Exploring Prokaryotic and Eukaryotic Microbiomes Helps in Detecting Tick-Borne Infectious Agents in the Blood of Camels
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Babesia Species
Laboratory diagnosis of babesiosis Babesia species Basic guidelines A. Capillary blood should be obtained by fingerstick, or venous blood should be obtained by venipuncture. B. Blood smears, at least two thick and two thin, should be prepared as soon as possible after col- lection. Delay in preparation of the smears can result in changes in parasite morphology and staining characteristics. In Babesia infections, infected red blood cells (rbcs) are normal in size. Typically rings are seen, and they may be vacuolated, pleomorphic or pyriform. Extracellular or tetrad-forms may also be present. Unlike Plasmodium spp., Babesia organisms lack pigment. Rings Rings of Babesia spp. have delicate cytoplasm and are often pleomorphic. Infected rbcs are not enlarged; multiple infection of rbcs can be common. Rings are usually vacuolated and do not produce pigment. Oc- casional classic tetrad-forms (Maltese Cross) or extracellular rings can be present. Rings of Babesia sp. in thick blood smears. Thin, delicate rings of Babesia sp. in a Babesia sp. in a thin blood smear, Thin blood smear showing a cluster of thin blood smear. showing pleomorphic rings and multiply- extracellular rings. infected rbcs. Laboratory diagnosis of babesiosis Babesia species Babesia microti in a thin blood smear. Note Babesia microti in thin blood smears. Notice the vacuolated and pleomorphic rings and multi- the classic “Maltese Cross” tetrad-form in ply-infected rbcs. Notice also there is no pigment present in any of the parasites. the infected rbc in the lower part of the image. Babesia sp. in a thin blood smear stained with Giemsa, showing pleomorphic rings and Babesia sp. -

Seed Plant Models
Review Tansley insight Why we need more non-seed plant models Author for correspondence: Stefan A. Rensing1,2 Stefan A. Rensing 1 2 Tel: +49 6421 28 21940 Faculty of Biology, University of Marburg, Karl-von-Frisch-Str. 8, 35043 Marburg, Germany; BIOSS Biological Signalling Studies, Email: stefan.rensing@biologie. University of Freiburg, Sch€anzlestraße 18, 79104 Freiburg, Germany uni-marburg.de Received: 30 October 2016 Accepted: 18 December 2016 Contents Summary 1 V. What do we need? 4 I. Introduction 1 VI. Conclusions 5 II. Evo-devo: inference of how plants evolved 2 Acknowledgements 5 III. We need more diversity 2 References 5 IV. Genomes are necessary, but not sufficient 3 Summary New Phytologist (2017) Out of a hundred sequenced and published land plant genomes, four are not of flowering plants. doi: 10.1111/nph.14464 This severely skewed taxonomic sampling hinders our comprehension of land plant evolution at large. Moreover, most genetically accessible model species are flowering plants as well. If we are Key words: Charophyta, evolution, fern, to gain a deeper understanding of how plants evolved and still evolve, and which of their hornwort, liverwort, moss, Streptophyta. developmental patterns are ancestral or derived, we need to study a more diverse set of plants. Here, I thus argue that we need to sequence genomes of so far neglected lineages, and that we need to develop more non-seed plant model species. revealed much, the exact branching order and evolution of the I. Introduction nonbilaterian lineages is still disputed (Lanna, 2015). Research on animals has for a long time relied on a number of The first (small) plant genome to be sequenced was of THE traditional model organisms, such as mouse, fruit fly, zebrafish or model plant, the weed Arabidopsis thaliana (c. -

