Adverse Effects and Precautions Pharmacokinetics Uses And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Safety Data Sheet
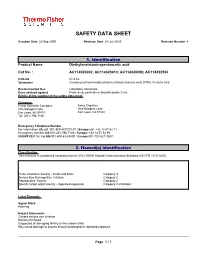
SAFETY DATA SHEET Creation Date 22-Sep-2009 Revision Date 24-Jun-2020 Revision Number 4 1. Identification Product Name Diethylenetriaminepentaacetic acid Cat No. : AC114320000; AC114320010; AC114320050; AC114322500 CAS-No 67-43-6 Synonyms (Carboxymethylimino)bis(ethylenenitrilo)tetraacetic acid; DTPA; Pentetic acid Recommended Use Laboratory chemicals. Uses advised against Food, drug, pesticide or biocidal product use. Details of the supplier of the safety data sheet Company Fisher Scientific Company Acros Organics One Reagent Lane One Reagent Lane Fair Lawn, NJ 07410 Fair Lawn, NJ 07410 Tel: (201) 796-7100 Emergency Telephone Number For information US call: 001-800-ACROS-01 / Europe call: +32 14 57 52 11 Emergency Number US:001-201-796-7100 / Europe: +32 14 57 52 99 CHEMTREC Tel. No.US:001-800-424-9300 / Europe:001-703-527-3887 2. Hazard(s) identification Classification This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute Inhalation Toxicity - Dusts and Mists Category 4 Serious Eye Damage/Eye Irritation Category 2 Reproductive Toxicity Category 2 Specific target organ toxicity - (repeated exposure) Category 2 Inhalation Label Elements Signal Word Warning Hazard Statements Causes serious eye irritation Harmful if inhaled Suspected of damaging fertility or the unborn child May cause damage to organs through prolonged or repeated exposure ______________________________________________________________________________________________ Page 1 / 7 Diethylenetriaminepentaacetic acid Revision -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

Time Dependent Dual Effect of Anti-Inflammatory Treatments On
Neurotoxicology 74 (2019) 19–27 Contents lists available at ScienceDirect Neurotoxicology journal homepage: www.elsevier.com/locate/neuro Full Length Article Time dependent dual effect of anti-inflammatory treatments on sarin- induced brain inflammation: Suggested role of prostaglandins T ⁎ Shira Chapman, Ettie Grauer , Rellie Gez, Inbal Egoz, Shlomi Lazar Israel Institute for Biological Research, Israel ARTICLE INFO ABSTRACT Keywords: A common consequence of exposure to organophosphate nerve agents is the centrally mediated seizure activity Sarin that appears even after conventional treatment with atropine and oximes. We have previously demonstrated a Organophosphates major inflammatory response with subsequent brain damage which was correlated with the duration of the fl Anti-in ammatory sarin-induced seizures (Chapman et al., 2006). In the present work seizures were induced by the nerve agent Prostaglandins sarin (1.2 LD50) insufficiently treated 1 min later by atropine and trimedoxime bromide (TA), with additional Convulsions midazolam treatment either 5 or 30 min after continuous seizure activity. The efficacy of both steroidal and nonsteroidal anti-inflammatory drugs (NSAIDs), as well as other drugs that were reported as beneficial in neuroprotection, were evaluated for their contribution as adjunct treatment against sarin induced seizures and the ensuing inflammatory brain damage. Results show that both steroids and NSAIDs were harmful when ad- ministered during convulsions, and steroids were at best ineffective if administered at their termination. However, if administered at termination of convulsions, the NSAID ibuprofen, the selective COX 2 inhibitor nimesulide and the PLA2 inhibitor quinacrine were partially effective in reducing brain inflammatory markers. Administration of exogenous analogs of prostaglandins (PGE2) immediately following sarin-induced convulsions was found to have a beneficial effect in reducing brain inflammatory markers measured at 24 h and one week post sarin exposure. -

The Nutrition and Food Web Archive Medical Terminology Book
The Nutrition and Food Web Archive Medical Terminology Book www.nafwa. -

