ANZCOR Guideline 11.6 – Equipment and Techniques in Adult Advanced Life Support Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -
TCCC CLS Skill Instructions Mod 7 25 JAN 20
MODULE 07: AIRWAY MANAGEMENT IN TFC SKILL INSTRUCTIONS 25 JAN 2020 COMBAT LIFESAVER (CLS) TACTICAL COMBAT CASUALTY CARE SKILL INSTRUCTIONS HEAD-TILT/CHIN-LIFT INSTRUCTION TASK: Open an airway using the head-tilt/chin-lift maneuver CONDITION: Given a simulated scenario where a casualty and responder are in combat gear and the casualty is unconscious without a patent airway STANDARD: EffeCtively open the airway by performing the head-tilt/chin-lift maneuver following all steps and measures correctly without Causing further harm to the Casualty EQUIPMENT: N/A PERFORMANCE MEASURES: step-by-step instructions NOTE: Do not use if a spinal or neck injury is suspected. 01 Roll the Casualty onto their back, if necessary, and place them on a hard, flat surface. 02 Kneel at the level of the Casualty’s shoulders. Position yourself at the side of the Casualty. 03 Open the mouth and looK for visible airway obstruCtions (e.g., laCerations, obstructions, broken teeth, burns, or swelling or other debris, such as vomit). NOTE: If foreign material or vomit is in the mouth, remove it as quiCKly as possible. NOTE: Do not perform a blind finger sweep. 04 PlaCe one hand on the Casualty's forehead and apply firm, backward pressure with the palm to tilt the head back. 05 PlaCe the fingertips of the other hand under the bony part of the lower jaw and lift, bringing the Chin forward. NOTE: Do not use the thumb to lift the chin. 06 While maintaining the open airway position, place an ear over the casualty's mouth and nose, looking toward the chest and stomaCh. -
Prehospital Airway Management Using the Laryngeal Tube an Emergency Department Point of View
Notfallmedizin Anaesthesist 2014 · 63:589–596 M. Bernhard1 · W. Beres2 · A. Timmermann3 · R. Stepan4 · C.-A. Greim5 · U.X. Kaisers6 · DOI 10.1007/s00101-014-2348-1 A. Gries1 Published online: 2. Juli 2014 1 Emergency Department, University Hospital of Leipzig, Leipzig © Springer-Verlag Berlin Heidelberg 2014 2 Department of Anaesthesiology and Intensive Care Medicine, Main Klinik Ochsenfurt, Ochsenfurt 3 Department of Anaesthesiology, Pain Therapy, Intensive Care Medicine and Emergency Medicine, DRK Kliniken Berlin Westend und Mitte, Berlin Redaktion 4 Department of Public Health, Fulda County, Fulda A. Gries, Leipzig 5 Department of Anesthesiology, Intensive Care Medicine and Emergency Medicine, Hospital of Fulda, Fulda V. Wenzel, Innsbruck 6 Department of Anesthesiology and Intensive Care Medicine, University Leipzig, Medical Faculty, Leipzig Prehospital airway management using the laryngeal tube An emergency department point of view Securing the airway and maintaining ox- Studies describing the successful use of mittee of the Medical Faculty of Leipzig, ygenation and ventilation represent es- the laryngeal tube in the prehospital setting Germany. Single cases were documented sential life-saving strategies in emergen- sound promising [9, 10, 22]. However, the initially after ED admission. The case se- cy medicine [1, 2, 3, 40]. Depending on results of these studies and of case reports ries was evaluated retrospectively, was not the experience of the person performing were not reported by an independent ob- preregistered, and written informed con- the procedure and on the individual in- server and, therefore, reporting bias could tent could not be obtained. tubation conditions, endotracheal intuba- be possible [11, 22]. Only one prospective, tion (ETI) is still considered to be the gold randomized study has confirmed that the Results standard [4, 5, 40]. -

Airway – Oropharyngeal: Insertion; Maintenance; Suction; Removal
Policies & Procedures Title: AIRWAY – OROPHARYNGEAL: INSERTION; MAINTENANCE; SUCTION; REMOVAL I.D. Number: 1159 Authorization Source: Nursing Date Revised: September 2014 [X] SHR Nursing Practice Committee Date Effective: October 2002 Date Reaffirmed: January 2016 Scope: SHR Acute, Parkridge Centre Any PRINTED version of this document is only accurate up to the date of printing 30-May-16. Saskatoon Health Region (SHR) cannot guarantee the currency or accuracy of any printed policy. Always refer to the Policies and Procedures site for the most current versions of documents in effect. SHR accepts no responsibility for use of this material by any person or organization not associated with SHR. No part of this document may be reproduced in any form for publication without permission of SHR. 1. PURPOSE 1.1 To safely and effectively use Oropharyngeal Airway (OPA). 