General Nutrition Guidelines for Glycogen Storage Disease Type III
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Defective Galactose Oxidation in a Patient with Glycogen Storage Disease and Fanconi Syndrome
Pediatr. Res. 17: 157-161 (1983) Defective Galactose Oxidation in a Patient with Glycogen Storage Disease and Fanconi Syndrome M. BRIVET,"" N. MOATTI, A. CORRIAT, A. LEMONNIER, AND M. ODIEVRE Laboratoire Central de Biochimie du Centre Hospitalier de Bichre, 94270 Kremlin-Bicetre, France [M. B., A. C.]; Faculte des Sciences Pharmaceutiques et Biologiques de I'Universite Paris-Sud, 92290 Chatenay-Malabry, France [N. M., A. L.]; and Faculte de Midecine de I'Universiti Paris-Sud et Unite de Recherches d'Hepatologie Infantile, INSERM U 56, 94270 Kremlin-Bicetre. France [M. 0.1 Summary The patient's diet was supplemented with 25-OH-cholecalci- ferol, phosphorus, calcium, and bicarbonate. With this treatment, Carbohydrate metabolism was studied in a child with atypical the serum phosphate concentration increased, but remained be- glycogen storage disease and Fanconi syndrome. Massive gluco- tween 0.8 and 1.0 mmole/liter, whereas the plasma carbon dioxide suria, partial resistance to glucagon and abnormal responses to level returned to normal (18-22 mmole/liter). Rickets was only carbohydrate loads, mainly in the form of major impairment of partially controlled. galactose utilization were found, as reported in previous cases. Increased blood lactate to pyruvate ratios, observed in a few cases of idiopathic Fanconi syndrome, were not present. [l-14ClGalac- METHODS tose oxidation was normal in erythrocytes, but reduced in fresh All studies of the patient and of the subjects who served as minced liver tissue, despite normal activities of hepatic galactoki- controls were undertaken after obtaining parental or personal nase, uridyltransferase, and UDP-glucose 4epirnerase in hornog- consent. enates of frozen liver. -

Improvement of the Nutritional Management of Glycogen Storage Disease Type I
1 Improvement of the nutritional management of glycogen storage disease type I Kaustuv Bhattacharya Presented for the degree of MD (res) at University College London 2 “The roots below the earth claim no rewards for making the branches fruitful” Sir Rabrindranath Tagore Stray Birds (1917) Acknowledgements Whilst this thesis is my own work, it is the product of several helpful discussions with many people around the world. It was conducted under the supervision of Philip Lee who, since completion of the data collection, faced bigger personal challenges than he could have imagined. I hope that this work is a fitting conclusion to one strategic direction, of some of his research, which I hope he can be proud of. I am very grateful for his help. Peter Clayton has been a source of inspiration throughout my “metabolic” career and his guidance throughout this process has been very gratefully received. I appreciate the tolerance of my other colleagues at Queen Square and Great Ormond Street Hospital that have accommodated in different ways. The dietetic experience of Maggie Lilburn has been invaluable to this work. Simon Eaton has helped tremendously with performing the assays in chapter 5. I would also like to thank, David Morley, Amy Cole, Martin Christian, and Bridget Wilcken for their constructive thoughts. None of this work would have been possible without the Murphy family’s generous support. I thank the Dromintee Trust for keeping me in worthwhile employment. I would like to thank the patients who volunteered and gave me so much of their time. The Association for Glycogen Storage Disease (UK), Glycologic Ltd and Vitaflo Ltd have also sponsored these trials and hopefully facilitated a better experience for patients. -