Download S/2013/735
United Nations A/68/663–S/2013/735 General Assembly Distr.: General 13 December 2013 Security Council Original: English General Assembly Security Council Sixty-eighth session Sixty-eighth year Agenda item 33 Prevention of armed conflict Identical letters dated 13 December 2013 from the Secretary-General addressed to the President of the General Assembly and the President of the Security Council I have the honour to convey herewith the final report of the United Nations Mission to Investigate Allegations of the Use of Chemical Weapons in the Syrian Arab Republic (see annex). I would be grateful if the present final report, the letter of transmittal and its appendices could be brought to the attention of the Members of the General Assembly and of the Security Council. (Signed) BAN Ki-moon 13-61784 (E) 131213 *1361784* A/68/663 S/2013/735 Annex Letter of transmittal Having completed our investigation into the allegations of the use of chemical weapons in the Syrian Arab Republic reported to you by Member States, and further to the report of the United Nations Mission to Investigate Allegations of the Use of Chemical Weapons in the Syrian Arab Republic (hereinafter, the “United Nations Mission”) on allegations of the use of the chemical weapons in the Ghouta area of Damascus on 21 August 2013 (A/67/997-S/2013/553), we have the honour to submit the final report of the United Nations Mission. To date, 16 allegations of separate incidents involving the use of chemical weapons have been reported to the Secretary-General by Member States, including, primarily, the Governments of France, Qatar, the Syrian Arab Republic, the United Kingdom of Great Britain and Northern Ireland and the United States of America. -

Professor Jo Klaveness School of Pharmacy University of Oslo
SUPERVISORS Professor Jo Klaveness School of Pharmacy University of Oslo Associate professor Pål Rongved School of Pharmacy University of Oslo 1 TABLE OF CONTENTS TABLE OF CONTENTS 1 ABBREVIATIONS..........................................................................5 2 ABSTRACT.....................................................................................6 3 INTRODUCTION............................................................................7 3.1 Acetylcholine- a neurotransmitter Synthesis, release and inactivation ... 7 3.1.1 Structure of acetylcholinesterase .................................................................... 8 3.2 Anticholinesterases interfere with acetylcholine activity ........................ 9 3.3 Effects of anticholinesterases................................................................... 9 3.4 Different groups of anticholinesterases.................................................. 10 3.4.1 Short- acting anticholinesterases .................................................................. 10 3.4.2 Medium- duration anticholinesterases .......................................................... 11 3.4.3 Irreversible anticholinesterases..................................................................... 12 3.5 Nerve agents: Irreversible anticholinesterases....................................... 13 3.5.1 The dawn of a deadly weapon ...................................................................... 14 3.5.2 Biochemistry................................................................................................ -

Nomination Background: 1-Butyl-3-Methylimidazolium Chloride
Ionic Liquids 1-Butyl-3-methylimidazolium Chloride (CAS No. 79917-90-1) 1-Butyl-1-methylpyrrolidinium Chloride (CAS No. 479500-35-1) N-Butylpyridinium Chloride (CAS No. 1124-64-7) Review of Toxicological Literature May 2004 Ionic Liquids 1-Butyl-3-methylimidazolium Chloride (CAS No. 79917-90-1) 1-Butyl-1-methylpyrrolidinium Chloride (CAS No. 479500-35-1) N-Butylpyridinium Chloride (CAS No. 1124-64-7) Review of Toxicological Literature Prepared for National Toxicology Program (NTP) National Institute of Environmental Health Sciences (NIEHS) National Institutes of Health U.S Department of Health and Human Services Contract No. N01-ES-35515 Project Officer: Scott A. Masten, Ph.D. NTP/NIEHS Research Triangle Park, North Carolina Prepared by Integrated Laboratory Systems, Inc. Research Triangle Park, North Carolina May 2004 Toxicological Summary for Ionic Liquids 05/2004 Abstract Ionic liquids are salts of organic cations with melting points generally below 100 °C and are being widely investigated as replacements for volatile organic solvents in industrial and laboratory processes because they are thought to be "environmentally benign." Although some efforts have begun to study their potential for ecotoxicity, limited vertebrate or genetic toxicity testing has been done. Three ionic liquids, 1-butyl-3-methylimidazolium chloride ([bmim]Cl), 1-butyl-1-methylpyrrolidinium chloride ([bmpy]Cl), and N-butylpyridinium chloride ([NBuPy]Cl), were nominated to the National Toxicology Program (NTP) for toxicological testing based on their widespread interest as possible alternatives to organic solvents. These chlorides are representative of the three most common cation classes of ionic liquids being investigated: imidazolium, pyridinium, and pyrrolidinium. The chlorides, soluble in water and polar organic liquids, are generally prepared from approximately equimolar amounts of the appropriately substituted heterocyclic compound and butyl chloride, often under both heat and pressure. -

