Covid-19 Sentinel Hospital Surveillance Update Highlights Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Public Service Vacancy Circular Publication No 36
PUBLIC SERVICE VACANCY CIRCULAR PUBLICATION NO 36 OF 2018 DATE ISSUED: 07 SEPTEMBER 2018 1. Introduction 1.1 This Circular is, except during December, published on a weekly basis and contains the advertisements of vacant posts and jobs in Public Service departments. 1.2 Although the Circular is issued by the Department of Public Service and Administration, the Department is not responsible for the content of the advertisements. Enquiries about an advertisement must be addressed to the relevant advertising department. 2. Directions to candidates 2.1 Applications on form Z83 with full particulars of the applicants’ training, qualifications, competencies, knowledge and experience (on a separate sheet if necessary or a CV) must be forwarded to the department in which the vacancy/vacancies exist(s). 2.2 Applicants must indicate the reference number of the vacancy in their applications. 2.3 Applicants requiring additional information regarding an advertised post must direct their enquiries to the department where the vacancy exists. The Department of Public Service and Administration must not be approached for such information. 2.4 It must be ensured that applications reach the relevant advertising departments on or before the applicable closing dates. 3. Directions to departments 3.1 The contents of this Circular must be brought to the attention of all employees. 3.2 It must be ensured that employees declared in excess are informed of the advertised vacancies. Potential candidates from the excess group must be assisted in applying timeously for vacancies and attending where applicable, interviews. 3.3 Where vacancies have been identified to promote representativeness, the provisions of sections 15 (affirmative action measures) and 20 (employment equity plan) of the Employment Equity Act, 1998 should be applied. -

13 July 2018 (Advert Is Valid for a Period of Six (6) Months up to 18 January 2019)
CLOSING DATE: 13 JULY 2018 (ADVERT IS VALID FOR A PERIOD OF SIX (6) MONTHS UP TO 18 JANUARY 2019) NOTE: Applications must be posted on the Z83 Form accompanied by copies of Qualification(s),Identity document (certified within the past three months), Proof of registration, proof of citizenship if not RSA citizen, a comprehensive CV, indicating three reference persons: Name and Contact Numbers, A relationship with reference, Reference checks will be done on nominated candidate(s). Note: Failure to submit these copies will result in the application not being considered. Please do not send any original certificates, diplomas or testimonials. Applicants must note that further Personnel Suitability checks will be conducted on short-listed and that their appointment is subject to the outcome of these checks include security clearance, security vetting, qualification verification and criminal checking. Note that correspondence will only be conducted with the short- listed candidates. If you have not been contacted by the department of Health within three (3) months of the closing date of the advertisement, please accept that your application was unsuccessful. We thank all applicants for their interest. All shortlisted candidates for SMS posts will be subjected to a technical exercise that intends to test relevant technical elements of the job, the logistics of which will be communicated by department. Following the interview and the technical exercise, the selection panel will recommend candidates to attend a generic managerial competency assessment (in compliance with the DPSA Directive on the implementation of competency based assessments). The competency assessment will be testing generic managerial competencies using the mandated DPSA SMS Competency assessments tools. -

The Perceptions of General Practitioners on National Health Insurance in Chris Hani District, Eastern Cape, South Africa
South African Family Practice 2019; 61(3):102–108 https://doi.org/10.1080/20786190.2019.1596665 S Afr Fam Pract ISSN 2078-6190 EISSN 2078-6204 Open Access article distributed under the terms of the © 2019 The Authors Creative Commons License [CC BY-NC 4.0] http://creativecommons.org/licenses/by-nc/4.0 RESEARCH The perceptions of general practitioners on National Health Insurance in Chris Hani district, Eastern Cape, South Africa Mthetheleli Mbongeni Gaqavu and Robert Mash* Division of Family Medicine and Primary Care, Stellenbosch University, South Africa *Corresponding author, email: [email protected] Background: National Health Insurance (NHI) intends to provide universal health coverage to all South Africans, with equity and quality as its tenets. The participation of private general practitioners (GPs) in NHI is essential. The aim was to explore perceptions of GPs on NHI in Chris Hani district, Eastern Cape, South Africa. Methods: A descriptive phenomenological qualitative study using semi-structured individual interviews of 12 GPs from six municipalities was undertaken. Data analysis used the framework method assisted by Atlas.ti software. Results: GPs in Chris Hani district felt that NHI would improve health and benefit society and be of particular benefit to poor and rural people as it will improve access to healthcare. Lack of governmental administrative capacity and a human resource plan were seen as barriers to implementation. They believed that NHI would benefit them through a single purchaser system and support more comprehensive care. GPs were concerned about a lack of information on primary care packages, accreditation, remuneration and patient allocation. -

