Signs and Symptoms of a Chest Infection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Keeping Your Gut in Check Healthy Options to Stay on Tract Your Digestive System Is Busy
May 2017 National Institutes of Health • Department of Health and Human Services • newsinhealth.nih.gov Inside News: 3 Bronchitis vs. Pneumonia... 4 Eating Habits and Disease... Spanish Health Materials... Human Genome Keeping Your Gut in Check Healthy Options to Stay on Tract Your digestive system is busy. What you eat can help or When you eat something, your hurt your digestive system, and food takes a twisty trip that influence how you feel. “Increas- starts with being chewed up ing fiber is really important for and ends with you going to constipation,” says Chang. “Most the bathroom. A lot happens in Americans do not eat a lot of between. The health of your gut fiber so you have to gradually plays a key role in your overall increase the fiber in your diet. health and well-being. You can Otherwise you might get gas make choices to help your body and more bloating, and won’t stay on tract. stick with [the changes].” Your digestive, or Chang says you should eat at gastrointestinal (GI), tract is a least 20–30 grams of fiber a day long, muscular tube that runs for constipation. You can spread from your mouth to your anus. out your fiber in small amounts It’s about 30 feet long and throughout the day. Start with works with other parts of your small servings and gradually digestive system to break food increase them to avoid gas, and drink down into smaller bloating, and discomfort. molecules of nutrients. The Try to eat fruits and vege- blood absorbs these and carries them Chang, a GI expert at the University tables at every meal. -

Use of Natural Colours in the Ice Cream Industry
USE OF NATURAL COLOURS IN THE ICE CREAM INDUSTRY Dr. Juan Mario Sanz Penella Dr. Emanuele Pedrazzini Dr. José García Reverter SECNA NATURAL INGREDIENTS GROUP Definition of ice cream Ice cream is a frozen dessert, a term that includes different types of product that are consumed frozen and that includes sorbets, frozen yogurts, non-dairy frozen desserts and, of course, ice cream. In order to simplify its classification, we can consider for practical purposes two different types of frozen desserts: ice cream and sorbets. Ice cream includes all products that have a neutral pH and contain dairy ingredients. While sorbet refers to products with an acidic pH, made with water and other ingredients such as fruit, but without the use of dairy. Additionally, when referring to ice cream, we are not referring to a single type of product, we are actually referring to a wide range of these. Ice cream is a food in which the three states of matter coexist, namely: water in liquid form and as ice crystals, sugars, fats and proteins in solid form and occluded air bubbles in gaseous form, Figure 1. Artisanal ice creams based on natural ingredients which give it its special texture. It should be noted that ice cream is a very complete food from a nutritional point of view since it incorporates in its formulation a wide range of ingredients (sugars, milk, fruits, egg products ...) essential for a balanced diet. Another aspect of great relevance in the manufacture of ice cream is the hedonic factor. Ice cream is consumed mainly for the pure pleasure of tasting it, the hedonic component being the main factor that triggers its consumption, considering its formulation and design a series of strategies to evoke a full range of sensations: gustatory, olfactory, visual and even, of the touch and the ear. -

Chest Pain and Non-Respiratory Symptoms in Acute Asthma
Postgrad Med J 2000;76:413–414 413 Chest pain and non-respiratory symptoms in Postgrad Med J: first published as 10.1136/pmj.76.897.413 on 1 July 2000. Downloaded from acute asthma W M Edmondstone Abstract textbooks. Occasionally the combination of The frequency and characteristics of chest dyspnoea and chest pain results in diagnostic pain and non-respiratory symptoms were confusion. This study was prompted by the investigated in patients admitted with observation that a number of patients admitted acute asthma. One hundred patients with with asthmatic chest pain had been suspected a mean admission peak flow rate of 38% of having cardiac ischaemia, pleurisy, pericardi- normal or predicted were interviewed tis, or pulmonary embolism. It had also been using a questionnaire. Chest pain oc- observed that many patients admitted with curred in 76% and was characteristically a asthma complained of a range of non- dull ache or sharp, stabbing pain in the respiratory symptoms, something which has sternal/parasternal or subcostal areas, been noted previously in children1 and in adult worsened by coughing, deep inspiration, asthmatics in outpatients.2 The aim of this or movement and improved by sitting study was to examine the frequency and char- upright. It was rated at or greater than acteristics of chest pain and other symptoms in 5/10 in severity by 67% of the patients. A patients admitted with acute asthma. wide variety of upper respiratory and sys- temic symptoms were described both Patients and methods before and during the attack. One hundred patients (66 females, mean (SD) Non-respiratory symptoms occur com- age 45.0 (19.7) years) admitted with acute monly in the prodrome before asthma asthma were studied. -