2. POLICY 2.1 The Registered Nurse (RN), Registered Psychiatric Nurse (RPN), Licensed Practical Nurse (LPN), Graduate Nurse (GN), Graduate Psychiatric Nurse (GPN), Graduate Licensed Practical Nurse (GLPN) will insert, maintain, suction and remove an oropharyngeal airway (OPA). 2.2 The OPA may be inserted to establish and assist in maintaining a patent airway. 2.3 An OPA should only be used in patients with decreased level of consciousness or decreased gag reflex. 2.4 Patients with OPAs that have been inserted for airway protection should not be left unattended due to risk of aspiration if gag reflex returns unexpectedly. Page 1 of 4 Policies and Procedures: Airway – Oropharyngeal: Insertion; Maintenance; I.D. # 1159 Suction; Removal 3. PROCEDURE 3.1 Equipment: • Oropharyngeal airway of appropriate size • Tongue blade (optional) • Clean gloves • Optional: suction equipment, bag-valve-mask device 3.2 Estimate the appropriate size of airway by aligning the tube on the side of the patient’s face parallel to the teeth and choosing an airway that extends from the ear lobe to the corner of the mouth. -
Scope of Practice Statements
Scope of Practice Statements Emergency Medical Services Authority California Health and Human Services Agency EMSA # 300 November 2017 HOWARD BACKER, MD, MPH, FACEP DIRECTOR DANIEL R. SMILEY CHIEF DEPUTY DIRECTOR SEAN TRASK DIVISION CHIEF EMSA # 300 Released November 2017 EMSA #300 • Page 1 Table of Contents Introduction ........................................................................................................................................... 4 The EMS Authority ................................................................................................................................ 4 Local EMS Agencies ............................................................................................................................. 4 California EMS Personnel Levels .......................................................................................................... 4 Reading the Scope of Practice Pages .................................................................................................. 5 Airway and Breathing ............................................................................................................................ 6 Airway Suctioning .............................................................................................................................. 7 Automatic Transport Ventilator .......................................................................................................... 8 Bag Valve Mask – BVM .................................................................................................................... -
Basic Life Support + First Aid for Healthcare Providers 2020 Course Introduction
Basic Life Support + First Aid for Healthcare Providers 2020 Course Introduction SECTION 1: Foundational concepts of BCLS SECTION 2: Response to an adult in cardiac arrest SECTION 3: Basic Life Support for infants and children SECTION 4: Automated external defibrillation in infants and children SECTION 5: Preventing cardiac arrest SECTION 6: First aid for adults SECTION 7: First aid for children Activity Summary • Activity Title: Basic Life Support (BLS) & First Aid (Cardiopulmonary Resuscitation (CPR), Automated External Defibrillator (AED), and First Aid) • Release date: 2021-06-01 • Expiration date: 2024-06-01 • Estimated time to complete activity: 8 hours • This course is accessible with any web browser. We recommend recent versions of • Google Chrome, Internet Explorer 9 and later, or Apple iPad. • This course is jointly provided by Pacific Medical Training and Postgraduate Institute for Medicine (PIM). You may reach PIM at [email protected]. Target Audience This activity has been designed to meet the educational needs of physicians, physician assistants, nurse practitioners, registered nurses, pharmacists and dentists involved in the care of patients who require advanced life support. 3103 Philmont Ave, Suite 308 • Huntingdon Valley, PA 19006 • 800-417-1748 page 1 Educational Objectives After completing this activity, the participant should be better able to: • Explain the change in emphasis from airway and ventilation to compressions and perfusion. • Select the correct order of interventions for the victim of cardiopulmonary arrest. • List the steps required to safely operate an AED. • Differentiate between adult and pediatric guidelines for CPR. • Explain how to apply the various first aid interventions. • Describe how to apply the various pediatric first aid interventions. -

Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality 1
Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality 1 Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality Web-based Integrated 2010 & 2015 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Key Words: cardiac arrest cardiopulmonary resuscitation defibrillation emergency 1 Highlights & Introduction 1.1 Highlights: Lay Rescuer CPR Summary of Key Issues and Major Changes Key issues and major changes in the 2015 Guidelines Update recommendations for adult CPR by lay rescuers include the following: The crucial links in the out-of-hospital adult Chain of Survival are unchanged from 2010, with continued emphasis on the simplified universal Adult Basic Life Support (BLS) Algorithm. The Adult BLS Algorithm has been modified to reflect the fact that rescuers can activate an emergency response (ie, through use of a mobile telephone) without leaving the victim’s side. It is recommended that communities with people at risk for cardiac arrest implement PAD programs. Recommendations have been strengthened to encourage immediate recognition of unresponsiveness, activation of the emergency response system, and initiation of CPR if the lay rescuer finds an unresponsive victim is not breathing or not breathing normally (eg, gasping). Emphasis has been increased about the rapid identification of potential cardiac arrest by dispatchers, with immediate provision of CPR instructions to the caller (ie, dispatch-guided CPR). The recommended sequence for a single rescuer has been confirmed: the single rescuer is to initiate chest compressions before giving rescue breaths (C-A-B rather than A-B-C) to reduce delay to first compression. The single rescuer should begin CPR with 30 chest compressions followed by 2 breaths. -

NIMS 508 Stillwater Flood Search and Rescue Team
Resource Typing Definition for Response Mass Search and Rescue Operations STILLWATER/FLOOD SEARCH AND RESCUE TEAM DESCRIPTION The Stillwater/Flood Search and Rescue (SAR) Team conducts search, rescue, and recovery operations for humans and animals in stillwater and stillwater/flood environments RESOURCE CATEGORY Search and Rescue RESOURCE KIND Team OVERALL FUNCTION The Stillwater/Flood SAR team: 1. Searches for and rescues individuals who may be injured or otherwise in need of medical attention 2. Provides emergency medical care, including Basic Life Support (BLS) 3. Provides animal rescue 4. Transports humans and animals to the nearest location for secondary land or air transport 5. Provides shore-based and boat-based water rescue for humans and animals 6. Supports helicopter rescue operations and urban SAR in water environments for humans and animals 7. Operates in environments with or without infrastructure, including environments with disrupted access to roadways, utilities, transportation, and medical facilities, and with limited access to shelter, food, and water COMPOSITION AND ORDERING 1. Requestor and provider address certain needs and issues prior to deployment, including: SPECIFICATIONS a. Communications equipment that enables more than intra-team communications, such as programmable interoperable communications equipment with capabilities for command, logistics, military, air, and so on b. Type of incident and operational environment, such as weather event, levy or dam breach, or risk of hazardous materials (HAZMAT) contamination c. Additional specialized personnel, such as advanced medical staff, animal SAR specialists, logistics specialists, advisors, helicopter support staff, or support personnel for unique operating environments d. Additional transportation-related needs, including specific vehicles, boats, trailers, drivers, mechanics, equipment, supplies, fuel, and so on e. -

The Laryngeal Mask Airway: Potential Applications in Neonates
F485 Arch Dis Child Fetal Neonatal Ed: first published as 10.1136/adc.2003.038430 on 21 October 2004. Downloaded from PERSONAL PRACTICE The laryngeal mask airway: potential applications in neonates D Trevisanuto, M Micaglio, P Ferrarese, V Zanardo ............................................................................................................................... Arch Dis Child Fetal Neonatal Ed 2004;89:F485–F489. doi: 10.1136/adc.2003.038430 The laryngeal mask airway is a safe and reliable airway 2.5–5 kg.11 It has been postulated that a smaller size (0.5) could be useful in preterm management device. This review describes the insertion newborns. However, there are reports of techniques, advantages, limitations, and potential successful use of size 1 in preterm neonates applications of the laryngeal mask airway in neonates. weighing 0.8–1.5 kg.12–15 ........................................................................... (2) Fully deflate the cuff as described