And Toxoplasmosis in Jackass Penguins in South Africa
IMMUNOLOGICAL SURVEY OF BABESIOSIS (BABESIA PEIRCEI) AND TOXOPLASMOSIS IN JACKASS PENGUINS IN SOUTH AFRICA GRACZYK T.K.', B1~OSSY J.].", SA DERS M.L. ', D UBEY J.P.···, PLOS A .. ••• & STOSKOPF M. K .. •••• Sununary : ReSlIlIle: E x-I1V\c n oN l~ lIrIUSATION D'Ar\'"TIGENE DE B ;IB£,'lA PH/Re El EN ELISA ET simoNi,cATIVlTli t'OUR 7 bxo l'l.ASMA GONIJfI DE SI'I-IENICUS was extracted from nucleated erythrocytes Babesia peircei of IJEMIiNSUS EN ArRIQUE D U SUD naturally infected Jackass penguin (Spheniscus demersus) from South Africo (SA). Babesia peircei glycoprotein·enriched fractions Babesia peircei a ele extra it d 'erythrocytes nue/fies p,ovenanl de Sphenicus demersus originoires d 'Afrique du Sud infectes were obto ined by conca navalin A-Sepharose affinity column natulellement. Des fractions de Babesia peircei enrichies en chromatogrophy and separated by sod ium dodecyl sulphate glycoproleines onl ele oblenues par chromatographie sur colonne polyacrylam ide gel electrophoresis (SDS-PAGE ). At least d 'alfinite concona valine A-Sephorose et separees par 14 protein bonds (9, 11, 13, 20, 22, 23, 24, 43, 62, 90, electrophorese en gel de polyacrylamide-dodecylsuJfale de sodium 120, 204, and 205 kDa) were observed, with the major protein (SOS'PAGE) Q uotorze bandes proleiques au minimum ont ete at 25 kDa. Blood samples of 191 adult S. demersus were tes ted observees (9, 1 I, 13, 20, 22, 23, 24, 43, 62, 90, 120, 204, by enzyme-linked immunosorbent assoy (ELISA) utilizing B. peircei et 205 Wa), 10 proleine ma;eure elant de 25 Wo. -

A Comparative Genomic Study of Attenuated and Virulent Strains of Babesia Bigemina
pathogens Communication A Comparative Genomic Study of Attenuated and Virulent Strains of Babesia bigemina Bernardo Sachman-Ruiz 1 , Luis Lozano 2, José J. Lira 1, Grecia Martínez 1 , Carmen Rojas 1 , J. Antonio Álvarez 1 and Julio V. Figueroa 1,* 1 CENID-Salud Animal e Inocuidad, Instituto Nacional de Investigaciones Forestales Agrícolas y Pecuarias, Jiutepec, Morelos 62550, Mexico; [email protected] (B.S.-R.); [email protected] (J.J.L.); [email protected] (G.M.); [email protected] (C.R.); [email protected] (J.A.Á.) 2 Centro de Ciencias Genómicas, Universidad Nacional Autónoma de México, AP565-A Cuernavaca, Morelos 62210, Mexico; [email protected] * Correspondence: fi[email protected]; Tel.: +52-777-320-5544 Abstract: Cattle babesiosis is a socio-economically important tick-borne disease caused by Apicom- plexa protozoa of the genus Babesia that are obligate intraerythrocytic parasites. The pathogenicity of Babesia parasites for cattle is determined by the interaction with the host immune system and the presence of the parasite’s virulence genes. A Babesia bigemina strain that has been maintained under a microaerophilic stationary phase in in vitro culture conditions for several years in the laboratory lost virulence for the bovine host and the capacity for being transmitted by the tick vector. In this study, we compared the virulome of the in vitro culture attenuated Babesia bigemina strain (S) and the virulent tick transmitted parental Mexican B. bigemina strain (M). Preliminary results obtained by using the Basic Local Alignment Search Tool (BLAST) showed that out of 27 virulence genes described Citation: Sachman-Ruiz, B.; Lozano, and analyzed in the B. -

Download Fall 2020
CHEMISTRY ELEMENTS A Publication of the Department of Chemistry at Illinois Tech Fall 2020 Letter from the Chair opportunity to our young chemists. We members: Professor Joy Chong received have solicited our very own Chemistry a four-year National Institutes of Health Alumni Ambassadors who will help us grant for her project titled “Development with local area high school recruitment of Superior Chelation Chemistry for 89Zr- at their respective schools, as well as ImmunoPET Imaging,” and Assistant career counseling for our prospective Professor Andrey Rogachev received an students. While we continue to have a ACS-PRF (Petroleum Research Fund) larger incoming undergraduate population grant award for his work titled “Deep in recent years as compared to previous Understanding of Catalytic Activity through years, we are determined to focus on High-Level Calculations.” building our undergraduate programs even more. Due to the pandemic, we had to postpone the 39th Kilpatrick Lecture to a future Many thanks to Bob Frey (CHEM ’65) for date—stay tuned. creating the Robert E. Frey Jr. Endowed Term Chair in Chemistry, which was As an African proverb says, “Smooth awarded to Associate Professor David seas do not make skillful sailors.” It’s Minh. Congratulations to David for achieving the hard knocks in life that shape us into the first endowed chair position in the something stronger, wiser, and more Department of Chemistry’s recent history. resilient. We are getting through this tough time together. We hope all is well with you We want to also thank alumnus Ted and your families. We want to thank you Brown (CHEM ’50) for initiating the for your continued support and loyalty. -

