A Layout Design Decision-Support Framework and Concept Demonstrator for Rural Hospitals Using Mixed Methods
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2014-2018 SRP Faculty and WUSM Med Students (488) 2014-2018 SRP List WUSM OMSR July 2018
2014-2018 SRP Faculty and WUSM Med Students (488) 2014-2018 SRP List WUSM OMSR July 2018 SRP Faculty SRP Faculty SRP SRP Faculty Faculty Research Interest Student LN Student FN SRP Research Project SRP FIHTM LN FN Faculty Division year Dept Abendschein Dana Medicine Cardiology Role of Coagulation Proteases & Karlow Nicholas Targeting the Antithrombotic 2015 Inflammatory Molecules in Vascular Effect of Human Apyrase Remodeling Directly to the Site of Arterial Thrombosis Abraham Christopher Radiation Clinical Brain metastases, stereotactic Bhat Nisha Predictors of Discovery of 2018 Oncology Divisions radiosurgery, and palliative care. Previously Undetected Brain Metastases at the Time of Gamma Knife Radiosurgery Akinwande Olaguoke Radiology Interventional oncology, bariatric Atagu Norman Construction of a predictive 2018 embolization. model for future liver remnant hypertrophy after portal vein embolization Anadkat Milan Medicine Dermatolog Dermatology; Blood Pokala Naveen Clinical Findings in Cutaneous 2015 y Graft vs Host Disease Ances Beau Neurology Developing Structural and Functional Deliz Juan Personality and Resting-State 2016 Neuroimaging Biomarkers of Normal Gonzalez Functional Connectivity in the Aging and Neurodegeneration; Setting of Alzheimer's Disease Therapeutic Interventions to Improve Neurocognitive Deficits Associated with Neurodegenerative Disorders Anokhin Andrey Psychiatry Substance Abuse; Genetic & Mulvey Bernard Neurocognition, Genetics, and 2014 Neurobiological Bases of Human Adolescent Substance Abuse Individual -

Writing Contest Winners Reasons Why Doctors Write Why We Need
ALSO INSIDE: Writing Contest Winners Reasons Why 7 Doctors Write Why We Need the Arts in Medicine MINNESOTA MEDICAL ASSOCIATION JULY 2011 MINNESOTA MEDICAL ASSOCIATION 17 22 JULY 2011 TABLE OF CONTENTS COVER STORY Medical Imaging 14 Winners of our photo 47 contest p.30 PULSE 14 A Life in Pictures | By Suzy Frisch Taking photos is the best medicine for pediatric surgeon Roberta 37 Sonnino. FEATURE 16 The Body Electric | By Kim Kiser Medical students create an online showcase for their creative works. Medical Musings 17 Visual Cues | By Carmen Peota A Minneapolis Institute of Arts program aids people with memory Results of our eighth annual writing contest loss. Student Winners 18 A New Leaf | By Lisa Harden Rehab patients express themselves through clay. 38 Unspoken Words | By Erica Warnock 40 The River | By Aaron Crosby 20 Study Break | By Kim Kiser Medical students use Art of Medicine awards to explore Physician Winner their creative side. 43 Hospice | By William Shores, M.D. 22 Uniform Design | By Carmen Peota Scrubs become high fashion. Physician Honorable Mention 44 Bethany, House of God PERSPECTIVE | By Jamie Santilli, M.D. 45 I Believe, You Believe 47 Seven Reasons Why Doctors Write | By Tony Miksanek, M.D. | By Marilyn Aschoff Mellor, M.D. Physicians write for the same reasons that nonphysicians do, 46 Infertility 628.2 | By Carrie Link, M.D. plus some special ones. 8 | Minnesota Medicine • July 2011 MMA NEWS minnesota MEDICINE 25 State Launches Time Out Campaign 2011 MMA Officers Owner and Publisher President Minnesota Medical Association Patricia J. Lindholm, M.D. -

Covid-19 Sentinel Hospital Surveillance for Hcws Report
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 37, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 12 September 2020 on the DATCOV platform. HIGHLIGHTS As of 12 September 2020, 2 811 (4.2%) of the 66 920 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 253 facilities (87 public-sector and 166 private-sector) in all nine provinces of South Africa. Among 885/2811 (31.5%) HCWs with available data on type of work, 430/885 (50.1%) were nurses, 165/885 (19.2%) were categorized as other HCWs, 119/885 (13.4%) porters or administrators, 65/885 (7.6%) allied HCWs, 56/885 (6.5%) doctors, 16/885 (1.9%) paramedics, and 7/885 (0.8%) laboratory scientists. There was an increase of 125 new HCW admissions since week 36. There were 407 (14.5%) and 2404 (85.5%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (869, 30.9%), KwaZulu-Natal (697, 24.8%), Eastern Cape (490, 17.3%) and Western Cape (290, 10.3%). The median age of COVID-19 HCW admissions was 49 years, there were 556 (19.8%) admissions in HCWs aged 60 years and older. A total of 2000 (71.2%) were female. -

