Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0 Published: May 28, 2009 (V4.03: June 14, 2010)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Vaccine Adverse Event Reporting System (VAERS)
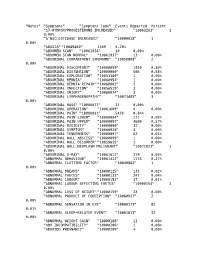
"Notes" "Symptoms" "Symptoms Code" Events Reported Percent "17-HYDROXYPROGESTERONE INCREASED" "10063263" 1 0.00% "5'NUCLEOTIDASE INCREASED" "10000028" 1 0.00% "ABASIA" "10049460" 1309 0.20% "ABDOMEN SCAN" "10061936" 10 0.00% "ABDOMEN SCAN NORMAL" "10061937" 13 0.00% "ABDOMINAL COMPARTMENT SYNDROME" "10058808" 2 0.00% "ABDOMINAL DISCOMFORT" "10000059" 1930 0.30% "ABDOMINAL DISTENSION" "10000060" 505 0.08% "ABDOMINAL EXPLORATION" "10053309" 1 0.00% "ABDOMINAL HERNIA" "10060954" 1 0.00% "ABDOMINAL HERNIA REPAIR" "10060802" 2 0.00% "ABDOMINAL INFECTION" "10056519" 3 0.00% "ABDOMINAL INJURY" "10060924" 3 0.00% "ABDOMINAL LYMPHADENOPATHY" "10073485" 3 0.00% "ABDOMINAL MASS" "10000077" 21 0.00% "ABDOMINAL OPERATION" "10061609" 6 0.00% "ABDOMINAL PAIN" "10000081" 5426 0.84% "ABDOMINAL PAIN LOWER" "10000084" 171 0.03% "ABDOMINAL PAIN UPPER" "10000087" 3699 0.57% "ABDOMINAL RIGIDITY" "10000090" 32 0.00% "ABDOMINAL SYMPTOM" "10060926" 3 0.00% "ABDOMINAL TENDERNESS" "10000097" 62 0.01% "ABDOMINAL WALL ABSCESS" "10000099" 1 0.00% "ABDOMINAL WALL DISORDER" "10059625" 1 0.00% "ABDOMINAL WALL NEOPLASM MALIGNANT" "10071023" 1 0.00% "ABDOMINAL X-RAY" "10061612" 279 0.04% "ABNORMAL BEHAVIOUR" "10061422" 1775 0.27% "ABNORMAL CLOTTING FACTOR" "10049862" 1 0.00% "ABNORMAL DREAMS" "10000125" 133 0.02% "ABNORMAL FAECES" "10000133" 247 0.04% "ABNORMAL LABOUR" "10000153" 37 0.01% "ABNORMAL LABOUR AFFECTING FOETUS" "10000154" 1 0.00% "ABNORMAL LOSS OF WEIGHT" "10000159" 23 0.00% "ABNORMAL PRODUCT OF CONCEPTION" "10060927" 2 0.00% "ABNORMAL SENSATION IN EYE" "10000173" -

