Identifying TB Hotspots Through Mobile X-Rays in Karachi, Pakistan: Spatial Analysis of Data from an Active Case-Fnding Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Manora Field Notes Naiza Khan
MANORA FIELD NOTES NAIZA KHAN PAVILION OF PAKISTAN CURATED BY ZAHRA KHAN MANORA FIELD NOTES NAIZA KHAN PAVILION OF PAKISTAN CURATED BY ZAHRA KHAN w CONTENTS FOREWORD – Jamal Shah 8 INTRODUCTION – Asma Rashid Khan 10 ESSAYS MANORA FIELD NOTES – Zahra Khan 15 NAIZA KHAN’S ENGAGEMENT WITH MANORA – Iftikhar Dadi 21 HUNDREDS OF BIRDS KILLED – Emilia Terracciano 27 THE TIDE MARKS A SHIFTING BOUNDARY – Aamir R. Mufti 33 MAP-MAKING PROCESS MAP-MAKING: SLOW AND FAST TECHNOLOGIES – Naiza Khan, Patrick Harvey and Arsalan Nasir 44 CONVERSATIONS WITH THE ARTIST – Naiza Khan 56 MANORA FIELD NOTES, PAVILION OF PAKISTAN 73 BIOGRAPHIES & CREDITS 125 bridge to cross the distance between ideas and artistic production, which need to be FOREWORD exchanged between artists around the world. The Ministry of Information and Broadcasting, Government of Pakistan, under its former minister Mr Fawad Chaudhry was very supportive of granting approval for the idea of this undertaking. The Pavilion of Pakistan thus garnered a great deal of attention and support from the art community as well as the entire country. Pakistan’s participation in this prestigious international art event has provided a global audience with an unforgettable introduction to Pakistani art. I congratulate Zahra Khan, for her commitment and hard work, and Naiza Khan, for being the first significant Pakistani artist to represent the country, along with everyone who played a part in this initiative’s success. I particularly thank Asma Rashid Khan, Director of Foundation Art Divvy, for partnering with the project, in addition to all our generous sponsors for their valuable support in the execution of our first-ever national pavilion. -

Population Distribution in Sindh According to Census 2017 (Population of Karachi: Reality Vs Expectation)
Volume 3, Issue 2, February – 2018 International Journal of Innovative Science and Research Technology ISSN No:-2456 –2165 Population Distribution in Sindh According to Census 2017 (Population of Karachi: Reality vs Expectation) Dr. Faiza Mazhar TTS Assistant Professor Geography Department. Government College University Faisalabad, Pakistan Abstract—Sindh is our second largest populated province. Historical Populations Growth of Sindh It has a great role in culture and economy of Pakistan. Karachi the largest city of Pakistan in terms of population Census Year Total Population Urban Population also has a unique impact in development of Pakistan. Now 1951 6,047,748 29.23% according to the current census of 2017 Sindh is again 1961 8,367,065 37.85% standing on second position. Karachi is still on top of the list in Pakistan’s ten most populated cities. Population of 1972 14,155,909 40.44% Karachi has not grown on an expected rate. But it was due 1981 19,028,666 43.31% to many reasons like bad law and order situation, miss management of the Karachi and use of contraceptive 1998 29,991,161 48.75% measures. It would be wrong if it is said that the whole 2017 47,886,051 52.02% census were not conducted in a transparent manner. Source: [2] WWW.EN.WIKIPEDIA.ORG. Keywords—Component; Formatting; Style; Styling; Insert Table 1: Temporal Population Growth of Sindh (Key Words) I. INTRODUCTION According to the latest census of 2017 the total number of population in Sindh is 48.9 million. It is the second most populated province of Pakistan. -