Public Service Vacancy Circular Publication No 21
PUBLIC SERVICE VACANCY CIRCULAR PUBLICATION NO 21 OF 2019 DATE ISSUED: 14 JUNE 2019 1. Introduction 1.1 This Circular is, except during December, published on a weekly basis and contains the advertisements of vacant posts and jobs in Public Service departments. 1.2 Although the Circular is issued by the Department of Public Service and Administration, the Department is not responsible for the content of the advertisements. Enquiries about an advertisement must be addressed to the relevant advertising department. 2. Directions to candidates 2.1 Applications on form Z83 with full particulars of the applicants’ training, qualifications, competencies, knowledge and experience (on a separate sheet if necessary or a CV) must be forwarded to the department in which the vacancy/vacancies exist(s). 2.2 Applicants must indicate the reference number of the vacancy in their applications. 2.3 Applicants requiring additional information regarding an advertised post must direct their enquiries to the department where the vacancy exists. The Department of Public Service and Administration must not be approached for such information. 2.4 It must be ensured that applications reach the relevant advertising departments on or before the applicable closing dates. 3. Directions to departments 3.1 The contents of this Circular must be brought to the attention of all employees. 3.2 It must be ensured that employees declared in excess are informed of the advertised vacancies. Potential candidates from the excess group must be assisted in applying timeously for vacancies and attending where applicable, interviews. 3.3 Where vacancies have been identified to promote representativeness, the provisions of sections 15 (affirmative action measures) and 20 (employment equity plan) of the Employment Equity Act, 1998 should be applied. -
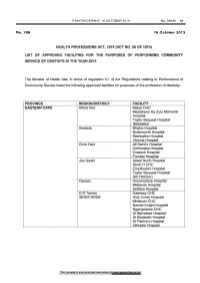
Health Professions Act: List of Approved Facilities for the Purposes of Performing Community Service by Dentists in the Year
STAATSKOERANT, 16 OKTOBER 2013 No. 36936 13 No. 788 16 October 2013 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY DENTISTS IN THE YEAR 2014 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service listed the following approved facilities for purposes of the profession of dentistry. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo Maluti CHC Madzikane Ka Zulu Memorial Hospital Taylor Bequest Hospital (Matatiele) Amato le Bhisho Hospital Butterworth Hospital Madwaleni Hospital Victoria Hospital Chris Hani All Saint's Hospital Cofimvaba Hospital Cradock Hospital Frontier Hospital Joe Gqabi Aliwal North Hospital Block H CHC Empilisweni Hospital Taylor Bequest Hospital (Mt Fletcher) Cacadu Humansdorp Hospital Midlands Hospital Settlers Hospital O.R Tambo Gateway CHC ISRDS NODE Holy Cross Hospital Mhlakulo CHC Nessie Knight Hospital Ngangelizwe CHC St Barnabas Hospital St Elizabeth Hospital St Patrick's Hospital Zithulele Hospital This gazette is also available free online at www.gpwonline.co.za 14 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 FREE STATE Motheo District(DC17) National Dental Clinic Botshabelo District Hospital Fezile Dabi District(DC20) Kroonstad Dental Clinic MafubefTokollo Hospital Complex Metsimaholo/Parys Hospital Complex Lejweleputswa DistrictWelkom Clinic Area(DC18) Thabo Mofutsanyana District Elizabeth Ross District Hospital* (DC19) Itemoheng Hospital* ISRDS NODE Mantsopa -