6 the Glycogen Storage Diseases and Related Disorders
6 The Glycogen Storage Diseases and Related Disorders G. Peter A. Smit, Jan Peter Rake, Hasan O. Akman, Salvatore DiMauro 6.1 The Liver Glycogenoses – 103 6.1.1 Glycogen Storage Disease Type I (Glucose-6-Phosphatase or Translocase Deficiency) – 103 6.1.2 Glycogen Storage Disease Type III (Debranching Enzyme Deficiency) – 108 6.1.3 Glycogen Storage Disease Type IV (Branching Enzyme Deficiency) – 109 6.1.4 Glycogen Storage Disease Type VI (Glycogen Phosphorylase Deficiency) – 111 6.1.5 Glycogen Storage Disease Type IX (Phosphorylase Kinase Deficiency) – 111 6.1.6 Glycogen Storage Disease Type 0 (Glycogen Synthase Deficiency) – 112 6.2 The Muscle Glycogenoses – 112 6.2.1 Glycogen Storage Disease Type V (Myophosphorylase Deficiency) – 113 6.2.2 Glycogen Storage Disease Type VII (Phosphofructokinase Deficiency) – 113 6.2.3 Phosphoglycerate Kinase Deficiency – 114 6.2.4 Glycogen Storage Disease Type X (Phosphoglycerate Mutase Deficiency) – 114 6.2.5 Glycogen Storage Disease Type XII (Aldolase A Deficiency) – 114 6.2.6 Glycogen Storage Disease Type XIII (E-Enolase Deficiency) – 115 6.2.7 Glycogen Storage Disease Type XI (Lactate Dehydrogenase Deficiency) – 115 6.2.8 Muscle Glycogen Storage Disease Type 0 (Glycogen Synthase Deficiency) – 115 6.3 The Generalized Glycogenoses and Related Disorders – 115 6.3.1 Glycogen Storage Disease Type II (Acid Maltase Deficiency) – 115 6.3.2 Danon Disease – 116 6.3.3 Lafora Disease – 116 References – 116 102 Chapter 6 · The Glycogen Storage Diseases and Related Disorders Glycogen Metabolism Glycogen is a macromolecule composed of glucose viding glucose and glycolytic intermediates (. Fig. 6.1). units. -

Glycogen Storage Diseases Are Genetic Deficiencies That Result in the Storage of Abnormal Amounts of Glycogen in the Body
UNDERSTANDING GLYCOGEN STORAGE DISEASE What is Glycogen Storage Disease? Glycogen storage diseases are genetic deficiencies that result in the storage of abnormal amounts of glycogen in the body. About 1 out of 100 000 babies are born with glycogen storage diseases each year in Canada. There are 5 different types of these diseases depending on the enzyme missing, however, only type 1a will be described here. All people who are born with GSD have one thing in common. They are unable to properly metabolize or break down glycogen, the storage form of sugar in the body. The food we eat is usually used for growth, tissue repair and energy. The body stores what it does not use. Excess sugar, or glucose, is stored as glycogen in the liver and muscle tissue. Between meals and during sleep (i.e. periods of fasting), or during exercise, the body breaks down glycogen and uses the stored sugar for energy. Due to an enzyme deficiency, people with GSD have the ability to store sugar as glycogen but are unable to use these stores to provide the body with energy during fasting or exercise. Think of a pantry where extra food is stored. In times of need, the pantry door can be opened and food can be accessed. In glycogen storage disease, food can be placed in the pantry for storage, but can’t be accessed in times of need. The pantry door is locked. Food can be pushed through a slot in the door but the door cannot be opened to get the food out. -

Advances in Biochemistry & Applications in Medicine
Advances in Biochemistry & Applications in Medicine Chapter 3 Inborn Errors of Metabolism Arvind Kumar Shakya School of Sciences, Indira Gandhi National Open University, New Delhi-110068 (India) Tel: 8447106178; Email: [email protected] 1. Introduction Inborn errors of metabolism (IEM) are a group of inherited metabolic disorders leading to enzymatic defects in the human metabolism. As its name implies, inborn errors means birth defects in newborn infants which passed down from family and affecting metabolism. Hence, it is called Inborn errors of metabolism or inherited metabolic disorders. IEM can appear at birth or later in life such as phenylketonuria, albinism, lactose intolerance, gaucher disease, fabry disease etc. IEM refers a condition where in body’s metabolism is affected due to genetic disorders. The cause of IEM is mutations in a gene that code for an enzyme leading to synthe- sis of defective enzyme activity or deficiency of an enzyme that affects the normal function of a metabolic pathway. The main indication of IEM is an excess storage or accumulation of specific metabolites in tissues, organs and blood which further manifest to health diseases. In last decades, several hundreds of different IEM have been identified. Most IEM are rare but some are life threatening. Although, most people do not know what inherited metabolic disor- ders are and may never have heard of them. Therefore, in this chapter, you are going to study the basic concept, genetic basis and metabolic consequences of inborn errors of metabolism. You will learn about metabolic defec- tive enzymes, clinical symptoms, diagnosis, and treatment of metabolic disorders of amino acids, carbohydrates, lipids, purines and pyrimidines. -