Drivers of Climate Change Vulnerability at Different Scales in Karachi
Drivers of climate change vulnerability at different scales in Karachi Arif Hasan, Arif Pervaiz and Mansoor Raza Working Paper Urban; Climate change Keywords: January 2017 Karachi, Urban, Climate, Adaptation, Vulnerability About the authors Acknowledgements Arif Hasan is an architect/planner in private practice in Karachi, A number of people have contributed to this report. Arif Pervaiz dealing with urban planning and development issues in general played a major role in drafting it and carried out much of the and in Asia and Pakistan in particular. He has been involved research work. Mansoor Raza was responsible for putting with the Orangi Pilot Project (OPP) since 1981. He is also a together the profiles of the four settlements and for carrying founding member of the Urban Resource Centre (URC) in out the interviews and discussions with the local communities. Karachi and has been its chair since its inception in 1989. He was assisted by two young architects, Yohib Ahmed and He has written widely on housing and urban issues in Asia, Nimra Niazi, who mapped and photographed the settlements. including several books published by Oxford University Press Sohail Javaid organised and tabulated the community surveys, and several papers published in Environment and Urbanization. which were carried out by Nur-ulAmin, Nawab Ali, Tarranum He has been a consultant and advisor to many local and foreign Naz and Fahimida Naz. Masood Alam, Director of KMC, Prof. community-based organisations, national and international Noman Ahmed at NED University and Roland D’Sauza of the NGOs, and bilateral and multilateral donor agencies; NGO Shehri willingly shared their views and insights about e-mail: [email protected]. -

Central-Karachi
Central-Karachi 475 476 477 478 479 480 Travelling Stationary Inclass Co- Library Allowance (School Sub Total Furniture S.No District Teshil Union Council School ID School Name Level Gender Material and Curricular Sport Total Budget Laboratory (School Specific (80% Other) 20% supplies Activities Specific Budget) 1 Central Karachi New Karachi Town 1-Kalyana 408130186 GBELS - Elementary Elementary Boys 20,253 4,051 16,202 4,051 4,051 16,202 64,808 16,202 81,010 2 Central Karachi New Karachi Town 4-Ghodhra 408130163 GBLSS - 11-G NEW KARACHI Middle Boys 24,147 4,829 19,318 4,829 4,829 19,318 77,271 19,318 96,589 3 Central Karachi New Karachi Town 4-Ghodhra 408130167 GBLSS - MEHDI Middle Boys 11,758 2,352 9,406 2,352 2,352 9,406 37,625 9,406 47,031 4 Central Karachi New Karachi Town 4-Ghodhra 408130176 GBELS - MATHODIST Elementary Boys 20,492 4,098 12,295 8,197 4,098 16,394 65,576 16,394 81,970 5 Central Karachi New Karachi Town 6-Hakim Ahsan 408130205 GBELS - PIXY DALE 2 Registred as a Seconda Elementary Girls 61,338 12,268 49,070 12,268 12,268 49,070 196,281 49,070 245,351 6 Central Karachi New Karachi Town 9-Khameeso Goth 408130174 GBLSS - KHAMISO GOTH Middle Mixed 6,962 1,392 5,569 1,392 1,392 5,569 22,278 5,569 27,847 7 Central Karachi New Karachi Town 10-Mustafa Colony 408130160 GBLSS - FARZANA Middle Boys 11,678 2,336 9,342 2,336 2,336 9,342 37,369 9,342 46,711 8 Central Karachi New Karachi Town 10-Mustafa Colony 408130166 GBLSS - 5/J Middle Boys 28,064 5,613 16,838 11,226 5,613 22,451 89,804 22,451 112,256 9 Central Karachi New Karachi -