Covid-19 Sentinel Hospital Surveillance for Hcws Report
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 34, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 22 August 2020 on the DATCOV platform. HIGHLIGHTS As of 22 August 2020, 2 481 (4.2%) of the 58 594 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 245 facilities (71 public-sector and 174 private-sector) in all nine provinces of South Africa. Among 701/2481 (28.3%) HCWs with available data on type of work, 335/701 (47.8%) were nurses, 171/701 (24.4%) were categorized as other HCWs, 88/701 (12.5%) porters or administrators, 47/701 (6.7%) allied HCWs, 37/701 (5.3%) doctors, 16/701 (2.3%) paramedics, and 7/701 (1.0%) laboratory scientists. There was an increase of 261 new HCW admissions since week 33. Notably, 185/261 HCW admissions were retrospectively captured into the DATCOV system and are not real-time admissions from the last week. There were 299 (12.1%) and 2182 (87.9%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (778, 31.4%), KwaZulu-Natal (606, 24.4%), Eastern Cape (395, 15.9%) and Western Cape (276, 11.1%). The median age of COVID-19 HCW admissions was 49 years, there were 440 (17.7%) admissions in HCWs aged 60 years and older. -

Covid-19 Sentinel Hospital Surveillance for Hcws Report
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 35, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 29 August 2020 on the DATCOV platform. HIGHLIGHTS As of 29 August 2020, 2 529 (4.1%) of the 61 599 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 248 facilities (74 public-sector and 174 private-sector) in all nine provinces of South Africa. Among 751/2529 (29.7%) HCWs with available data on type of work, 368/751 (49.0%) were nurses, 169/751 (22.5%) were categorized as other HCWs, 95/751 (12.6%) porters or administrators, 50/751 (6.7%) allied HCWs, 47/751 (6.3%) doctors, 15/751 (2.0%) paramedics, and 7/751 (0.9%) laboratory scientists. There was an increase of 48 new HCW admissions since week 34. There were 321 (12.1%) and 2208 (87.3%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (787, 31.1%), followed by KwaZulu-Natal (612, 24.2%), Eastern Cape (414, 16.4%) and Western Cape (278, 11.0%). The median age of COVID-19 HCW admissions was 49 years, there were 447 (17.7%) admissions in HCWs aged 60 years and older. A total of 1808 (71.5%) were female. -

Health Professions Act: List of Approved Facilities for the Purposes
STAATSKOERANT, 16 OKTOBER 2013 No. 36936 39 No. 791 16 October 2013 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY MEDICAL PRACTITIONERS IN THE YEAR 2014 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following approved facilities for purposes of the profession of medicine. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo Khotsong Hospital* Madzikane kaZulu Hospital ** Umzimvubu Cluster Mt Ayliff Hospital** Taylor Bequest Hospital* (Matatiele) Amathole Bhisho CHH Cathcart Hospital * Amahlathi/Buffalo City Cecilia Makiwane Hospital Cluster Dimbaza CHC Duncan Village Day Hospital Empilweni Gompo CHC Fort Grey TB Hospital Frere Hospital Grey Hospital * Komga Hospital Nkqubela TB Hospital Nompumelelo Hospital* SS Gida Hospital* Stutterheim FPA Hospital* Mnquma Sub-District Butterworth Hospital* Nqgamakwe CHC* Nkonkobe Sub-District Adelaide FPA Hospital Tower Hospital* Victoria Hospital * Mbashe /KSD District Elliotdale CHC* Idutywa CHC* Madwaleni Hospital* Chris Hani All Saints Hospital** Engcobo/IntsikaYethu Cofimvaba Hospital** Martjie Venter FPA Hospital This gazette is also available free online at www.gpwonline.co.za 40 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 Sub-District Mjanyana Hospital * InxubaYethembaSub-Cradock Hospital** Wilhelm Stahl Hospital** District Inkwanca -