in the manual, and lubricate the back of the mask tip (for neonates in the labour ward, he ability to maintain a patent airway and lubrication may not be necessary, as oral provide effective positive pressure ventilation and pharyngeal secretions may reproduce T(PPV) is the main objective of neonatal this function). resuscitation and all anaesthesiological proce- (3) Press (flatten) the tip of the LMA against the dures.1–6 This is currently achieved with the use hard palate. During this manoeuvre, the of a face mask or an endotracheal tube. Both of these devices have major limitations from a operator should grasp the LMA like a pen strictly anatomical point of view and require with the index finger at the junction adequate operator skills. In certain situations, between the mask and the distal end of the both face mask ventilation and tracheal intuba- airway tube. -
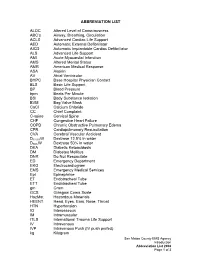
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Basic Life Support Health Care Provider
ELLIS & ASSOCIATES Health Care Provider Basic Life Support MEETS CURRENT CPR & ECC GUIDELINES Ellis & Associates / Safety & Health HEALTH CARE PROVIDER BASIC LIFE SUPPORT - I Ellis & Associates, Inc. P.O. Box 2160, Windermere, FL 34786-2160 www.jellis.com Copyright © 2016 by Ellis & Associates, LLC All rights reserved. No part of this publication may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the publisher, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Ellis & Associates P.O. Box 2160, Windermere, FL 34786-2160 Ordering Information: Quantity sales. Special discounts are available on quantity purchases by corporations, associations, trade bookstores and wholesalers. For details, contact the publisher at the address above. Disclaimer: The procedures and protocols presented in this manual and the course are based on the most current recommendations of responsible medical sources, including the International Liaison Committee on Resuscitation (ILCOR) 2015 Guidelines for CPR & ECC. Ellis & Associates, however, make no guarantee as to, and assume no responsibility for, the correctness, sufficiency, or completeness of such recommendations or information. Additional procedures may be required under particular circumstances. Ellis & Associates disclaims all liability for damages of any kind arising from the use of, reference to, reliance on, or performance based on such information. Library of Congress Cataloging-in-Publication Data Not Available at Time of Printing ISBN 978-0-9961108-0-8 Unless otherwise indicated on the Credits Page, all photographs and illustrations are copyright protected by Ellis & Associates. -

Intravenous Alfaxalone Anaesthesia in Two Squamate Species: Eublepharis Macularius and Morelia Spilota Cheynei
INTRAVENOUS ALFAXALONE ANAESTHESIA IN TWO SQUAMATE SPECIES: EUBLEPHARIS MACULARIUS AND MORELIA SPILOTA CHEYNEI Tesi per il XXIX Ciclo del Dottorato in Scienze Veterinarie, Curriculum Scienze Cliniche Veterinarie Dipartimento di Scienze Veterinarie, Universita’ degli Studi di Messina Tutor: Prof. Filippo Spadola Cotutor: Prof. Zdenek Knotek Dr. Manuel Morici Sommario L’anestesia negli Squamati è una costante sfida della medicina e chirurgia dei rettili. Le differenze morfo-fisiologiche di questi taxa, rendono difficilmente applicabile i comuni concetti di anestesiologia veterinaria usati con successo negli altri animali da compagnia. Diversi protocolli anestetici sono stati utilizzati, sia per l’induzione che per il mantenimento, sia negli ofidi che nei sauri, ma con risultati variabili. Di fatti la maggior parte dei protocolli risultano in induzione o recuperi troppo brevi o troppo lunghi. L’obbiettivo di questa tesi dottorale è di valutare l’efficacia di un anestetico steroideo (alfaxalone), somministrato per via endovenosa in due specie di squamati usati come modello: il geco leopardo (Eublepharis macularius) e il pitone tappeto (Morelia spilota cheynei). Due metodi di somministrazione endovenosa (vena giugulare nei gechi e vena caudale nei serpenti) sono stati analizzati e descritti, usando un dosaggio di anestetico di 5 mg/kg in 20 gechi leopardo, e di 10 mg/kg in 10 pitoni tappeto. Nei gechi il tempo di induzione, il tempo di perdita del tono mandibolare, l’intervallo di anestesia chirurgica e il recupero completo sono stati rispettivamente di 27.5 ± 30.7 secondi, 1.3 ± 1.4 minuti, 12.5 ± 2.2 minuti and 18.8 ± 12.1 minuti. Nei pitoni tappeto, il tempo di induzione, la perdita di sensazione, il tempo di inserimento del tubo endotracheale, l’intervallo di anestesia chirurgica e il recupero sono stati rispettivamente di 3.1±0.8 minuti, 5.6±0.7 minuti, 6.9±0.9 minuti, 18.8±4.7 minuti, e 36.7±11.4 minuti.