ICD-9 Diagnosis Codes Effective 10/1/2011 (V29.0) Source: Centers for Medicare and Medicaid Services
ICD-9 Diagnosis Codes effective 10/1/2011 (v29.0) Source: Centers for Medicare and Medicaid Services 0010 Cholera d/t vib cholerae 00801 Int inf e coli entrpath 01086 Prim prg TB NEC-oth test 0011 Cholera d/t vib el tor 00802 Int inf e coli entrtoxgn 01090 Primary TB NOS-unspec 0019 Cholera NOS 00803 Int inf e coli entrnvsv 01091 Primary TB NOS-no exam 0020 Typhoid fever 00804 Int inf e coli entrhmrg 01092 Primary TB NOS-exam unkn 0021 Paratyphoid fever a 00809 Int inf e coli spcf NEC 01093 Primary TB NOS-micro dx 0022 Paratyphoid fever b 0081 Arizona enteritis 01094 Primary TB NOS-cult dx 0023 Paratyphoid fever c 0082 Aerobacter enteritis 01095 Primary TB NOS-histo dx 0029 Paratyphoid fever NOS 0083 Proteus enteritis 01096 Primary TB NOS-oth test 0030 Salmonella enteritis 00841 Staphylococc enteritis 01100 TB lung infiltr-unspec 0031 Salmonella septicemia 00842 Pseudomonas enteritis 01101 TB lung infiltr-no exam 00320 Local salmonella inf NOS 00843 Int infec campylobacter 01102 TB lung infiltr-exm unkn 00321 Salmonella meningitis 00844 Int inf yrsnia entrcltca 01103 TB lung infiltr-micro dx 00322 Salmonella pneumonia 00845 Int inf clstrdium dfcile 01104 TB lung infiltr-cult dx 00323 Salmonella arthritis 00846 Intes infec oth anerobes 01105 TB lung infiltr-histo dx 00324 Salmonella osteomyelitis 00847 Int inf oth grm neg bctr 01106 TB lung infiltr-oth test 00329 Local salmonella inf NEC 00849 Bacterial enteritis NEC 01110 TB lung nodular-unspec 0038 Salmonella infection NEC 0085 Bacterial enteritis NOS 01111 TB lung nodular-no exam 0039 -

Livedoid Vasculopathy Associated with Peripheral Neuropathy: a Report of Two Cases* Vasculopatia Livedoide Associada a Neuropatia Periférica: Relato De Dois Casos
CASE REPORT 227 s Livedoid vasculopathy associated with peripheral neuropathy: a report of two cases* Vasculopatia livedoide associada a neuropatia periférica: relato de dois casos Mariana Quirino Tubone1 Gabriela Fortes Escobar1 Juliano Peruzzo1 Pedro Schestatsky2 Gabriela Maldonado3 DOI: http://dx.doi.org/10.1590/abd1806-4841.20132363 Abstract: Livedoid vasculopathy (LV) is a chronic and recurrent disease consisting of livedo reticularis and sym- metric ulcerations, primarily located on the lower extremities, which heal slowly and leave an atrophic white scar ("atrophie blanche"). Neurological involvment is rare and presumed to be secondary to the ischemia from vascu- lar thrombosis of the vasa nervorum. Laboratory evaluation is needed to exclude secondary causes such as hyper- coagulable states, autoimmune disorders and neoplasms. We present two patients with a rare association of peripheral neuropathy and LV, thereby highlighting the importance of a multidisciplinary approach to reach the correct diagnosis. Keywords: Livedo reticularis; Mononeuropathies; Polyneuropathies; Skin diseases, vascular Resumo: Vasculopatia livedoide é uma doença crônica e recorrente caracterizada por livedo reticular e úlceras simétricas nos membros inferiores, que cicatrizam e deixam uma cicatriz branca atrófica ("atrophie blanche"). Envolvimento neurológico é raro e está provavelmente associado a isquemia pela trombose dos vasa nervorum. Avaliação laboratorial é indicada com o intuito de excluir causas secundárias como estados de hipercoagulabili- dade, doenças autoimunes e neoplasias. Apresentamos dois pacientes com uma rara associação de vasculopatia livedoide com neuropatia periférica, enfatizando a importância de uma abordagem multidisciplinar na busca do diagnóstico correto. Palavras-chave: Dermatopatias vasculares; Livedo reticular; Mononeuropatias; Polineuropatias INTRODUCTION Livedoid vasculopathy (LV) is a chronic and resentation of the dermo-hypodermic junction, was recurrent disease, usually restricted to the skin, and compatible with LV. -