39070 7-8 Health
Government Gazette Staatskoerant REPUBLIC OF SOUTH AFRICA REPUBLIEK VAN SUID AFRIKA Regulation Gazette No. 10177 Regulasiekoerant August Vol. 602 6 2015 No. 39070 Augustus PART 1 OF 2 ISSN 1682-5843 N.B. The Government Printing Works will 39070 not be held responsible for the quality of “Hard Copies” or “Electronic Files” submitted for publication purposes 9 771682 584003 AIDS HELPLINE: 0800-0123-22 Prevention is the cure 2 No. 39070 GOVERNMENT GAZETTE, 6 AUGUST 2015 IMPORTANT I nfarmai,o-w from Government Printing Works Dear Valued Customers, Government Printing Works has implemented rules for completing and submitting the electronic Adobe Forms when you, the customer, submits your notice request. Please take note of these guidelines when completing your form. GPW Business Rules 1. No hand written notices will be accepted for processing, this includes Adobe ,-..,. forms which have been completed by hand. 2. Notices can only be submitted in Adobe electronic form format to the email submission address submit.egazette @gpw.gov.za. This means that any notice submissions not on an Adobe electronic form that are submitted to this mailbox will be rejected. National or Provincial gazette notices, where the Z95 or Z95Prov must be an Adobe form but the notice content (body) will be an attachment. 3. Notices brought into GPW by "walk -in" customers on electronic media can only be submitted in Adobe electronic form format. This means that any notice submissions not on an Adobe electronic form that are submitted by the customer on electronic media will be rejected. National or Provincial gazette notices, where the Z95 or Z95Prov must be an Adobe form but the notice content (body) will be an attachment. -

Cohsasa News Sept 06
CohsasaThe Newsletter The Council for Health Service Accreditation of Southern Africa TECHNOLOGY UPDATE OCTOBER 2006 New information system is a treasure map COHSASA – in partnership with Xylaco Software – has developed a unique application, which will provide a 360-degree view of strengths, weaknesses and Ten South African urgent improvements needed in health facilities enrolled in COHSASA’s quality hospices accredited improvement and accreditation programmes. Ten hospices in the country, all members of the Hospice Palliative Care Association of Examining 37 areas of operation and measuring both clinical and non- South Africa, have been accredited clinical performance indicators, the new database, migrated from for two years, having met the COHSASA’s multiple legacy databases, will be able to provide professional quality standards clients with quick and easy access to a treasure trove of of COHSASA. information about their hospitals. A total of 47 members of Want to know how your hospital shapes up with regard to the Association entered the infection control? Get your access code, connect on-line and accreditation programme. the COHSASA information system will tell you exactly how Grahamstown Hospice you stand against professional standards, how various was the first to be departments associated with infection control are managing, accredited, followed by what criteria they are meeting and urgent deficiencies that nine others, which have met must be promptly addressed. stringent requirements for Moreover, if you are in the COHSASA Facilitated REWARDING QUALITY: Chairman of COHSASA, the provision of palliative care. Accreditation Programme, you can monitor staff progress and Albert Ramukumba, hands over the accreditation award to the Nursing Services Director of St Francis They were rated on standards pinpoint the bottlenecks and delays. -

COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized Hcws
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 36, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 5 September 2020 on the DATCOV platform. HIGHLIGHTS As of 5 September 2020, 2 686 (4.2%) of the 64 705 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 247 facilities (81 public-sector and 166 private-sector) in all nine provinces of South Africa. Among 801/2686 (29.8%) HCWs with available data on type of work, 391/801 (48.8%) were nurses, 168/801 (21.0%) were categorized as other HCWs, 111/801 (13.9%) porters or administrators, 57/801 (7.1%) allied HCWs, 52/801 (6.5%) doctors, 15/801 (1.9%) paramedics, and 7/801 (0.9%) laboratory scientists. There was an increase of 157 new HCW admissions since week 35. There were 360 (13.4%) and 2326 (86.6%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (834, 31.1%), KwaZulu-Natal (656, 24.4%), Eastern Cape (465, 17.3%) and Western Cape (281, 10.5%). The median age of COVID-19 HCW admissions was 49 years, there were 482 (17.9%) admissions in HCWs aged 60 years and older. A total of 1912 (71.2%) were female. -