Abbott Laboratories (Pak) Ltd. List of Non CNIC Shareholders Final Dividend for the Year Ended Dec 31, 2015 SNO WARRANT NO FOLIO NAME HOLDING ADDRESS 1 510004 95 MR
Abbott Laboratories (Pak) Ltd. List of non CNIC shareholders Final Dividend For the year ended Dec 31, 2015 SNO WARRANT_NO FOLIO NAME HOLDING ADDRESS 1 510004 95 MR. AKHTER HUSAIN 14 C-182, BLOCK-C NORTH NAZIMABAD KARACHI 2 510007 126 MR. AZIZUL HASAN KHAN 181 FLAT NO. A-31 ALLIANCE PARADISE APARTMENT PHASE-I, II-C/1 NAGAN CHORANGI, NORTH KARACHI KARACHI. 3 510008 131 MR. ABDUL RAZAK HASSAN 53 KISMAT TRADERS THATTAI COMPOUND KARACHI-74000. 4 510009 164 MR. MOHD. RAFIQ 1269 C/O TAJ TRADING CO. O.T. 8/81, KAGZI BAZAR KARACHI. 5 510010 169 MISS NUZHAT 1610 469/2 AZIZABAD FEDERAL 'B' AREA KARACHI 6 510011 223 HUSSAINA YOUSUF ALI 112 NAZRA MANZIL FLAT NO 2 1ST FLOOR, RODRICK STREET SOLDIER BAZAR NO. 2 KARACHI 7 510012 244 MR. ABDUL RASHID 2 NADIM MANZIL LY 8/44 5TH FLOOR, ROOM 37 HAJI ESMAIL ROAD GALI NO 3, NAYABAD KARACHI 8 510015 270 MR. MOHD. SOHAIL 192 FOURTH FLOOR HAJI WALI MOHD BUILDING MACCHI MIANI MARKET ROAD KHARADHAR KARACHI 9 510017 290 MOHD. YOUSUF BARI 1269 KUTCHI GALI NO 1 MARRIOT ROAD KARACHI 10 510019 298 MR. ZAFAR ALAM SIDDIQUI 192 A/192 BLOCK-L NORTH NAZIMABAD KARACHI 11 510020 300 MR. RAHIM 1269 32 JAFRI MANZIL KUTCHI GALI NO 3 JODIA BAZAR KARACHI 12 510021 301 MRS. SURRIYA ZAHEER 1610 A-113 BLOCK NO 2 GULSHAD-E-IQBAL KARACHI 13 510022 320 CH. ABDUL HAQUE 583 C/O MOHD HANIF ABDUL AZIZ HOUSE NO. 265-G, BLOCK-6 EXT. P.E.C.H.S. KARACHI. -

The Early Marriage: Origin of Domestic Violence and Reproductive Health Challenges (With Special Reference to Orangi Town –Karachi)
The Early Marriage: Origin of Domestic Violence and Reproductive Health Challenges (With Special Reference to Orangi Town –Karachi) Nisar Ahmed Nisar* Zubair Latif* Saeeda Khan* Sumera Ishrat** Abstract This traditional practice affecting not only the reproductive health of young girls but it is a major cause of domestic violence as well. This issue has been calling the care of national and international organizations in modern societies, containing Pakistan. Numerous issues which support this belief include poverty, lake of education, the perception of “virginity” of a single girl as key to a family‟s honor, family building (whether joint family or nuclear family), spiritual clarification of being an adult, and short employment opportunities consequence in whole necessity of these girls on their manlike blood relatives. However, the present literature review revealed that there is no comprehensive study on child marriages and its impact on girls‟ reproductive health common in Pakistan. The objectives of the present study were to study the causes of early marriages, domestic violence, and reproductive health problems as well as evaluate socio-economic features on this practice. Orangi Town then the oldest slum settlement of Karachi city was treated as the research universe in the present study while it‟s UC-12 „Mujahidabad‟ and UC-13 „Baloch Goth‟ was the target areas. This research was a qualitative study where the researchers selected the mixed-method strategy for data collection. The snowball sampling and convenience sampling techniques were adopted. A tailor-made Questionnaire was used for data collection. The data was analyzed in tabular form and relevant case studies were also incorporated. -

