Finishing Mills Ltd East Chundora, Shafipur, Kaliakoar, Gazipur 1751 ✓ ✓ ✓ APS Group Kamar Gaon Pubail Road Gazipur ✓ ✓ Argon Denims Ltd Beraider Chala Po Gilaberaid Ps Sripur, Gazipur, 1742, Gazipur ✓ ✓ ✓ Arif Spinning Mill Ltd Mastarbari, Jamirdia, Valuka, Mymensingh ✓ Armada Spinning Mills -

Transmissibility of Hand, Foot, and Mouth Disease in 97 Counties of Jiangsu Province, China, 2015- 2020
Transmissibility of Hand, Foot, and Mouth Disease in 97 Counties of Jiangsu Province, China, 2015- 2020 Wei Zhang Xiamen University Jia Rui Xiamen University Xiaoqing Cheng Jiangsu Provincial Center for Disease Control and Prevention Bin Deng Xiamen University Hesong Zhang Xiamen University Lijing Huang Xiamen University Lexin Zhang Xiamen University Simiao Zuo Xiamen University Junru Li Xiamen University XingCheng Huang Xiamen University Yanhua Su Xiamen University Benhua Zhao Xiamen University Yan Niu Chinese Center for Disease Control and Prevention, Beijing City, People’s Republic of China Hongwei Li Xiamen University Jian-li Hu Jiangsu Provincial Center for Disease Control and Prevention Tianmu Chen ( [email protected] ) Page 1/30 Xiamen University Research Article Keywords: Hand foot mouth disease, Jiangsu Province, model, transmissibility, effective reproduction number Posted Date: July 30th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-752604/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 2/30 Abstract Background: Hand, foot, and mouth disease (HFMD) has been a serious disease burden in the Asia Pacic region represented by China, and the transmission characteristics of HFMD in regions haven’t been clear. This study calculated the transmissibility of HFMD at county levels in Jiangsu Province, China, analyzed the differences of transmissibility and explored the reasons. Methods: We built susceptible-exposed-infectious-asymptomatic-removed (SEIAR) model for seasonal characteristics of HFMD, estimated effective reproduction number (Reff) by tting the incidence of HFMD in 97 counties of Jiangsu Province from 2015 to 2020, compared incidence rate and transmissibility in different counties by non -parametric test, rapid cluster analysis and rank-sum ratio. -

GH 8 2 V Announcement
Geospatial Health 8(2), 2014, pp. 429-435 Spatial distribution and risk factors of influenza in Jiangsu province, China, based on geographical information system Jia-Cheng Zhang1, Wen-Dong Liu2, Qi Liang2, Jian-Li Hu2, Jessie Norris3, Ying Wu2, Chang-Jun Bao2, Fen-Yang Tang2, Peng Huang1, Yang Zhao1, Rong-Bin Yu1, Ming-Hao Zhou2, Hong-Bing Shen1, Feng Chen1, Zhi-Hang Peng1 1Department of Epidemiology and Biostatistics, School of Public Health, Nanjing Medical University, Nanjing, People’s Republic of China; 2Jiangsu Province Center for Disease Control and Prevention, Nanjing, People’s Republic of China; 3National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, People’s Republic of China Abstract. Influenza poses a constant, heavy burden on society. Recent research has focused on ecological factors associated with influenza incidence and has also studied influenza with respect to its geographic spread at different scales. This rese- arch explores the temporal and spatial parameters of influenza and identifies factors influencing its transmission. A spatial autocorrelation analysis, a spatial-temporal cluster analysis and a spatial regression analysis of influenza rates, carried out in Jiangsu province from 2004 to 2011, found that influenza rates to be spatially dependent in 2004, 2005, 2006 and 2008. South-western districts consistently revealed hotspots of high-incidence influenza. The regression analysis indicates that rail- ways, rivers and lakes are important predictive environmental variables for influenza risk. A better understanding of the epi- demic pattern and ecological factors associated with pandemic influenza should benefit public health officials with respect to prevention and controlling measures during future epidemics. -