Efficacy of Trimedoxime in Mice Poisoned with Dichlorvos, Heptenophos Or Monocrotophos
CORE Metadata, citation and similar papers at core.ac.uk Provided by FarFar - Repository of the Faculty of Pharmacy, University of Belgrade C Basic & Clinical Pharmacology & Toxicology 2005, 96, 111–117. Printed in Denmark . All rights reserved Copyright C ISSN 1742-7835 Efficacy of Trimedoxime in Mice Poisoned with Dichlorvos, Heptenophos or Monocrotophos Biljana Antonijevic´1, Dubravko Bokonjic´2, Milosˇ P. Stojiljkovic´2, Vesna Kilibarda2, Zoran A. Milovanovic´2, Mirjana Nedeljkovic´1 and Matej Maksimovic´1 1Institute of Toxicological Chemistry, School of Pharmacy, University of Belgrade, Vojvode Stepe 450, and 2National Poison Control Centre, Military Medical Academy, Crnotravska 17; 11000 Belgrade, Serbia and Montenegro (Received June 18, 2004; Accepted September 3, 2004) Abstract: The aim of the study was to examine antidotal potency of trimedoxime in mice poisoned with three direct dimethoxy-substituted organophosphorus inhibitors. In order to assess the protective efficacy of trimedoxime against dichlorvos, heptenophos or monocrotophos, median effective doses and efficacy half-times were calculated. Trimedoxime (24 mg/kg intravenously) was injected 5 min. before 1.3 LD50 intravenously of poisons. Activities of brain, diaphragmal and erythrocyte acetylcholinesterase, as well as of plasma carboxylesterases were determined at different time intervals (10, 40 and 60 min.) after administration of the antidotes. Protective effect of trimedoxime decreased according to the following order: monocrotophos Ͼ heptenophos Ͼ dichlorvos. Administration of the oxime produced a significant reacti- vation of central and peripheral acetylcholinesterase inhibited with dichlorvos and heptenophos, with the exception of erythrocyte acetylcholinesterase inhibited by heptenophos. Surprisingly, trimedoxime did not induce reactivation of mon- ocrotophos-inhibited acetylcholinesterase in any of the tissues tested. -

Nitric Oxide Modulation of Interleukin-1Я-Evoked Intracellular
The Journal of Neuroscience, December 15, 2000, 20(24):8980–8986 Nitric Oxide Modulation of Interleukin-1-Evoked Intracellular Ca2؉ Release in Human Astrocytoma U-373 MG Cells and Brain Striatal Slices Antonella Meini,1 Alberto Benocci,1 Maria Frosini,1 Gianpietro Sgaragli,1 Gianpaolo Pessina,2 Carlo Aldinucci,2 Gise` le Tchuisseu Youmbi,1 and Mitri Palmi1 1Istituto di Scienze Farmacologiche and 2Istituto di Fisiologia, Universita` di Siena, 53100 Siena, Italy Intracellular Ca 2ϩ mobilization and release into mammal CSF Ca 2ϩ release induced by 2.5 but not 10 ng/ml IL-1. Ruthenium plays a fundamental role in the etiogenesis of fever induced by red (50 M) and, to a lesser extent, heparin (3 mg/ml) antagonized the proinflammatory cytokine interleukin-1 (IL-1) and other IL-1-induced Ca 2ϩ release, and both compounds administered pyrogens. The source and mechanism of IL-1-induced intracel- together completely abolished this response. Similar results were lular Ca 2ϩ mobilization was investigated using two experimental obtained in human astrocytoma cells in which IL-1 elicited a models. IL-1 (10 ng/ml) treatment of rat striatal slices preloaded delayed (30 min) increase in intracellular Ca 2ϩ concentration 45 2ϩ 2ϩ Ϯ with Ca elicited a delayed (30 min) and sustained increase ([Ca ]i ) (402 71.2% of baseline), which was abolished by 1 45 2ϩ (125–150%) in spontaneous Ca release that was potentiated mML-NAME. These data indicate that the NO/cGMP-signaling by L-arginine (300 M) and counteracted by N--nitro-L-arginine pathway is part of the intracellular mechanism transducing IL- 2ϩ methyl ester (L-NAME) (1 and 3 mM). -

Acetylcholinesterase: the “Hub” for Neurodegenerative Diseases And
Review biomolecules Acetylcholinesterase: The “Hub” for NeurodegenerativeReview Diseases and Chemical Weapons Acetylcholinesterase: The “Hub” for Convention Neurodegenerative Diseases and Chemical WeaponsSamir F. de A. Cavalcante Convention 1,2,3,*, Alessandro B. C. Simas 2,*, Marcos C. Barcellos 1, Victor G. M. de Oliveira 1, Roberto B. Sousa 1, Paulo A. de M. Cabral 1 and Kamil Kuča 3,*and Tanos C. C. França 3,4,* Samir F. de A. Cavalcante 1,2,3,* , Alessandro B. C. Simas 2,*, Marcos C. Barcellos 1, Victor1 Institute G. M. ofde Chemical, Oliveira Biological,1, Roberto Radiological B. Sousa and1, Paulo Nuclear A. Defense de M. Cabral (IDQBRN),1, Kamil Brazilian Kuˇca Army3,* and TanosTechnological C. C. França Center3,4,* (CTEx), Avenida das Américas 28705, Rio de Janeiro 23020-470, Brazil; [email protected] (M.C.B.); [email protected] (V.G.M.d.O.); [email protected] 1 Institute of Chemical, Biological, Radiological and Nuclear Defense (IDQBRN), Brazilian Army (R.B.S.); [email protected] (P.A.d.M.C.) Technological Center (CTEx), Avenida das Américas 28705, Rio de Janeiro 23020-470, Brazil; 2 [email protected] Mors Institute of Research (M.C.B.); on Natural [email protected] Products (IPPN), Federal (V.G.M.d.O.); University of Rio de Janeiro (UFRJ), CCS,[email protected] Bloco H, Rio de Janeiro (R.B.S.); 21941-902, [email protected] Brazil (P.A.d.M.C.) 32 DepartmentWalter Mors of Institute Chemistry, of Research Faculty of on Science, Natural Un Productsiversity (IPPN), -