Vote 03 : Health
120 Department: Health 7DEOH6XPPDU\RIGHSDUWPHQWDODOORFDWLRQ 5¶ 7REHDSSURSULDWHGE\9RWHLQ 5 5HVSRQVLEOH0(& 0(&IRU+HDOWK $GPLQLVWUDWLQJ'HSDUWPHQW 'HSDUWPHQWRI+HDOWK $FFRXQWLQJ2IILFHU +HDGRI'HSDUWPHQW 2YHUYLHZ 9LVLRQ $TXDOLW\KHDOWKVHUYLFHWRWKHSHRSOHRIWKH(DVWHUQ&DSH3URYLQFHSURPRWLQJDEHWWHUOLIHIRUDOO 0LVVLRQ 7RSURYLGHDQGHQVXUHDFFHVVLEOHFRPSUHKHQVLYHLQWHJUDWHGVHUYLFHVLQWKH(DVWHUQ&DSHHPSKDVL]LQJ WKH SULPDU\ KHDOWK FDUH DSSURDFK RSWLPDOO\ XWLOLVLQJ DOO UHVRXUFHV WR HQDEOH DOO LWV SUHVHQW DQG IXWXUH JHQHUDWLRQVWRHQMR\KHDOWKDQGTXDOLW\RIOLIH &RUHIXQFWLRQVDQGUHVSRQVLELOLWLHV 7KHFRUHIXQFWLRQVDQGUHVSRQVLELOLWLHVRIWKHGHSDUWPHQWZKLFKDUHDOLJQHGWRWKHQDWLRQDODQGSURYLQFLDO SULRULWLHV LQFOXGLQJ RYHUKDXOLQJ WKH SURYLQFLDO KHDOWKFDUH V\VWHP E\ LPSOHPHQWLQJ DQG VXVWDLQLQJ DQ HYLGHQFH DQG UHVXOWVEDVHG SURYLQFLDO KHDOWK V\VWHP ZKLFK LV DOLJQHG WR WKH 1DWLRQDO +HDOWK 6\VWHP 1+6 SRLQWSODQQDWLRQDODQGSURYLQFLDOOHJLVODWLYHUHTXLUHPHQWVDQGGLVHDVHSURILOHV%XLOGLQJWKH UHTXLUHGFDSDFLW\WRRYHUVHHDQGPDQDJHKHDOWKVHUYLFHVLQWKHSURYLQFHWKURXJK ,PSURYLQJWKHTXDOLW\DQGFRQWLQXXPRISULPDU\KHDOWKFDUH LQFOXGLQJFRPPXQLW\EDVHGDQGKRVSLWDO VHUYLFHV E\ LPSOHPHQWLQJ D UHVRXUFHG SDFNDJH RI VHUYLFHV DQG LPSURYLQJ FOLQLFDO JRYHUQDQFH V\VWHPVDQGSURFHVVHVDQG 5HGXFLQJ PRUELGLW\ DQG PRUWDOLW\ GXH WR FRPPXQLFDEOH GLVHDVHV DQG QRQFRPPXQLFDEOH LOOQHVVHV DQGFRQGLWLRQVE\LPSOHPHQWLQJKLJKLPSDFWVWUDWHJLHVWRDGGUHVVSUHYHQWLRQGHWHFWLRQPDQDJHPHQW DQGVXSSRUWDWDOOOHYHOVRIFDUH 7KHVWUDWHJLFREMHFWLYHVDUHLQOLQHZLWKWKHLPSOHPHQWDWLRQRIWKH1DWLRQDODQG3URYLQFLDO'HYHORSPHQW 3ODQ 1'3 WKH 0HGLXP 7HUP 6WUDWHJLF )UDPHZRUN -

Covid-19 Sentinel Hospital Surveillance for Hcws Report
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 32, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 8 August 2020 on the DATCOV platform. HIGHLIGHTS As of 8 August 2020, 965 (2.0%) of the 49106 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 161 facilities (47 public-sector and 114 private-sector) in all nine provinces of South Africa. Among 565/965 (58.5%) HCWs with available data on type of work, 262/565 (46.4%) were nurses, 175/565 (31.0%) were categorized as other HCWs, 30/565 (5.3%) porters or administrators, 29/565 (5.1%) allied HCWs, 24/565 (4.2%) doctors, 13/565 (2.3%) paramedics, and 6/565 (1.1%) laboratory scientists. There was an increase of 82 new HCW admissions since week 31. There were 214 (22.2%) and 751 (77.8%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (289, 29.9%), KwaZulu-Natal (267, 27.7%), Western Cape (115, 11.9%), Free State (99, 10.3%) and Eastern Cape (93, 9.6%). The median age of COVID-19 HCW admissions was 45 years, there were 92 (9.5%) admissions in HCWs aged 60 years and older. A total of 765 (79.3%) were female. -