E Cacy of Home-Based Forti Ed Diet in Rehabilitation Of
Ecacy of Home-Based Fortied Diet in Rehabilitation of Malnourished Children in Resource Restrained Country: An Institution Based Retrospective Study Saba Shahid ( [email protected] ) INDUS Hospital Marvi Mahesar INDUS Hospital Anum Rahim INDUS Hospital Yumna Sadiq INDUS Hospital Research article Keywords: Malnutrition, children, home fortied diet, weight gain, anemia, and rickets Posted Date: August 28th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-60166/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published at BMC Nutrition on August 13th, 2021. See the published version at https://doi.org/10.1186/s40795-021-00455-x. Page 1/16 Abstract Background: Globally, it is estimated that 50 million children under ve are wasted. National nutrition survey-2018 has shown that 23.3% and 45.5% of children are wasted and stunted in Pakistan. Many studies have shown that hospital-based management of malnutrition is not practical due to high cost and iatrogenic infections and currently WHO recommends community-based management of malnutrition with provision of therapeutic food. There is limited evidence of community rehabilitation of malnourished children by using home fortied diet in Pakistan. This study aims to evaluate effectiveness of using energy dense, home fortied diet in weight gain of malnourished children in Karachi, through a retrospective chart review. Methods: A retrospective chart review of pediatric patients (aged 6 month–5 years) seen in Indus Hospital between January 2017 to June 2018 was conducted. A pre-designed data abstraction form was used to record detailed information about demographic characteristics, feeding, anthropometric, micronutrient, and nutritional details at enrollment and on follow-up. -
Law and Order URC
Law and Order URC NEWSCLIPPINGS JANUARY TO JUNE 2019 LAW & ORDERS Urban Resource Centre A-2, 2nd floor, Westland Trade Centre, Block 7&8, C-5, Shaheed-e-Millat Road, Karachi. Tel: 021-4559317, Fax: 021-4387692, Email: [email protected], Website: www.urckarachi.org Facebook: www.facebook.com/URCKHI Twitter: https://twitter.com/urc_karachi 1 Law and Order URC Targeted killing: KMC employee shot dead in Hussainabad Unidentified assailants shot and killed an employee of the Karachi Metropolitan Corporation (KMC) at Hussainabad locality of Federal B Area in Central district on Monday. The deceased was struck by seven bullets in different parts of the body. Nine bullet shells of a 9mm pistol were recovered from the scene of the crime. According to police, the deceased was called to the location through a phone call. They said the late KMC employee was on his motorcycle waiting for someone. Two unidentified men killed him by opening fire at him at Hussainabad, near Okhai Memon Masjid, in the limits of Azizabad police station. The deceased, identified as Shakeel Ahmed, aged 35, son of Shafiq Ahmed, was shifted to Abbasi Shaheed Hospital for medico-legal formalities. He was a resident of house no. L-72 Sector 5C 4, North Karachi, and worked as a clerk in KMC‘s engineering department. Rangers and police officials reached the scene after receiving information of the incident. They recovered nine bullet shells of a 9mm pistol and have begun investigating the incident. According to Azizabad DSP Shaukat Raza, someone had phoned and summoned the deceased to Hussainabad, near Okhai Memon Masjid. -