Women, Business and the Law 2020 World Bank Group
WOMEN, BUSINESS AND THE LAW 2020 AND THE LAW BUSINESS WOMEN, WOMEN, BUSINESS AND THE LAW 2020 WORLD BANK GROUP WORLD WOMEN, BUSINESS AND THE LAW 2020 © 2020 International Bank for Reconstruction and Development / The World Bank 1818 H Street NW, Washington, DC 20433 Telephone: 202-473-1000; Internet: www.worldbank.org Some rights reserved 1 2 3 4 23 22 21 20 This work is a product of the staff of The World Bank with external contributions. The findings, interpretations, and conclusions expressed in this work do not necessarily reflect the views of The World Bank, its Board of Executive Directors, or the govern- ments they represent. The World Bank does not guarantee the accuracy of the data included in this work. The boundaries, colors, denominations, and other information shown on any map in this work do not imply any judgment on the part of The World Bank concerning the legal status of any territory or the endorsement or acceptance of such boundaries. Nothing herein shall constitute or be considered to be a limitation upon or waiver of the privileges and immunities of The World Bank, all of which are specifically reserved. Rights and Permissions This work is available under the Creative Commons Attribution 3.0 IGO license (CC BY 3.0 IGO) http://creativecommons.org/ licenses/by/3.0/igo. Under the Creative Commons Attribution license, you are free to copy, distribute, transmit, and adapt this work, including for commercial purposes, under the following conditions: Attribution—Please cite the work as follows: World Bank. 2020. Women, Business and the Law 2020. -
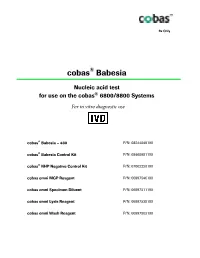
Package Insert
Rx Only ® cobas Babesia Nucleic acid test ® for use on the cobas 6800/8800 Systems For in vitro diagnostic use ® cobas Babesia – 480 P/N: 08244049190 cobas® Babesia Control Kit P/N: 08460981190 cobas® NHP Negative Control Kit P/N: 07002220190 cobas omni MGP Reagent P/N: 06997546190 cobas omni Specimen Diluent P/N: 06997511190 cobas omni Lysis Reagent P/N: 06997538190 cobas omni Wash Reagent P/N: 06997503190 cobas® Babesia Table of contents Intended use ............................................................................................................................ 4 Summary and explanation of the test ................................................................................. 4 Reagents and materials ......................................................................................................... 7 cobas® Babesia reagents and controls ....................................................................................................... 7 cobas omni reagents for sample preparation ........................................................................................ 10 Reagent storage and handling requirements ......................................................................................... 11 Additional materials required ................................................................................................................. 12 Instrumentation and software required ................................................................................................. 12 Precautions and handling requirements -

Tutorial in English, Based on the Introduction of Islam
CENTRAL MUSLIM SPIRITUAL BOARD RUSSIA RUSSIAN ISLAMIC UNIVERSITY TUTORIAL IN ENGLISH, BASED ON THE INTRODUCTION OF ISLAM Initial training for educational institutions of secondary and higher level UFA, 2011 Published by the decision of the Editorial Board of the Russian Islamic University (Ufa) Tutorial in English, based on the introduction of Islam. - Ufa Publishing Division of the Russian Islamic University, 2011. - 000 pages. The book contains a mandatory minimum of knowledge, which every Muslim must possess: knowledge of the faith and order of worship to Allah. The book is intended for a wide range of readers. TsDUM Russia, 2011 PREFACE Endless thanks and praise to Allah the Most High, Who has created mankind and the entire universe with divine wisdom and for a great purpose. May blessings and peace be upon Muhammad, the means of compassion to the universe, the most distinguished intercessor and the most beloved Prophet of Allah the Lord, upon his family, upon his companions and upon all those who have followed and continue to follow his holy path. The content of this Introduction to Islam pertains to a branch of Islamic knowledge that provides information about faith (iman) and worship (ibadah). Muhammad, peace and blessings be upon him (Sallallahu 'alayhi wa-sallam)1, said that it is compulsory for every Muslim man and woman to acquire knowledge. The knowledge (Introduction to Islam) in this manual gives essential information about faith (iman) and worship (ibadah) which will guide its adherent to happiness both in this world and in the Hereafter. One cannot become a complete and perfect Muslim without learning and believing these essentials, known in Arabic as Dharurah-al-Diniyyah (Necessary Rules of Religion). -