1567 Mrs HO Mkhaliphi (EFF) to Ask the Minister of Health
SUBJECT: PARLIAMENTARY QUESTION 1567(NW1704E): MRS HO MKHALIPHI AND MS NR MASHABELA (EFF) TO ASK THE MINISTER OF HEALTH: QUESTIONS FOR WRITTEN REPLY QUESTION 1567-2018 1567 Mrs HO Mkhaliphi (EFF) to ask the Minister of Health: 1. What is the (a) total number of cleaners are employed at each hospital in the country, (b)(i) name and (ii) location of each hospital and (c) name of each company that employees the cleaning personnel? Response 1. (a)(b)(i) and (ii) - Your attention is directed to the table attached of cleaners appointed on the PERSAL system. 2. (c) Information regarding private cleaners employed have been requested from Provincial Departments DISTRICT HOSPITAL 103 11 114 300260 - SUBSECTION:CLEANING SERVICES BISHO HOSPIT 9 9 300329 - SUBSECTION :CLEANING SERVICES BURGERSDORP 1 1 300443 - SUBSECTION :CLEANING SERVICES CALA HOSPITA 1 1 300486 - SECTION :PROVISIONING ADMINISTRATION CANZI 1 1 300587 - SUBSECTION :CLEANING SERVICES CLOETE JOUBE 1 1 300635 - SECTION :CLEANING SERVICES CRADOCK HOSPITA 1 1 300691 - SUBSECTION :CLEANING SERVICES COFIMVABA HO 1 1 300940 - SUBSECTION :CLEANING SERVICES GLEN GREY HO 7 7 303041 - SUBSECTION :CLEANING SERVICES MADWALENI HO 1 1 304036 - SUBSECTION :CLEANING SERVICES MIDLAND HOSP 1 1 307355 - HOSPITAL:STUTIERHEIM 1 1 2 307365 - SUBDIVISION :OPERATIONS STUTIERHEIM HOSPIT 8 8 307396 - HOSPITAL:TARKASTAD DISTRICT HOSPITAL 5 5 307407 - SUBDIVISION :OPERATIONS TARKASTAD HOSPITAL 6 6 307419 - HOSPITAL: MOLTENO DISTRICT HOSPITAL 1 1 307430 - SUBDIVISION :OPERATIONS MOLT ENO HOSPITAL 6 6 307440 - HOSPITAL:NEW -

An Exploration and Description of Rural Rehabilitation Service Model in the Mbhashe Municipality, Amathole District in the Easte
AN EXPLORATION AND DESCRIPTION OF RURAL REHABILITATION SERVICE MODEL IN THE MBHASHE MUNICIPALITY, AMATHOLE DISTRICT IN THE EASTERN CAPE PROVINCE OF SOUTH AFRICA: A PILOT STUDY (Presented in an article format for the African Journal of Disability). Nozipiwo Joyce Gysman Submitted in partial fulfilment of the re quirements for the degree MSc Med Sc. R ehabilitation Studies (Structured) Centre for Rehabilitation Studies Stellenbosch University 2020 Supervisor: Prof Gubela Mji Stellenbosch University https://scholar.sun.ac.za DECLARATION I, Nozipiwo Joyce Gysman declare that the work contained in this research assignment is entirely my own, original work (except where acknowledgement indicates otherwise), and it has not been previously submitted for any other degree at Stellenbosch University or at another University. Nozipiwo Joyce Gysma Date: March 2020 Copyright © 2020 Stellenbosch University All rights reserved Stellenbosch University https://scholar.sun.ac.za ABSTRACT Background People with disabilities are still disadvantaged in accessing health and rehabilitation services, especially those who reside in rural areas, despite the available policies. Rehabilitation is one of the components of Primary Health Care (PHC) but it remains excluded and poorly understood in PHC programmes. Despite available policies to address rehabilitation for people with disabilities (PWDs), PWDs still have difficulty accessing the rehabilitation services. Rehabilitation remains: • excluded and poorly understood in PHC programmes, • fragmented and uncoordinated with services inaccessible to some parts of society especially in the rural context compared to urban counterparts, • dominated by the medical model and institutionalization of services, and • questionable in terms of relevance of services as there is less involvement, guidance and support from communities where these rehabilitation services are being provided. -