Eloise Butler Wildflower Garden and Bird Sanctuary
ELOISE BUTLER WILDFLOWER GARDEN AND BIRD SANCTUARY WEEKLY GARDEN HIGHLIGHTS Phenology notes for the week of October 5th – 11th It’s been a relatively warm week here in Minneapolis, with daytime highs ranging from the mid-60s the low 80s. It’s been dry too; scant a drop of rain fell over the past week. The comfortable weather was pristine for viewing the Garden’s fantastic fall foliage. Having achieved peak color, the Garden showed shades of amber, auburn, beige, blond, brick, bronze, brown, buff, burgundy, canary, carob, castor, celadon, cherry, cinnabar, claret, clay, copper, coral, cream, crimson, ecru, filemont, fuchsia, gamboge, garnet, gold, greige, khaki, lavender, lilac, lime, magenta, maroon, mauve, meline, ochre, orange, peach, periwinkle, pewter, pink, plum, primrose, puce, purple, red, rose, roseate, rouge, rubious, ruby, ruddy, rufous, russet, rust, saffron, salmon, scarlet, sepia, tangerine, taup, tawny, terra-cotta, titian, umber, violet, yellow, and xanthic, to name a few. According to the Minnesota Department of Natural Resources, the northern two thirds of the state reached peak color earlier in 2020 than it did in both 2019 and 2018, likely due to a relatively cool and dry September. Many garter snakes have been seen slithering through the Garden’s boundless leaf litter. Particularly active this time of year, snakes must carefully prepare for winter. Not only do the serpents need to locate an adequate hibernaculum to pass the winter, but they must also make sure they’ve eaten just the right amount of food. Should they eat too little, they won’t have enough energy to make it through the winter. -

Dye and Gluten Chart
2020 Natural/Artificial Coloring & Gluten Chart Cream Ice Flavors Artificial Coloring Natural Coloring Allergen: Blue #1 Blue #2 Red #3 Red #40 Yellow #5 Yellow #6 Caramel Color Titanium Dioxide Annatto Extract Beta Carotene Turmeric Gluten Banana Split Cream X X X Birthday Cake X X X X Black Cherry Cheesecake X X Brookie Dough X X Caramel (Dulce de Leche) X Cheesecake Chocolate Chip Cheesecake Chocolate-Covered Banana X X Chocolate-Covered Strawberry X Coconut Cream X Cookie Dough X X Fudge Brownie X X Horchata Iced Coffee Marshmallow Peanut Butter X Mint Chocolate Chip X X Mint OREO® X X X Mocha X OREO® Cookies 'n Cream X X Peppermint Chip X X Pumpkin Cheesecake X Pumpkin Pie X Pumpkin Spice Latte X Root Beer Float X S'mores X Strawberry-Banana X X X Strawberry Cheesecake X Vanilla Cream X Watermelon Chip X X Italian Ice Flavors Allergen: Blue #1 Blue #2 Red #3 Red #40 Yellow #5 Yellow #6 Caramel Color Titanium Dioxide Annatto Extract Beta Carotene Turmeric Gluten Apple Berry Blue X X Banana X X Blood Orange X X Blue Raspberry X Blueberry X Cantaloupe X X Cherry Lemonade X Cherry Limeade X Cherry X Chocolate X Chocolate Chocolate Chip X Chocolate Peanut Butter X Cotton Candy X Dr Pepper X Florida Orange X X Georgia Peach X Grape X X Green Apple X X Hawaiian Punch® X X Island Fusion X X X Juicy Pear X X Key Lime X X Kiwi-Strawberry X X X Lemon Mango X X Mango-Orange X X Mango-Peach X X Mango-Pineapple X X Mango-Strawberry X X X Margarita X X Mojito X X Passion Fruit X X Peanut Butter & Jelly X Piña Colada X Pineapple X X Raspberry X -