Novel and Rapidly Diverging Intergenic Sequences Between Tandem Repeats of the Luciferase Genes in Seven Dinoflagellate Species1
J. Phycol. 42, 96–103 (2005) r 2005 Phycological Society of America DOI: 10.1111/j.1529-8817.2005.00165.x NOVEL AND RAPIDLY DIVERGING INTERGENIC SEQUENCES BETWEEN TANDEM REPEATS OF THE LUCIFERASE GENES IN SEVEN DINOFLAGELLATE SPECIES1 Liyun Liu and J. Woodland Hastings2 Department of Molecular and Cellular Biology, Harvard University, 16 Divinity Avenue, Cambridge, Massachusetts 02138, USA Tandemly arranged luciferase genes were previ- Our previous studies of the structure of dinoflagel- ously reported in two dinoflagellates species, but lates genes and their circadian regulation revealed that their intergenic regions were strikingly different several occur in tandemly arranged copies (Le et al. and no canonical promoter sequences were found. 1997, Li and Hastings 1998, Okamoto et al. 2001). Here, we examined the intergenic regions of the Other than for ribosomal genes (Sollner-Webb and luciferase genes of five other dinoflagellate species Tower 1986) and a few protein-coding genes in two along with those of the earlier two. In all cases, the protozoa, Trypanosoma brucei and Babesia bovis (Lee and genes exist in multiple copies and are arranged Van der Ploeg 1997, Suarez et al. 1998), such an ar- tandemly, coding for proteins of similar sizes and rangement is not known in other eukaryotes. Indeed, sequences. However, the 50 untranslated region, 30 it is well known that the dinoflagellate nucleus is very untranslated region, and intergenic regions of the unusual; its envelope remains intact throughout the seven genes differ greatly in length and sequence, cell cycle, with the separation of the chromosomes in except for two stretches that are conserved in the mitosis being carried out by an external mitotic spindle intergenic regions of two pairs of phylogenetically (Taylor 1987). -

Huda Essa Culturelinksllc.Com Jot Down Questions to Be Answered at Q & a Time! Middle Eastern, Arabic, Arabs, Muslims, ???…
Huda Essa culturelinksllc.com Jot down questions to be answered at Q & A time! Middle Eastern, Arabic, Arabs, Muslims, ???… • Arab = Person with origins from Arab country • Arabic = language • Middle Eastern = Region (Western Asia) • Muslim = One who practices religion of Islam The Arab World •Over 400 Million People •Collective cultural, ethnic, and national Arab Identity Religious Identity of Arabs • Numerous religions and ethnic groups in Arab World • Islam, Judaism and Christianity all originated inside Arab world Arabic English • Adam • Shuaib = Jethro • Daniel • Musa = Moses • Hud • Harun = Aaron • Sara • Dzulkifil = Ezekial • Idris = Enoch • Dawud = David • Noah = Nuh • Sulaiman = Soloman • Shaleh = Saleh • Ilyas = Elijah • Ibrahim = Abraham • Alyas’a = Elisha • Lut = Lot • Younes = Jonah • Ismail = Ishmael • Zakaria = Zachariah • Ishaq = Issac • Yahya = John • Yaqub = Jacob • Issa = Jesus • Yousef = Joseph • Mariam = Mary • Ayyub = Job • Hajar = Hagar Diversity of Muslims in America - Institute for Social Policy and Understanding, 2016 Majority of comparison are similarities, such as… •Honesty, common good, respect, charity, etc. •One God as the creator and sustainer of the universe •10 Commandments •Old testament/Torah, New testament/Gospel are holy scriptures •God sent prophets as messengers to mankind – Moral teachings of prophets Furthermore…. • Mary, the mother of Jesus, was a virgin; Jesus was born miraculously • Jesus is the Messiah and he performed miracles • An Anti-Christ will appear on Earth before the Day of Judgment -