Glycogen Storage Disease Type 0
Glycogen storage disease type 0 Description Glycogen storage disease type 0 (also known as GSD 0) is a condition caused by the body's inability to form a complex sugar called glycogen, which is a major source of stored energy in the body. GSD 0 has two types: in muscle GSD 0, glycogen formation in the muscles is impaired, and in liver GSD 0, glycogen formation in the liver is impaired. The signs and symptoms of muscle GSD 0 typically begin in early childhood. Affected individuals often experience muscle pain and weakness or episodes of fainting ( syncope) following moderate physical activity, such as walking up stairs. The loss of consciousness that occurs with fainting typically lasts up to several hours. Some individuals with muscle GSD 0 have a disruption of the heart's normal rhythm ( arrhythmia) known as long QT syndrome. In all affected individuals, muscle GSD 0 impairs the heart's ability to effectively pump blood and increases the risk of cardiac arrest and sudden death, particularly after physical activity. Sudden death from cardiac arrest can occur in childhood or adolescence in people with muscle GSD 0. Individuals with liver GSD 0 usually show signs and symptoms of the disorder in infancy. People with this disorder develop low blood sugar (hypoglycemia) after going long periods of time without food (fasting). Signs of hypoglycemia become apparent when affected infants begin sleeping through the night and stop late-night feedings; these infants exhibit extreme tiredness (lethargy), pale skin (pallor), and nausea. During episodes of fasting, ketone levels in the blood may increase (ketosis). -

15 Disorders of Carbohydrate and Glycogen Metabolism Jan Peter Rake, Gepke Visser, G
15 Disorders of Carbohydrate and Glycogen Metabolism Jan Peter Rake, Gepke Visser, G. Peter A. Smit 15.1 Introduction The disorders described in this chapter have symptoms varying from mild to severe and life-threatening. The symptoms comprise failure to thrive, hep- atomegaly, jaundice and liver failure, hypoglycemia, metabolic acidosis, and (cardio-) myopathy, including muscle pain and exercise intolerance. Four groups of disorders can be distinguished: A. Disorders of galactose metabolism comprise galactokinase deficiency, gal- actose-1-P-uridyl transferase deficiency (classical galactosemia), and UDP- galactose-4-epimerase deficiency. The primary source of dietary galactose is lactose, the sugar in milk. It is present in human and cow’s milk and in most infant formulae. Individuals with one of these enzyme defects are unable to transform galactose into glucose and they accumulate metabolites of galactose after ingesting lactose and/or galactose. Galactitol accumulation accounts for cataract formation. Galactose-1-phosphate is considered to be responsible for the other clinical manifestations, especially liver and kidney failure. Cataracts are the only manifestations of galactose kinase deficiency. The clinical manifestations of classic galactosemia are vomiting, failure to thrive, liver failure with jaundice, kidney failure, cataract, and sepsis, occurring when galactose is introduced in the diet. The severe form of UDP galacose-4-epimerase deficiency resembles classic galactosemia. The main goal of treatment for galactokinase deficiency (more liberal) and classic galactosemia (strict) is the elimination of galactose from the diet. In severe forms of UDP galactose-4-epimerase deficiency, a narrow balance in dietary galactose requirements for biosynthesis (galactosylated compounds) and excess causing accumulation of galactose-1-phosphate should be aimed for. -

Glycogen Storage Disease Type III
Glycogen storage disease type III Description Glycogen storage disease type III (also known as GSDIII or Cori disease) is an inherited disorder caused by the buildup of a complex sugar called glycogen in the body's cells. The accumulated glycogen is structurally abnormal and impairs the function of certain organs and tissues, especially the liver and muscles. GSDIII is divided into types IIIa, IIIb, IIIc, and IIId, which are distinguished by their pattern of signs and symptoms. GSD types IIIa and IIIc mainly affect the liver and muscles, and GSD types IIIb and IIId typically affect only the liver. It is very difficult to distinguish between the types of GSDIII that affect the same tissues. GSD types IIIa and IIIb are the most common forms of this condition. Beginning in infancy, individuals with any type of GSDIII may have low blood sugar ( hypoglycemia), excess amounts of fats in the blood (hyperlipidemia), and elevated blood levels of liver enzymes. As they get older, children with this condition typically develop an enlarged liver (hepatomegaly). Liver size usually returns to normal during adolescence, but some affected individuals develop chronic liver disease (cirrhosis) and liver failure later in life. People with GSDIII often have slow growth because of their liver problems, which can lead to short stature. In a small percentage of people with GSDIII, noncancerous (benign) tumors called adenomas may form in the liver. Individuals with GSDIIIa may develop muscle weakness (myopathy) later in life. These muscle problems can affect both heart (cardiac) muscle and the muscles that are used for movement (skeletal muscles). -