Cerebral Venous Thrombosis and Livedo Reticularis in a Case with MTHFR 677TT Homozygote
Journal of Clinical Neurology / Volume 2 / June, 2006 Case Report Cerebral Venous Thrombosis and Livedo Reticularis in a Case with MTHFR 677TT Homozygote Jee-Young Lee, M.D., Manho Kim, M.D., Ph.D. Department of Neurology, College of Medicine, Seoul National University, Seoul, Korea Hyperhomocysteinemia associated with methylene terahydrofolate reductase (MTHFR) mutation can be a risk factor for idiopathic cerebral venous thrombosis. We describe the first case of MTHFR 677TT homozygote with cerebral venous thrombosis and livedo reticularis. A 45-year-old man presented with seizures and mottled-like skin lesions, that were aggravated by cold temperature. Hemorrhagic infarct in the right frontoparietal area with superior sagittal sinus thrombosis was observed. He had hyperhomocysteinemia, low plasma folate level, and MTHFR 677TT homozygote genotype, which might be associated with livedo reticularis and increase the risk for cerebral venous thrombosis. J Clin Neurol 2(2):137-140, 2006 Key Words : Livedo reticularis, Methylene tetrahydrofolate reductase, Cerebral venous thrombosis Hyperhomocysteinemia causes vascular endothelial venous infarct due to cerebral venous thrombosis. damage that result in atherosclerosis and ischemic strokes.1 It is also associated with prothrombotic state or venous thromboembolism2 including cerebral venous CASE REPORT thrombosis.3 Among the thrombophilic factors with hyperhomocysteinemia, methylene tetrahydrofolate reduc- A 45 year-old man was brought to the emergency tase (MTHFR) mutant (C677 → T, homozygote) with room with uncontrolled seizures. Two days ago, sudden low plasma folate concentration increases the risk for paresthesia in left arm developed, which progressed to cerebral venous thrombosis.4 MTHFR 677TT is thermo- tonic posturing and leftward head version, followed by labile and sensitive to temperature alteration.5 a generalized tonic clonic seizure. -

What Are Panic Attacks?
What are Panic Attacks? Understanding the body’s “Fight or Flight” response to a threat. We all have a built-in alarm system that turns on automatically to make sure we survive whatever danger triggers it. This alarm is a lot like a burglar alarm on a house; once it detects something that might be a threat, it automatically sets off several events. If someone were breaking into your house, you would want the alarm system to call the police immediately. You would also likely want to turn on lights and even sound an audible alarm to wake you and scare off the intruder. The brain’s alarm system sets off a series of events as well, commonly called the “fight or flight” response. The fight or flight response is meant to put us in a state of high alert so that we can fight off an enemy or flee to escape with our lives. This alarm makes us faster and stronger and more focused than we would normally be. Our ancestors may not have survived if the human body was not hardwired with the fight or flight response. The reaction is automatic. It helps us survive, and we do not have to think about it; it just happens. But because it is automatic, we do not get to choose which things will set it off. Sometimes, the fight or flight response can start firing if it thinks there is danger, even when there isn’t any real threat around. This is especially common in people who have been through a traumatic event. -

Livedoid Vasculopathy – Benefit of Intravenous Immunoglobulin in A
CASE REPORTS Ref: Ro J Rheumatol. 2021;30(1) DOI: 10.37897/RJR.2021.1.4 LIVEDOID VASCULOPATHY – BENEFIT OF INTRAVENOUS IMMUNOGLOBULIN IN A REFRACTORY CASE Stefan Cristian Dinescu1, Andreea Lili Barbulescu2, Paulina Lucia Ciurea1, Roxana Mihaela Dumitrascu3, Beatrice Andreea Chisalau3, Cristina Dorina Parvanescu3, Sineta Cristina Firulescu4, Florentin Ananu Vreju1 1 Department of Rheumatology, University of Medicine and Pharmacy, Craiova, Romania 2 Department of Pharmacology, University of Medicine and Pharmacy, Craiova, Romania 3Doctoral School, University of Medicine and Pharmacy, Craiova, Romania 4 Department of Rheumatology, Emergency County Hospital, Craiova, Romania Abstract Livedoid vasculopathy is a rare vascular disease which typically manifests as recurrent ulcerative lesions on the lower extremities. It is classified as a vasculopathy, not a true vasculitis, and defined as a vasooclusive syndrome, caused by non-inflammatory thrombosis of the upper and mid-dermal venulae. Main disorders associated with LV include thrombophilias, autoimmune diseases and neoplasia. A triad of clinical features is present in most patients and consist of livedo racemosa (less frequently livedo reticularis), ulcerations and atrophie blanche. Management generally relies on antiplatelet drugs, anticoagulants, vasodilators and fibrinolytic therapy. Some benefit has been observed with intravenous immunoglobulin, colchicine, hyperbaric oxygen, while glucocorticoids are efficient to a lesser extent. This case report highlights a refractory clinical form with no identifiable predisposing condition, which proved responsive only to intravenous immunoglobulin. Keywords: thrombosis, purpura, ulcer, intravenous immunoglobulins INTRODUCTION cal form with no identifiable predisposing condition, which proved responsive only to intravenous immu Livedoid vasculopathy (LV) is a rare vascular dis noglobulin. ease which typically manifests as recurrent ulcerative lesions on the lower extremities. -