Contact List of Huatai Agency
Contact List of Huatai Agency www.huataimarine.com Name of Agent: Huatai Beijing Head Office Postal Address.: 14F China Re Building, No.11 Jin Rong Avenue, Xicheng District, Beijing 100033, China ZIP/Postal Code: 100033 City: Beijing Country: China Tel: +86 10 66576588 (general line) Fax: +86 10 66576501 E-mail: [email protected] Persons who may be contacted after office hours Name: Ms. Shan Hong Mobile Phone: +86 13801187853 Direct Line: +86 10 66576566 Name: Ms. He Miao Mobile Phone: +86 13801098591 Direct Line: +86 10 66576587 Name Mr. Wu Dongxu Mobile Phone +86 13811693258 Direct Line +86 10 66576547 Name of Agent: Huatai Dalian Branch covering ports including Dalian, Dandong, Yingkou (Bayuquan), Jinzhou, Huludao, etc. Postal 22nd Floor, Anho Building, No.87, Renmin Road, Zhongshan Address: District, Dalian 116001, China ZIP/Postal Code: 116001 City: Dalian Country: China Tel: +86 411 82535351, 82535357 Fax: +86 411 82535352 E-mail: [email protected] Persons who may be contacted after office hours 1/4 Name: Capt. Lu Tongzhe Mobile Phone: +86 13909851192 Name: Ms. Zhao Bei Mobile Phone: +86 13942086293 Name of Agent: Huatai Tianjin Branch covering ports including Tianjin (Xingang), Huanghua, Caofeidian, Jingtang (Tangshan), Qinhuangdao, etc. Postal Address.: Rm 8501, E8B, Binhai Finance Zone, No. 20 Guang Chang East Road, TEDA, Tianjin, China ZIP/Postal Code: 300457 City: Tianjin Country: China Tel: +86 22 66220722 Fax: +86 22 66220725 E-mail: [email protected] Persons who may be contacted after office hours Name: Mr. Mu Haitao Mobile Phone: +86 13602017813 Direct Line: +86 22 6622 0720 Name: Mr. -

CND Changzhou National Hi-Tech District
CND Changzhou National Hi-tech District Präsentation Pave the way for your success www.invest_in_cnd.cn Inhalt Wie kommen Sie zu CND Changzhou Geschichte CND Fakten CND im Überblick Internationale Kontakte WiekommenSiezuuns Direkte Flugverbindungen von Nordamerika FRA und Europa nach Shanghai und Peking. PEK Insbesondere, direkte Flugverbindung von NKG CZPVG Frankfurt nach Nanjing Lukou International Flughafen. CAN WiekommenSiezuuns Erste Option: Mit dem Zug Von Shanghai zu CND –40 Minuten Von Nanjing zu CND –38 Minuten Zweite Option: Mit dem Auto von Shanghai zu CND –1.5 Stunden Von Nanjing zu CND –1 Stunde Inhalt Wie kommen Sie zu uns Changzhou Geschichte CND Fakten CND im Überblick Internationale Kontakte Die Stadt Changzhou Changzhou in Yangtse-Fluss-Delta Ô Eine historische Stadt mit eine Geschichte von über 2,500 Jahre Ô Gesamte Fläche von 4,385 KM2 Ô Registrierte Einwohner von 3.6 Millionen, und 1.1 Millionen Einwanderer Ô BIP im Jahr 2013: RMB 435 Milliarden Ô Einbezahltes Auslandskapital im Jahr 2013: USD 3.53 Milliarden Ô No. 9 “Best Commercial City in China”, Forbes Changzhou – Strategishes Standort In 2 Stunden Fahrzeit erreichen Sie: Shanghai (Metropoli) Nanjing (Hauptstadt von Jiangsu Province) Hangzhou (Hauptstadt von Zhejiang Province) 2 F a S h t u r z n e d i t e n Inhalt Wie kommen Sie zu uns Changzhou Geschichte CND Fakten CND im Überblick Internationale Kontakte CND 110KM zu Nanjing 1 60K M z u Sh ang hai Changzhou CND Fakten Gegründet im Jahr 1992 Die einzige staatliche Hi‐tech Zone in Changzhou CND Fläche: 439 KM2, -