Influenza (PDF)
INFLUENZA Outbreaks of influenza, or “flu”, typically occur every winter. Colds may occur at any time of year with seasonal peaks occurring in fall and spring. Influenza is a respiratory illness usually caused by infection with one of two influenza viruses – influenza A or influenza B. Outbreaks of influenza (flu) typically occur every winter. Influenza is characterized by an abrupt onset of fever, chills, headache, body aches, and lack of energy accompanied by respiratory symptoms, most frequently cough and sore throat. Most people are largely recovered in one week, although many feel fatigued for several weeks. Serious complications of flu, such as pneumonia, however, can occur, especially if the body’s defenses are weakened by age or disease. Influenza is spread by inhaling the influenza virus which is usually carried on tiny, invisible water droplets in the air generated by coughs and sneezes. Hand-to-hand contact as well as contact with infected secretions on a hard surface may also cause transmission of the virus. Each year influenza viruses change and new vaccines are made to combat the particular strains that are expected to cause illness that year. The flu vaccine may reduce the chance of getting the flu by 60-80%, and lessen the severity of illness in the person who does get the flu. According to the Centers for Disease Control (CDC), everyone 6 months or order should get a yearly flu vaccine. The following people are at high risk for complications of flu and are especially urged to get vaccinated: Individuals with chronic heart or lung problems that have required regular medical follow-up or hospitalization during the last year. -
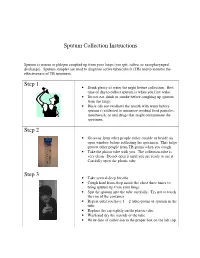
Sputum Collection Instructions Step 1 Step 2 Step 3
Sputum Collection Instructions Sputum is mucus or phlegm coughed up from your lungs (not spit, saliva, or nasopharyngeal discharge). Sputum samples are used to diagnose active tuberculosis (TB) and to monitor the effectiveness of TB treatment. Step 1 • Drink plenty of water the night before collection. Best time of day to collect sputum is when you first wake. • Do not eat, drink or smoke before coughing up sputum from the lungs. • Rinse (do not swallow) the mouth with water before sputum is collected to minimize residual food particles, mouthwash, or oral drugs that might contaminate the specimen. Step 2 • Go away from other people either outside or beside an open window before collecting the specimen. This helps protect other people from TB germs when you cough. • Take the plastic tube with you. The collection tube is very clean. Do not open it until you are ready to use it. Carefully open the plastic tube. Step 3 • Take several deep breaths. • Cough hard from deep inside the chest three times to bring sputum up from your lungs. • Spit the sputum into the tube carefully. Try not to touch the rim of the container. • Repeat until you have 1 – 2 tablespoons of sputum in the tube. • Replace the cap tightly on the plastic tube. • Wash and dry the outside of the tube. • Write date of collection in the proper box on the lab slip. Step 4 • Place the primary specimen container (usually a conical centrifuge tube) in the clear plastic baggie that has the biohazard symbol imprint. • Place the white absorbent sheet in the plastic baggie. -

Perinatal/Neonatal Case Presentation
Perinatal/Neonatal Case Presentation &&&&&&&&&&&&&& Urinary Tract Infection With Trichomonas vaginalis in a Premature Newborn Infant and the Development of Chronic Lung Disease David J. Hoffman, MD vaginal bleeding with suspected abruption resulted in delivery of Gerard D. Brown, DO the infant by Cesarean section. The Apgar scores were 1, 5, and 9 Frederick H. Wirth, MD at 1, 5, and 10 minutes of life, respectively. Betsy S. Gebert, CRNP After delivery, the infant was managed with mechanical Cathy L. Bailey, MS, CRNP ventilation with pressure support and volume guarantee for Endla K. Anday, MD respiratory distress syndrome. She received exogenous surfactant We report a case of a low-birth-weight infant with an infection of the urinary tract with Trichomonas vaginalis, who later developed cystic chronic lung disease suggestive of Wilson-Mikity syndrome. Although she had mild respiratory distress syndrome at birth, the extent of the chronic lung disease was out of proportion to the initial illness. We speculate that maternal infection with this organism may have resulted in an inflammatory response that led to its development. Journal of Perinatology (2003) 23, 59 – 61 doi:10.1038/sj.jp.7210819 CASE PRESENTATION A 956-g, appropriate-for-gestational-age, African–American female was delivered by Cesarean section following 27 5/7 weeks of gestation in breech presentation after a period of advanced cervical dilatation and uterine contractions. Her mother was a 20-year-old gravida 5, para 2022 woman whose prenatal laboratory data were significant for vaginal colonization with Streptococcus agalactiae, treatment for Chlamydia trachomatis, and a history of cocaine and marijuana usage confirmed by urine toxicology. -

COPD (Chronic Obstructive Pulmonary Disease)
COPD (Chronic Obstructive Pulmonary Disease) A difficult problem explained in simple language. Introduction The normal lung Lung facts What is COPD? How does COPD damage your health? How can I tell if I am developing COPD? How can we tell if you are developing COPD? What can you do to help yourself? What can we do to help you? Conclusion INTRODUCTION So you want to find out more about the illness that we call COPD. It may be that your doctor has raised some concerns that you might have this condition but has not had a chance to explain what it is. You may have seen something in the press about COPD which describes symptoms that you have been getting such as cough, phlegm and breathlessness or you may have a loved one who is developing these symptoms and you are concerned to find out what the cause is. Make sure you read all the way through to the end of this description and we hope that you will have a much better understanding. The normal lung. As we travel through the voice box (larynx) into the main windpipe (trachea) we find the airways that we pass through get smaller and smaller with increasing numbers of branches until the tiniest tubes open into bubbles whose walls consist of a very fine membrane. These bubbles are arranged in bunches like grapes around which is a lace work of very fine blood vessels. In the healthy lung, when air reaches these bubbles (alveoli), oxygen passes readily through the bubble membrane into the blood stream. -