Sneddon's Syndrome
DOI: 10.5272/jimab.14-1-2010.72 Journal of IMAB - Annual Proceeding (Scientific Papers) 2008, vol. 14, book 1 SNEDDON’S SYNDROME Valentin Valtchev1, Virginia Simeonova2 , Dimitar Gospodinov1, Ivelina Yordanova1, Valentina Dimitrova1, Verka Pavlova1, Emiliana Konova4, S. Popovska3 , Boyko Stamenov2 1Department of Dermatology and Venereology, 2Department of Neurology, 3Department of General and Clinical Pathology, 4Department of Immunology, Medical University – Pleven, Bulgaria ABSTRACT pressure and migraine for 10 years. She has been having Sneddon’s syndrome is usually characterized by the persistent cutaneous lesions on the upper and lower association of an ischemic cerebrovascular disease and a extremities and trunk for the last 20 years. widespread livedo reticularis. The incidence of Sneddon At physical examination, a slight elevation in syndrome is 4/1000 000. We present 42-year-old woman with pressure levels (150 x 80mm Hg), III degree obesity and livedo reticularis, recurrence ischaemic cerebrovascular slight edema of the lower limbs were found. The accidents, two repetitive miscarriages and positive anti-2GPi neurological examination revealed ataxic walk. Romberg antibodies. Skin biopsy specimens reveal inflammatory reflex was negative (-) and Babinski was positive (+) in changes of small- to medium-sized arteries and right. The ophthalmologic examination demonstrated an subendothelial proliferation and fibrosis. The diagnosis initial angiosclerosis. The dermatological examination Sneddon syndrome is confirmed by skin biopsy, and MR showed erythematous violaceous lesions with a reticular evidence. pattern, localized in the arms, trunk (Figure 1) thighs and We suggest that anti-2GPi antibodies may be knees (Figure 2, Figure 3). The following exams in the pathophysiologically related to the clinical manifestation laboratorial evaluation were normal or negative: blood count observed in some patients with Sneddon syndrome. -