ISARIC (International Severe Acute Respiratory and Emerging Infections Consortium)
medRxiv preprint doi: https://doi.org/10.1101/2020.07.17.20155218; this version posted July 14, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-ND 4.0 International license . ISARIC Clinical Data Report issued: 14 July 2021 International Severe Acute Respiratory and emerging Infections Consortium ISARIC Clinical Characterisation Group*^ *group members, participating institutions and funders are listed at end of report and at https://isaric.org/research/covid-19-clinical- research-resources/covid-19-data-management-hosting/covid-19-clinical-data-contributors-list/ ^Correspondence to: [email protected] 1 1 ISARIC, Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK Abstract ISARIC (International Severe Acute Respiratory and emerging Infections Consortium) partnerships and outbreak preparedness initiatives enabled the rapid launch of standardised clinical data collection on COVID-19 in Jan 2020. Extensive global uptake of this resource has resulted in a large, standardised collection of comprehensive clinical data from hundreds of sites across dozens of countries. Data are analysed regularly and reported publicly to inform patient care and public health response. This report, our 15th report, is a part of a series and includes the results of data analysis for data captured before 26 May 2021. The report marks a significant milestone – the submission of clinical data from over half a million individuals hospitalised with COVID-19. We thank all of the data contributors for their ongoing support. -

Covid-19 Sentinel Hospital Surveillance Update South Africa Week 32 2020
COVID-19 SENTINEL HOSPITAL SURVEILLANCE UPDATE SOUTH AFRICA WEEK 32 2020 OVERVIEW This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all provinces. The report is based on data collected from 5 March to 8 August 2020. HIGHLIGHTS ∙ As of 8 August, 49218 COVID-19 admissions were reported from 380 facilities (144 public-sector and 236 private-sector) in all nine provinces of South Africa. There was an increase of 5177 new admissions since the last report, and 40 additional hospitals (35 public-sector and 5 private-sector) reporting COVID-19 admissions. There were 15503 (32%) and 33625 (68%) admissions reported in public and private sector respectively. The majority of COVID-19 admissions were reported from four provinces, 15782 (32%) in Western Cape, 14122 (29%) in Gauteng, 7824 (16%) in KwaZulu-Natal and 4306 (9%) in Eastern Cape. Admissions in the Western Cape, Eastern Cape and Gauteng have decreased and there are indications of slowing of the rate of increase in admissions in the other provinces over the past three weeks. ∙ ∙ Of the 49128 admissions, 6723 (14%) patients were in hospital at the time of this report, 34667 (71%) patients were discharged alive or transferred out and 7655 (16%) patients had died. There were 1028 additional deaths since the last report. ∙ ∙ Of the 41841 COVID-19 patients who had recorded in-hospital outcome (died and discharged), the case fatality ratio (CFR) was 18%. On multivariable analysis, factors associated with in-hospital mortality were older age groups; male sex; Black African and Coloured race; admission in the public sector; and having comorbid hypertension, diabetes, chronic cardiac disease, chronic renal disease, malignancy, HIV, current tuberculosis alone or both current and past tuberculosis, and obesity. -
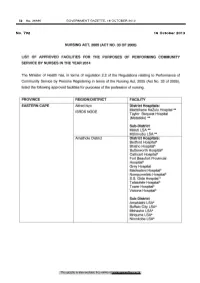
Nursing Act: List of Approved Facilities for the Purposes of Performing Community Service by Nurses in the Year 2014
52 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 No. 792 16 October 2013 NURSING ACT, 2005 (ACT NO. 33 OF 2005) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY NURSES IN THE YEAR 2014 The Minister of Health has, in terms of regulation 2.2 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Nursing Act, 2005 (Act No. 33 of 2005), listed the following approved facilities for purposes of the profession of nursing. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo District Hospitals: Madzikane Ka Zulu Hospital** ISRDS NODE Taylor Bequest Hospital (Matatiele) ** Sub-District Maluti LSA** Mzimvubu LSA*" Amathole District District Hospitals: Bedford Hospital* Bhisho Hospital* Butterworth Hospital* Cathcart Hospital* Fort Beaufort Provincial Hospital* Grey Hospital Madwaleni Hospital* Nompumelelo Hospital* S.S. Gida Hospital * Tafalofefe Hospital* Tower Hospital* Victoria Hospital* Sub-District Amahiathi LSA* Buffalo City LSA* Mbhashe LSA* Mnquma LSA* Nkonkobe LSA* This gazette is also available free online at www.gpwonline.co.za STAATSKOERANT, 16 OKTOBER 2013 No. 36936 53 Cacadu District District Hospitals Andries Vosloo Hospital* Humansdorp Hospital* Midlands Hospital* Port Alfred Hospital* Settlers Hospital* Sub-Districts Camdeboo LSA* Kouga LSA* Makana LSA* Chris Hani District District Hospitals: All Saints Hospital ** ISRDS NODE Cala Hospital** Cofimvaba Hospital ** Cradock Hospital** Dodrecht Hospital Elliot Hospital ** Glen Grey Hospital ** Hewu