Polycentricity in the Yangtze River Delta Urban Agglomeration (YRDUA): More Cohesion Or More Disparities?
sustainability Article Polycentricity in the Yangtze River Delta Urban Agglomeration (YRDUA): More Cohesion or More Disparities? Wen Chen 1, Komali Yenneti 2,*, Yehua Dennis Wei 3 , Feng Yuan 1, Jiawei Wu 1 and Jinlong Gao 1 1 Key Laboratory of Watershed Geographic Sciences, Nanjing Institute of Geography and Limnology, Chinese Academy of Sciences, 73 East Beijing Road, Nanjing 210008, China; [email protected] (W.C.); [email protected] (F.Y.); [email protected] (J.W.); [email protected] (J.G.) 2 Faculty of Built Environment, University of New South Wales (UNSW), Sydney, NSW 2052, Australia 3 Department of Geography, University of Utah, Salt Lake City, UT 84112, USA; [email protected] * Correspondence: [email protected] Received: 23 April 2019; Accepted: 28 May 2019; Published: 1 June 2019 Abstract: Urban spatial structure is a critical component of urban planning and development, and among the different urban spatial structure strategies, ‘polycentric mega-city region (PMR)’ has recently received great research and public policy interest in China. However, there is a lack of systematic understanding on the spatiality of PMR from a pluralistic perspective. This study aims to fill this gap by investigating the spatiality of PMR in the Yangtze River Delta Urban Agglomeration (YRDUA) using city-level data on gross domestic product (GDP), population share, and urban income growth for the period 2000–2013. The results reveal that economically, the YRDUA is experiencing greater polycentricity, but in terms of social welfare, the region manifests growing monocentricity. We further find that the triple transition framework (marketization, urbanization, and decentralization) can greatly explain the observed patterns. -

Research on Strategic Countermeasures of Nanjing Port Based on the Analysis of Its Major Cargoes Sisi Yang World Maritime University
World Maritime University The Maritime Commons: Digital Repository of the World Maritime University World Maritime University Dissertations Dissertations 2006 Research on strategic countermeasures of Nanjing port based on the analysis of its major cargoes Sisi Yang World Maritime University Follow this and additional works at: http://commons.wmu.se/all_dissertations Part of the Strategic Management Policy Commons Recommended Citation Yang, Sisi, "Research on strategic countermeasures of Nanjing port based on the analysis of its major cargoes" (2006). World Maritime University Dissertations. 147. http://commons.wmu.se/all_dissertations/147 This Dissertation is brought to you courtesy of Maritime Commons. Open Access items may be downloaded for non-commercial, fair use academic purposes. No items may be hosted on another server or web site without express written permission from the World Maritime University. For more information, please contact [email protected]. WORLD MARITIME UNIVERSITY Shanghai, China RESEARCH ON STRATEGIC COUNTERMEASURES OF NANJING PORT BASED ON THE ANALYSIS OF ITS MAJOR CARGOES By YANG SISI China A research paper submitted to the World Maritime University in partial Fulfillment of the requirements for the award of the degree of MASTER OF SCIENCE (INTERNATIONAL TRANSPORT AND LOGISTICS) 2006 Yang Sisi, 2006 DECLARATION I certify that all the material in this research paper that is not my own work has been identified, and that no material is concluded for which a degree has previously been conferred on me. The contents of this research paper reflect my own personal views, and are not necessarily endorsed by the University. (Signature): (Date): Supervised by Associate Professor Sha Mei Shanghai Maritime University Assessor Professor Mike Ircha Newbrunswick University, Canada Co-Assessor Professor Wang Xuefeng Shanghai Maritime University ii ACKNOWLEDGEMENT This research paper would not been completed without the help and direction of many people.