Review Article
251 Review Article Ana Maria Martins Inborn errors of metabolism: a clinical overview Department of Pediatrics, Universidade Federal de São Paulo/ Escola Paulista de Medicina, São Paulo, Brazil ABSTRACT INTRODUCTION CONTEXT: Inborn errors of metabolism cause hereditary metabolic diseases (HMD) and classically they result from the In 1904 the doctor Archibald E. Garrod lack of activity of one or more specific enzymes or defects in the described alkaptonuria, a disease he classified transportation of proteins. as a lifelong congenital chemical alteration. OBJECTIVES: A clinical review of inborn errors of metabolism (IEM) to give a practical approach to the Later on, in 1909, he described other diseases: physician with figures and tables to help in understanding albinism, cystinuria, porphyria and pentosuria, the more common groups of these disorders. which he named “Inborn Errors of Metabolism”. DATA SOURCE: A systematic review of the clinical and biochemical basis of IEM in the literature, especially Garrod’s conclusions were completely correct considering the last ten years and a classic textbook in relation to the genetic basis of metabolic 1 (Scriver CR et al, 1995). disorders and the gene–enzyme concept. SELECTION OF STUDIES: A selection of 108 references about IEM by experts in the subject was made. Clinical cases According to Scriver, in the foreword of are presented with the peculiar symptoms of various diseases. “Physician’s Guide to the Laboratory Diagnosis 2 DATA SYNTHESIS: IEM are frequently misdiagnosed of Metabolic Diseases”, the importance of because the general practitioner, or pediatrician in the neonatal or intensive care units, does not think about this Garrod’s observation that inborn errors of diagnosis until the more common cause have been ruled out. -
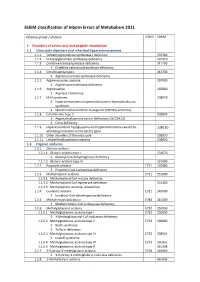
SSIEM Classification of Inborn Errors of Metabolism 2011
SSIEM classification of Inborn Errors of Metabolism 2011 Disease group / disease ICD10 OMIM 1. Disorders of amino acid and peptide metabolism 1.1. Urea cycle disorders and inherited hyperammonaemias 1.1.1. Carbamoylphosphate synthetase I deficiency 237300 1.1.2. N-Acetylglutamate synthetase deficiency 237310 1.1.3. Ornithine transcarbamylase deficiency 311250 S Ornithine carbamoyltransferase deficiency 1.1.4. Citrullinaemia type1 215700 S Argininosuccinate synthetase deficiency 1.1.5. Argininosuccinic aciduria 207900 S Argininosuccinate lyase deficiency 1.1.6. Argininaemia 207800 S Arginase I deficiency 1.1.7. HHH syndrome 238970 S Hyperammonaemia-hyperornithinaemia-homocitrullinuria syndrome S Mitochondrial ornithine transporter (ORNT1) deficiency 1.1.8. Citrullinemia Type 2 603859 S Aspartate glutamate carrier deficiency ( SLC25A13) S Citrin deficiency 1.1.9. Hyperinsulinemic hypoglycemia and hyperammonemia caused by 138130 activating mutations in the GLUD1 gene 1.1.10. Other disorders of the urea cycle 238970 1.1.11. Unspecified hyperammonaemia 238970 1.2. Organic acidurias 1.2.1. Glutaric aciduria 1.2.1.1. Glutaric aciduria type I 231670 S Glutaryl-CoA dehydrogenase deficiency 1.2.1.2. Glutaric aciduria type III 231690 1.2.2. Propionic aciduria E711 232000 S Propionyl-CoA-Carboxylase deficiency 1.2.3. Methylmalonic aciduria E711 251000 1.2.3.1. Methylmalonyl-CoA mutase deficiency 1.2.3.2. Methylmalonyl-CoA epimerase deficiency 251120 1.2.3.3. Methylmalonic aciduria, unspecified 1.2.4. Isovaleric aciduria E711 243500 S Isovaleryl-CoA dehydrogenase deficiency 1.2.5. Methylcrotonylglycinuria E744 210200 S Methylcrotonyl-CoA carboxylase deficiency 1.2.6. Methylglutaconic aciduria E712 250950 1.2.6.1. Methylglutaconic aciduria type I E712 250950 S 3-Methylglutaconyl-CoA hydratase deficiency 1.2.6.2. -