List of Unclaimed Dividends and Shares
Ferozsons Laboratories Limited List of Unclaimed Dividend & Bonus Amount of No. of Unclaimed S.No Folio Name Address CNIC Unclaimed Dividend Shares (Rupees) 1 0005 Mr. Abdul Hamid Khan C/O Ferozsons Limited 60 The Mall, Lahore. 00000-0000000-0 499 117,337 2 0011 Mr. Mohammad Javid Khan, Pak International Printers 118 - G. T. Road Lahore. 00000-0000000-0 8 3,806 3 0012 Begum Abdul Majid Khan C/O Pakistan International Printers,118-G.T.Road, Lahore. 00000-0000000-0 718 308,023 4 0017 Miss Kaukab Sadiq 64 / E - 1, Gulberg - III Lahore. 00000-0000000-0 1724 301,856 5 0019 Imtiaz Begum Sahiba 64 / E - 1, Gulberg - III Lahore. 00000-0000000-0 143 24,882 6 0028 Mr. Abdul Razzaq H.No.815,St.64, G-9/4 Islamabad 00000-0000000-0 902 156,010 7 0035 Mr. Shams-ul-Hassan Khawaja Pharmaceutical Section Ministry of Health Al-Riyadh 00000-0000000-0 236 40,960 8 0043 Mrs. Shujaat Parveen Vill: & P. O.Toru Mardan. 00000-0000000-0 1056 1,292,201 9 0050 Mrs. Khawar Kazi L - 102, D. H. A. Lahore Cantt. 35201-8757810-4 0 2,029 10 0059 Mr. Tahir Ali Khan H.No.280,St.38, G-9/1, Islamabad 00000-0000000-0 4423 759,766 11 0060 Mr. Abdul Qadir Khan Retd.Veterinary Doctor Kacha Gojra Faisalabad. 00000-0000000-0 1874 323,753 12 0063 Mr. Said Ahmed Shah House # 64 Biket Ganj Street Mardan. 00000-0000000-0 210 318,085 13 0065 Dr. Mrs. Farrakh Iqbal A-572 Block 5, Gulshan-e-Iqbal, Karachi 75300 42201-5619562-0 0 11,332 14 0066 Mr. -

LIST of POLLING STATIONS for a CONSTITUENCY of Election to the Provincial Assembly of the Sindh PS-116 KARACHI WEST-V
ELECTION COMMISSION OF PAKISTAN FORM-28 [see rule 50] LIST OF POLLING STATIONS FOR A CONSTITUENCY OF Election to the Provincial Assembly of the Sindh PS-116 KARACHI WEST-V Number of voters as igned to In Case of Rural Areas In Case of Urban Areas Number of polling booths S. No. of voters polling station on the electoral No. and Name of Polling Sr. No. roll in case Station Census Block Census Block Name of Electoral Areas Name of Electoral Areas electoral area is Male Female Total Male Female Total Code Code bifurcated 1 2 3 4 5 6 7 8 9 10 11 12 13 Islam Nagar 408010101 - 0 423 207 630 1 Babul Ilam Sec School Islam Nagar 408010102 - - 0 356 0 356 2 1 3 Islam Nagar 408010108 -- 0 302 0 302 1 Total - -- 1081 207 1288 2 1 3 Islam Nagar 408010103 - 0 284 0 284 Islam Nagar 408010104 - - 0 234 0 234 Islam Nagar 408010105 0 117 0 117 2 Babul Ilam Sec School 3 0 3 Islam Nagar 408010106 0 211 0 211 Islam Nagar 408010107 -- 0 461 0 461 Islam Nagar 408010109 -- 0 201 0 201 2 Total - - 1508 0 1508 3 0 3 Islam Nagar 408010102 - - 0 0 243 243 Islam Nagar 408010103 - 0 0 170 170 Islam Nagar 408010104 - 0 0 152 152 Islam Nagar 408010105 - - 0 0 72 72 3 Babul Ilam Sec School 0 - 3 3 Islam Nagar 408010106 - 0 0 126 126 Islam Nagar 408010107 - 0 0 281 281 Islam Nagar 408010108 -- 0 0 116 116 Islam Nagar 408010109 - - 0 0 156 156 3 Total - - - 0 1316 1316 0 3 3 Abidabad BI-A Islam 408010201 - - 0 330 197 527 Nagar Abidabad BI-A Islam 4 GBPS Siddiqui, Abidabad 408010202 - 0 401 207 608 2 1 3 Nagar Abidabad BI-A Islam 408010203 - 0 101 68 169 Nagar 4 Total - - - 832 472 1304 2 1 3 Number of voters assigned to Number of polling booths In Case of Rural Areas In Case of Urban Areas 5. -
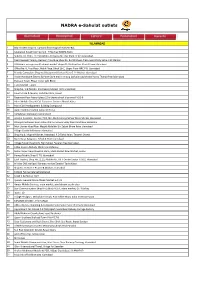
Active Franchise List ~ NADRA.Xlsx