Stories of the Prophets
Stories of the Prophets Written by Al-Imam ibn Kathir Translated by Muhammad Mustapha Geme’ah, Al-Azhar Stories of the Prophets Al-Imam ibn Kathir Contents 1. Prophet Adam 2. Prophet Idris (Enoch) 3. Prophet Nuh (Noah) 4. Prophet Hud 5. Prophet Salih 6. Prophet Ibrahim (Abraham) 7. Prophet Isma'il (Ishmael) 8. Prophet Ishaq (Isaac) 9. Prophet Yaqub (Jacob) 10. Prophet Lot (Lot) 11. Prophet Shuaib 12. Prophet Yusuf (Joseph) 13. Prophet Ayoub (Job) 14 . Prophet Dhul-Kifl 15. Prophet Yunus (Jonah) 16. Prophet Musa (Moses) & Harun (Aaron) 17. Prophet Hizqeel (Ezekiel) 18. Prophet Elyas (Elisha) 19. Prophet Shammil (Samuel) 20. Prophet Dawud (David) 21. Prophet Sulaiman (Soloman) 22. Prophet Shia (Isaiah) 23. Prophet Aramaya (Jeremiah) 24. Prophet Daniel 25. Prophet Uzair (Ezra) 26. Prophet Zakariyah (Zechariah) 27. Prophet Yahya (John) 28. Prophet Isa (Jesus) 29. Prophet Muhammad Prophet Adam Informing the Angels About Adam Allah the Almighty revealed: "Remember when your Lord said to the angels: 'Verily, I am going to place mankind generations after generations on earth.' They said: 'Will You place therein those who will make mischief therein and shed blood, while we glorify You with praises and thanks (exalted be You above all that they associate with You as partners) and sanctify You.' Allah said: 'I know that which you do not know.' Allah taught Adam all the names of everything, then He showed them to the angels and said: "Tell Me the names of these if you are truthful." They (angels) said: "Glory be to You, we have no knowledge except what You have taught us. -

Equine Piroplasmosis
EAZWV Transmissible Disease Fact Sheet Sheet No. 119 EQUINE PIROPLASMOSIS ANIMAL TRANS- CLINICAL SIGNS FATAL TREATMENT PREVENTION GROUP MISSION DISEASE ? & CONTROL AFFECTED Equines Tick-borne Acute, subacute Sometimes Babesiosis: In houses or chronic disease fatal, in Imidocarb Tick control characterised by particular in (Imizol, erythrolysis: fever, acute T.equi Carbesia, in zoos progressive infections. Forray) Tick control anaemia, icterus, When Dimenazene haemoglobinuria haemoglobinuria diaceturate (in advanced develops, (Berenil) stages). prognosis is Theileriosis: poor. Buparvaquone (Butalex) Fact sheet compiled by Last update J. Brandt, Royal Zoological Society of Antwerp, February 2009 Belgium Fact sheet reviewed by D. Geysen, Animal Health, Institute of Tropical Medicine, Antwerp, Belgium F. Vercammen, Royal Zoological Society of Antwerp, Belgium Susceptible animal groups Horse (Equus caballus), donkey (Equus asinus), mule, zebra (Equus zebra) and Przewalski (Equus przewalskii), likely all Equus spp. are susceptible to equine piroplasmosis or biliary fever. Causative organism Babesia caballi: belonging to the phylum of the Apicomplexa, order Piroplasmida, family Babesiidae; Theileria equi, formerly known as Babesia equi or Nutallia equi, apicomplexa, order Piroplasmida, family Theileriidae. Babesia canis has been demonstrated by molecular diagnosis in apparently asymptomatic horses. A single case of Babesia bovis and two cases of Babesia bigemina have been detected in horses by a quantitative PCR. Zoonotic potential Equine piroplasmoses are specific for Equus spp. yet there are some reports of T.equi in asymptomatic dogs. Distribution Widespread: B.caballi occurs in southern Europe, Russia, Asia, Africa, South and Central America and the southern states of the US. T.equi has a more extended geographical distribution and even in tropical regions it occurs more frequent than B.caballi, also in the Mediterranean basin, Switzerland and the SW of France.