Upper Limb Pain and Paresthesia in a Post-Stroke Patient Treated With
02 Brain Neurorehabil. 2018 Mar;11(1):e1 https://doi.org/10.12786/bn.2018.11.e1 pISSN 1976-8753·eISSN 2383-9910 Brain & NeuroRehabilitation Case Upper Limb Pain and Paresthesia in a Post-Stroke Patient Treated with Ultrasound-Guided Electrical Twitch-Obtaining Intramuscular Stimulation(ETOIMS) of Scalene Muscles Je Shik Nam, Yeo-Reum Choe, Seo Yeon Yoon, Tae Im Yi Received: Sep 1, 2017 Highlights Revised: Sep 29, 2017 Accepted: Oct 2, 2017 • Disputed thoracic outlet syndrome (TOS) can be one of the possible causes of post-stroke Correspondence to pain. Tae Im Yi • Ultrasound-guided electrical twitch-obtaining intramuscular stimulation can be used as a Departments of Rehabilitation Medicine, safe and minimally invasive technique for the treatment of the disputed TOS. Bundang Jesaeng General Hospital, • Large-scale randomized controlled studies are needed to confirm its therapeutic efficacy. 20 Seohyeon-ro 180 beon-gil, Bundang-gu, Seongnam 13590, Korea. E-mail: [email protected] Copyright © 2018. Korea Society for Neurorehabilitation i 02 Brain Neurorehabil. 2018 Mar;11(1):e1 https://doi.org/10.12786/bn.2018.11.e1 pISSN 1976-8753·eISSN 2383-9910 Brain & NeuroRehabilitation Case Upper Limb Pain and Paresthesia in a Post-Stroke Patient Treated with Ultrasound-Guided Electrical Twitch-Obtaining Intramuscular Stimulation(ETOIMS) of Scalene Muscles Je Shik Nam , Yeo-Reum Choe , Seo Yeon Yoon , Tae Im Yi Department of Rehabilitation Medicine, Bundang Jesaeng General Hospital, Seongnam, Korea Received: Sep 1, 2017 ABSTRACT Revised: Sep 29, 2017 Accepted: Oct 2, 2017 In post-stroke patients, the pain or paresthesia of the affected limb is common. -

Prognosis of a Case with Paresthesia Associated with Prolonged Touching of an Endodontic Paste to the Inferior Alveolar Nerve
J Clin Exp Dent. 2011;3(Suppl1):e377-81. Inferior alveolar nerve paresthesia. Journal section: Oral Surgery doi:10.4317/jced.3.e377 Publication Types: Case Report Prognosis of a case with paresthesia associated with prolonged touching of an endodontic paste to the inferior alveolar nerve M. Cemil Buyukkurt 1, Hakan Arslan 2, H. Sinan Topcuoglu 2, M. Melih Omezli 3 1 PhD, DDS. Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Sifa University, İzmir, Turkey 2 DDS. Department of Endodontic, Faculty of Dentistry, Ataturk University, Erzurum, Turkey 3 DDS. Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Ataturk University, Erzurum, Turkey Correspondence: Department of Endodontic, Faculty of Dentistry, Ataturk University, Erzurum, 25240, Turkey E-mail address: [email protected] Received: 10/02/2011 Accepted: 08/05/2011 Buyukkurt MC, Arslan H, Topcuoglu HS, Omezli MM. Prognosis of a case with paresthesia associated with prolonged touching of an endodontic paste to the inferior alveolar nerve. J Clin Exp Dent. 2011;3(Suppl1):e377- 81. http://www.medicinaoral.com/odo/volumenes/v3iSuppl1/jcedv3iSu- ppl1p377.pdf Article Number: 50506 http://www.medicinaoral.com/odo/indice.htm © Medicina Oral S. L. C.I.F. B 96689336 - eISSN: 1989-5488 eMail: [email protected] Abstract Paresthesia is described as an abnormal sensation, such as burning, pricking, tickling, tingling, formication or num- bness. Several conditions can cause paresthesia. This article presents a case of paresthesia caused by the extrusion of endodontic paste (Endomethasone®) into the mandibular canal. The clinical manifestations comprised the numb- ness on the right side of the mandible and right lower lip, appearing after endodontic treatment. -