NADRA e-Sahulat outlets ISLAMABAD 1 Bilal traders shop no 7 ground floor mughal market I‐8/1 2 Islamabad Karachi company G ‐ 9 Markaz NADRA Kisok 3 Subicca Inc. H.No. 112 Street No 70 Opposite Filter Plant G 9/3 Islamabad. 4 Pearl Iceream,Yammy Icecream franchise,Shop No. B‐2,Shaheen Plaza,near Utility Sotre,I‐10 Markaz 5 Al Rehmat enterprises Al rehmat market shops 01‐03 street no 4 koral town Islamabad 6 Office No. 6, First Floor, Malik Plaza, Block 16‐C, Upper Floor NRC F‐8, Islamabad 7 Friends Computers Shop no 9 basement Farhan Plaza G‐11 Markaz Islamabad 8 Arslan Hardware Electric & Paint Store machine stop Darkala road chowk Harno Thanda Pani Islamabad 9 Pakistan Town, Phase‐I near Lohi Bheer 10 Tariq Market F‐10/2. 11 Shop No. 1‐B Plot No. 2/A Pakeza Market I‐8/4 Islamabad 12 Hamza Card & Mobile, Saifullah Plaza, Rawat 13 Basement floor hajveri plaza 22‐b chaina chock blue area F‐6,G‐6 14 Adeel Mobile Shop & Call Customer Services Bharak Kahu 15 Main CDA Headquarters Building Compound 16 Aamir Communication Jabba UC Tarlai 17 Al‐Rehman Stationary Golra Sharif 18 Arsalan Customer Service, PCO, Nei Abadi Korang Sohan Warsi Market Islamabad. 19 Dhanyal Customer Near Police Station Service Simly Dam Road Near Barakahu. 20 Moh Usman Abad Near Masjid Abdullah Bin Zubair Bhara Kaho Islamabad 21 Village Chatta Bakhtawar Islamabad. 22 Shop No.8, Mughal Market, Irfanabad, P.O Tarlai Kalan, Taramri Chowk. 23 Main Bazar Sang Jani, Tehsil & Distt Islamabad 24 Village Farash Near Girls High School Federal Area Islamabad. -

Informal Land Controls, a Case of Karachi-Pakistan
Informal Land Controls, A Case of Karachi-Pakistan. This Thesis is Submitted in Fulfilment of the Requirements for the Degree of Doctor of Philosophy Saeed Ud Din Ahmed School of Geography and Planning, Cardiff University June 2016 DECLARATION This work has not been submitted in substance for any other degree or award at this or any other university or place of learning, nor is being submitted concurrently in candidature for any degree or other award. Signed ………………………………………………………………………………… (candidate) Date ………………………… i | P a g e STATEMENT 1 This thesis is being submitted in partial fulfillment of the requirements for the degree of …………………………(insert MCh, MD, MPhil, PhD etc, as appropriate) Signed ………………………………………………………………………..………… (candidate) Date ………………………… STATEMENT 2 This thesis is the result of my own independent work/investigation, except where otherwise stated. Other sources are acknowledged by explicit references. The views expressed are my own. Signed …………………………………………………………….…………………… (candidate) Date ………………………… STATEMENT 3 I hereby give consent for my thesis, if accepted, to be available for photocopying and for inter- library loan, and for the title and summary to be made available to outside organisations. Signed ……………………………………………………………………………… (candidate) Date ………………………… STATEMENT 4: PREVIOUSLY APPROVED BAR ON ACCESS I hereby give consent for my thesis, if accepted, to be available for photocopying and for inter- library loans after expiry of a bar on access previously approved by the Academic Standards & Quality Committee. Signed …………………………………………………….……………………… (candidate) Date ………………………… ii | P a g e iii | P a g e Acknowledgement The fruition of this thesis, theoretically a solitary contribution, is indebted to many individuals and institutions for their kind contributions, guidance and support. NED University of Engineering and Technology, my alma mater and employer, for financing this study.