Covid-19 Sentinel Hospital Surveillance for Hcws Report
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 37, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 12 September 2020 on the DATCOV platform. HIGHLIGHTS As of 12 September 2020, 2 811 (4.2%) of the 66 920 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 253 facilities (87 public-sector and 166 private-sector) in all nine provinces of South Africa. Among 885/2811 (31.5%) HCWs with available data on type of work, 430/885 (50.1%) were nurses, 165/885 (19.2%) were categorized as other HCWs, 119/885 (13.4%) porters or administrators, 65/885 (7.6%) allied HCWs, 56/885 (6.5%) doctors, 16/885 (1.9%) paramedics, and 7/885 (0.8%) laboratory scientists. There was an increase of 125 new HCW admissions since week 36. There were 407 (14.5%) and 2404 (85.5%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (869, 30.9%), KwaZulu-Natal (697, 24.8%), Eastern Cape (490, 17.3%) and Western Cape (290, 10.3%). The median age of COVID-19 HCW admissions was 49 years, there were 556 (19.8%) admissions in HCWs aged 60 years and older. A total of 2000 (71.2%) were female. -

36936 16-10 Health Layout 1
Government Gazette Staatskoerant REPUBLIC OF SOUTH AFRICA REPUBLIEK VAN SUID-AFRIKA October Vol. 580 Pretoria, 16 2013 Oktober No. 36936 N.B. The Government Printing Works will not be held responsible for the quality of “Hard Copies” or “Electronic Files” submitted for publication purposes AIDS HELPLINE: 0800-0123-22 Prevention is the cure 305126—A 36936—1 2 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 IMPORTANT NOTICE The Government Printing Works will not be held responsible for faxed documents not received due to errors on the fax machine or faxes received which are unclear or incomplete. Please be advised that an “OK” slip, received from a fax machine, will not be accepted as proof that documents were received by the GPW for printing. If documents are faxed to the GPW it will be the sender’s respon- sibility to phone and confirm that the documents were received in good order. Furthermore the Government Printing Works will also not be held responsible for cancellations and amendments which have not been done on original documents received from clients. CONTENTS • INHOUD Page Gazette No. No. No. GOVERNMENT NOTICES Health, Department of Government Notices 787 Health Professions Act (56/1974): List of approved facilities for the purposes of performing community services: Clinical Psychologists in the year 2014 ......................................................................................................................... 3 36936 788 do.: do.: Dentists in the year 2014................................................................................................................................ -

Covid-19 Sentinel Hospital Surveillance for Hcws Report
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 34, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 22 August 2020 on the DATCOV platform. HIGHLIGHTS As of 22 August 2020, 2 481 (4.2%) of the 58 594 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 245 facilities (71 public-sector and 174 private-sector) in all nine provinces of South Africa. Among 701/2481 (28.3%) HCWs with available data on type of work, 335/701 (47.8%) were nurses, 171/701 (24.4%) were categorized as other HCWs, 88/701 (12.5%) porters or administrators, 47/701 (6.7%) allied HCWs, 37/701 (5.3%) doctors, 16/701 (2.3%) paramedics, and 7/701 (1.0%) laboratory scientists. There was an increase of 261 new HCW admissions since week 33. Notably, 185/261 HCW admissions were retrospectively captured into the DATCOV system and are not real-time admissions from the last week. There were 299 (12.1%) and 2182 (87.9%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (778, 31.4%), KwaZulu-Natal (606, 24.4%), Eastern Cape (395, 15.9%) and Western Cape (276, 11.1%). The median age of COVID-19 HCW admissions was 49 years, there were 440 (17.7%) admissions in HCWs aged 60 years and older.