Metabolic Disorders and Molecular Background of Urolithiasis in Childhood B
Scanning Microscopy Vol. 13, No. 2-3, 1999 (Pages 267-280) 0891-7035/99$5.00+.25 Scanning Microscopy International, ChicagoMolecular (AMF mechanisms O’Hare), IL of60666 childhood USA urolithiasis METABOLIC DISORDERS AND MOLECULAR BACKGROUND OF UROLITHIASIS IN CHILDHOOD B. Hoppe1,* and A. Hesse2 1Northwestern University, Children’s Memorial Hospital, Chicago, IL 60614 2Division of Experimental Urology, Department of Urology, University of Bonn, Germany (Received for publication March 29, 1997 and in revised form August 15, 1997) Abstract Introduction Urolithiasis in childhood is less frequently observed than Interesting advances in the understanding of the in adults, but it still has a considerable morbidity. In contrast pathophysiology and the molecular mechanisms of uro- to the situation in adults, an infectious or metabolic cause lithiasis have been made during the last few years. Al- for stone formation is detected in the majority of pediatric though some of the molecular mechanisms found, have come patients. The underlying molecular mechanism of from studies in pediatric patients, they turn out to be urolithiasis has been shown in a number of conditions, and important for all groups of patients. Due to our better some of them have been discovered in pediatric patients. knowledge of both the metabolic basis and the molecular Mutations of the AGXT-gene (2q37.3) have been found to mechanism of stone disease, the management and treatment be responsible for the enzyme defect in primary has been greatly improved. hyperoxaluria type I, and two of the genes provoking Urolithiasis in children is far less common than in cystinuria have been identified (type I: 2p21, type III: adults, but still has a considerable morbidity [13]. -

Download Download
jrenhep.com codonpublications.com REVIEW ARTICLE Liver Transplantation for Monogenic Metabolic Diseases Involving the Kidney Maurizio Salvadori1, Aris Tsalouchos2 1Renal Unit Careggi University Hospital, Viale Pieraccini, Florence, Italy; 2Division of Nephrology, Azienda Ospedaliera Careggi, Largo Alessandro Brambilla, Florence, Italy Abstract Several metabolic monogenic diseases may be cured by liver transplantation alone (LTA) or by combined liver–kidney transplan- tation (CLKT) when the metabolic disease has caused end-stage renal disease. Liver transplantation may be regarded as a substi- tute for an injured liver or as supplying a tissue that may replace a mutant protein. Two groups of diseases should be distinguished. In the first group, the kidney tissue may be severely damaged while the liver tissue is almost normal. In this group, renal transplan- tation is recommended according to the degree of renal damage and liver transplantation is essential as a genetic therapy for correcting the metabolic disorder. In the second group, the liver parenchymal damage is severe. In this group, liver transplanta- tion is essential to avoid liver failure. LTA may also avoid the progression of the renal disease; otherwise a CLKT is needed. In this review, we describe monogenic metabolic diseases involving the kidney that may have beneficial effects from LTA or CLKT. We also highlight the limitations of such procedures and the choice of alternative medical conservative treatments. Keywords: atypical hemolytic uremic syndrome; glycogen storage disease; monogenic metabolic diseases; organic acidurias; primary hyperoxaluria Received: 23 May 2017; Accepted after revision: 26 June 2017; Published: 19 July 2017. Author for correspondence: Maurizio Salvadori, Renal Unit Careggi University Hospital, Viale Pieraccini, 18, 50139, Florence, Italy.