Drugs Which Can Affect Near Vision: a Useful List
Drugs Which Can Affect Near Vision: A Useful List Joanne L. Smith B.Sc., Ph.Phm.* J. Raymond Buncic, M.D., F.R.C.S.(C)t ABSTRACT This paper documents a list of drugs that cause problems with near vision, by virtue of effects on accommodation, occasionally refractive error and diplopia. It is meant as a reference aid to the clinician when confronted with problems of focusing on near objects or print. There are many drugs that have been reported to interfere with near or reading vision, producing blurring, decreased accommodation and diplopia. This paper lists the drugs that have been reported in the literature to produce symptoms which interfere with near vision. Case reports for the listed drugs vary greatly from many to few. The drugs have been divided into the following categories: those causing (A) blurring at near, (B) diplopia and (C) induced myopia. Those drugs which only rarely cause these symptoms have been omitted. From the Departments of Pharmacy* and Ophthalmologyt, The Hospital For Sick Children, Toronto, Ontario, Canada Requests for reprints should be addressed to: Dr. J. Raymond Buncic, Department of Ophthalmology, The Hospital For Sick Children, 555 University Ave., Toronto, Ontario, Canada M5G lX8 TABLE 1 DRUGS COMMONLY CAUSING DIFFICULTY WITH FOCUSING AT NEAR OR BLURRED VISION. DRUG INCIDENCE REFERENCE Antipsychotics Chlorpromazine 14-23 8 Clozapine 5 8,14 Fluphenazine 1.2-4.3 8 Haloperidol 6.8-16 8 Loxapine 12,14 Perphenazine 7.4-17.8 8 Pimozide 20 8 Risperidone 1-2%, >/= 10% 11 Thioridazine 0.6-18 8 Thiothixene 20 8 -

(12) Patent Application Publication (10) Pub. No.: US 2012/0046244 A1 Rogers Et Al
US 20120046244A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2012/0046244 A1 Rogers et al. (43) Pub. Date: Feb. 23, 2012 (54) DUAL FUNCTIONING IONIC LIQUIDS AND (86). PCT No.: PCT/USO9/69652 SALTS THEREOF S371 (c)(1), (75) Inventors: Robin D. Rogers, Tuscaloosa, AL (2), (4) Date: Nov. 3, 2011 (US); Daniel T. Daly, Tuscaloosa, AL (US); Douglas MacFarlane, Related U.S. Application Data SG (KSR,kiSt. Port (60) Eyal application No. 61/141,168, filed on Dec. Seddon, Donaghadee (IE): s Gabriela Gurau, Tuscaloosa, AL O O (US); Katharina Bica, Vienna Publication Classification (AT); Jelena Turanjanin, Victoria (51) Int. Cl. (AU); Pamela M. Dean, Victoria A6II 3/66 (2006.01) (AU) A6II 3L/205 (2006.01) A6II 3/545 (2006.01) (73) Assignees: THE BOARD OF TRUSTEES OF A613/606 (2006.01) THE UNIVERSITY OF (52) U.S. Cl. ......... 514/75; 514/166; 514/555; 514/226.2 ALABAMA, Tuscaloosa, AL (US); QUEENS UNIVERSITY (57) ABSTRACT BELFAST, Belfast (UK); MONASH UNIVERSITY, Disclosed herein are ionic liquid compositions comprising Melbourne (AU) active pharmaceutical, biological, and nutritional com pounds, and methods of use. Further disclosed are composi (21) Appl. No.: 13/142.559 tions of matter including liquid ion pairs alone or in Solution and their use; compositions of ionic liquids that are solvated. (22) PCT Filed: Dec. 29, 2009 for example, hydrated and their uses. Patent Application Publication Feb. 23, 2012 Sheet 1 of 7 US 2012/0046244 A1 O 20 40 SO 8) O) Wit% Choline DPP Fig. 1 Patent Application Publication Feb. 23, 2012 Sheet 2 of 7 US 2012/0046244 A1 CN- P(Busal H, Vam 4.