Actiq (Oral Transmucosal Fentanyl)
Texas Prior Authorization Program Clinical Edit Criteria Drug/Drug Class Actiq (Oral Transmucosal Fentanyl) Clinical Edit Information Included in this Document Actiq 200mcg • Drugs requiring prior authorization: the list of drugs requiring prior authorization for this clinical edit • Prior authorization criteria logic: a description of how the prior authorization request will be evaluated against the clinical edit criteria rules • Logic diagram: a visual depiction of the clinical edit criteria logic • Supporting tables: a collection of information associated with the steps within the criteria (diagnosis codes, procedure codes, and therapy codes); provided when applicable • References: clinical publications and sources relevant to this clinical edit Actiq Greater Than or Equal To (≥) 400mcg • Drugs requiring prior authorization: the list of drugs requiring prior authorization for this clinical edit • Prior authorization criteria logic: a description of how the prior authorization request will be evaluated against the clinical edit criteria rules • Logic diagram: a visual depiction of the clinical edit criteria logic • Supporting tables: a collection of information associated with the steps within the criteria (diagnosis codes, procedure codes, and therapy codes); provided when applicable • References: clinical publications and sources relevant to this clinical edit Note: Click the hyperlink to navigate directly to that section. February 7, 2012 Copyright © 2011-2012 Health Information Designs, LLC 1 Texas Prior Authorization Program Clinical -

Small Animal
Small Animal Sampler Separation Distress Syndrome From Blackwell’s Five-Minute Veterinary Consult – Canine and Feline, Sixth Edition. by Deborah F. Horwitz Chapter 236: Vomiting From The Feline Patient, Fifth Edition. Edited by Gary D. Norsworthy. Chapter 12: Pharmacologic and Clinical Principles of Adjunct Analgesia From Analgesia and Anesthesia for the Ill or Injured Dog and Cat, First Edition. by Karol A. Mathews, Melissa Sinclair, Andrea M. Steele, and Tamara Grubb. 1208 Blackwell’s Five-Minute Veterinary Consult Separation Distress Syndrome commonly reported. Destruction targets windows and doors and/or owner possessions. Other signs include behavioral depression, BASICS anorexia,r drooling, hiding, shaking, panting, DIAGNOSIS DEFINITION pacing, attempts to prevent owner departure, DIFFERENTIAL DIAGNOSIS A distress response of dogs (occasionally cats) and self-trauma from lick lesions. Diarrhea Vocalization: response to outdoor separated from the person or persons to and vomiting are occasionally noted. Signs influences,r territorial displays, play with other whom they are most attached, usually their of strong pet-owner attachment may ber pets in the home or fears. Destructive owner(s). The separation may be real (the present: excessive attention-seeking behaviors behaviors: occur both whenr the owner is owner is gone) or perceived (the pet is just and following behaviors but not necessary for present and absent (e.g., territorial destructive separated from the owner). In other cases the diagnosis. Frequently owners report displays at windows and doors; destruction pet may be distressed because some excessive, excited,r and prolonged greeting due to fear-producing stimuli such as noises fear-inducing event has occurred while home behavior upon return. -

The 12 Cranial Nerves
The 12 Cranial Nerves Edited by Sterling Precision Nelson Cranial Nerve I: Olfactory Nerve Type of Nerve: Sensory Function of Nerve: Sense of Smell Brief description: The Olfactory Nerve is the first of the 12 pairs of cranial nerves in the brain. It’s a sensory nerve, in charge of transmitting olfactory stimuli from the nose to the brain, Its actual origin is given by the cells of the olfactory bulb and is the shortest cranial pair of all of the pairs in the brain. Important side note: Damaged olfactory nerve cells can regenerate, but don’t always reconnect properly in the brain. Name Nerve Disorder Treatment Dysnomia - Parosmia Distortion of smelling that No specific cure refers to the perception of available, but symptoms the smell. lessen over time, in some patients it may take years. Dysnomia - Phantosmia Distortion of smelling that Can recover easily if it refers to a smell not from sickness however present. rinsing out the sinus with saline solution will help treat the problem. Hyposmia A decreased ability to there's no known cure or smell. treatment for congenital anosmia. Anosmia A total inability to smell. there's no known cure or treatment for congenital anosmia. Cranial Nerve II: Optical Type of Nerve: Sensory Function of Nerve: Vision Brief description: The Optical cranial pair is the second of the 12 pairs of cranial nerves and it is responsible for conducting visual stimuli from the eye to the brain. It is made of axons from the ganglion cells of the retina, that take the information of the photoreceptors to the brain, where later it will be integrated and interpreted and It emerges in the diencephalon.