COVID-19 Infection Versus Influenza (Flu) and Other Respiratory Illnesses
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES PATIENT EDUCATION | INFORMATION SERIES COVID-19 Infection versus Influenza (Flu) and Other Respiratory Illnesses SARS-CoV-2 is the virus that causes the COVID-19 infection. You can be ill with more than one virus at the same time. As the SARS-CoV-2 virus pandemic continues, influenza and other respiratory infections can also be present in the community. Respiratory infections may present with similar symptoms and all can spread from person to person. It is hard to tell which virus or bacteria is causing a person’s illness based on symptoms alone. At times testing is needed to see which virus(es) or bacteria are present. These tests usually involve getting a nose and/or throat swab sample, as most of these viruses are present in large amounts in the back of the nose and throat. There is still a lot to learn about the COVID-19 infection and research is ongoing. You can be ill with more than one virus at the same time. COVID-19). COVID vaccine supplies are limited but When multiple viruses are present the risk of developing increasing. The states control who is eligible and where severe disease increases. Severe disease usually involves vaccines are given. difficulty breathing and getting oxygen into your body. The influenza vaccine covers Flu A and B strains expected Risk factors for severe illness are shown in the table. in each year’s flu season. Getting a flu vaccine each year How are COVID-19 and other respiratory can help protect you and reduce your risk of severe viruses spread? illness. -

Factors Associated with Pleurisy in Pigs: a Case-Control Analysis of Slaughter Pig Data for England and Wales
Aus dem Zentrum für Klinische Tiermedizin der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Arbeit angefertigt unter der Leitung von Prof. Dr. Mathias Ritzmann Angefertigt am Cambridge Infectious Diseases Consortium, University of Cambridge, Department of Veterinary Medicine, Cambridge, UK (Dr. A W (Dan) Tucker) Factors associated with pleurisy in pigs: A case-control analysis of slaughter pig data for England and Wales Inaugural-Dissertation zur Erlangung der tiermedizinischen Doktorwürde der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Von Henrike Caroline Jäger aus Wiesbaden München 2012 Gedruckt mit der Genehmigung der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Dekan: Univ.-Prof. Dr. Joachim Braun Berichterstatter: Univ.-Prof. Dr. Mathias Ritzmann Korreferent: Univ.-Prof. Dr. Dr. habil. Manfred Gareis Tag der Promotion: 9. Februar 2013 Meinem Vater Dr. med Sepp-Dietrich Jäger Table of Contents 4 TABLE OF CONTENTS I. INTRODUCTION ...................................................................................... 7 II. LITERATURE OVERVIEW .................................................................... 8 1. Anatomy and Physiology of the Pleura ....................................................8 2. Pleurisy ........................................................................................................9 2.1. Morphology ..................................................................................................9 2.2. Prevalence ..................................................................................................11 -

Chest Pain in Pediatrics
PEDIATRIC CARDIOLOGY 0031-3955/99 $8.00 + .OO CHEST PAIN IN PEDIATRICS Keith C. Kocis, MD, MS Chest pain is an alarming complaint in children, leading an often frightened and concerned family to a pediatrician or emergency room and commonly to a subsequent referral to a pediatric cardiologist. Because of the well-known associ- ation of chest pain with significant cardiovascular disease and sudden death in adult patients, medical personnel commonly share heightened concerns over pediatric patients presenting with chest pain. Although the differential diagnosis of chest pain is exhaustive, chest pain in children is least likely to be cardiac in origin. Organ systems responsible for causing chest pain in children include*: Idiopathic (12%-85%) Musculoskeletal (15%-31%) Pulmonary (12%-21%) Other (4%-21%) Psychiatric (5%-17%) Gastrointestinal (4'/0-7%) Cardiac (4%4%) Furthermore, chest pain in the pediatric population is rareZy associated with life-threatening disease; however, when present, prompt recognition, diagnostic evaluation, and intervention are necessary to prevent an adverse outcome. This article presents a comprehensive list of differential diagnostic possibilities of chest pain in pediatric patients, discusses the common causes in further detail, and outlines a rational diagnostic evaluation and treatment plan. Chest pain, a common complaint of pediatric patients, is often idiopathic in etiology and commonly chronic in nature. In one study,67 chest pain accounted for 6 in 1000 visits to an urban pediatric emergency room. In addition, chest pain is the second most common reason for referral to pediatric cardiologist^.^, 23, 78 Chest pain is found equally in male and female patients, with an average *References 13, 17, 23, 27, 32, 35, 44, 48, 49, 63-67, 74, and 78.