Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0 Published: November 27, 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abscess Prevention
ABSCESS PREVENTION ▪ Chest pains may occur if infection How do you soak/use Avoiding abscesses goes to heart or lungs compresses? • Wash your hands and the injection site. What should I do if I get ▪ Use warm/hot water (that doesn’t burn your skin) • Use alcohol pads and wipe an abscess? ▪ Soak in tub of plain hot water or hot back & forth (rub hard) over ▪ Treat at home with warm soaks water with Epsom salts injection site to remove dirt. only if: ▪ Use hot, wet, clean washcloth and - No red streaks hold on abscess, if abscess cannot • Then use another new alcohol - Skin not hot and puffy be soaked in tub pad for the final cleaning. ▪ Soak abscess 3 to 4 times a day for ▪ Go to a clinic if abscess: 10-15 minutes each time, if possible What is a skin abscess? - Not improving, especially ▪ Cover with a clean dry bandage after after 5-7 days soaking ▪ Pocket of pus - Gets bigger and/or very ▪ soaking/using compresses ▪ Often found at injection sites, but STOP painful when abscess starts draining can be found elsewhere - Is hot and puffy ▪ More likely with Red streaks start spreading skin-popping from the abscess-go ASAP! muscling What about missing a vein ▪ Go to emergency room if: ▪ May occur even after you stop Chest pain antibiotics? injecting High fever, chills ▪ Take all antibiotics, if Infection looks like it is How do you know it’s an spreading fast prescribed, even if you feel better abscess? ▪ Take antibiotics after you fix (if ▪ using heroin) ▪ Pink or reddish lump on skin ▪ Do not take antibiotics with ▪ Tender or painful Warning -

Recognizing When a Child's Injury Or Illness Is Caused by Abuse
U.S. Department of Justice Office of Justice Programs Office of Juvenile Justice and Delinquency Prevention Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE U.S. Department of Justice Office of Justice Programs 810 Seventh Street NW. Washington, DC 20531 Eric H. Holder, Jr. Attorney General Karol V. Mason Assistant Attorney General Robert L. Listenbee Administrator Office of Juvenile Justice and Delinquency Prevention Office of Justice Programs Innovation • Partnerships • Safer Neighborhoods www.ojp.usdoj.gov Office of Juvenile Justice and Delinquency Prevention www.ojjdp.gov The Office of Juvenile Justice and Delinquency Prevention is a component of the Office of Justice Programs, which also includes the Bureau of Justice Assistance; the Bureau of Justice Statistics; the National Institute of Justice; the Office for Victims of Crime; and the Office of Sex Offender Sentencing, Monitoring, Apprehending, Registering, and Tracking. Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE NCJ 243908 JULY 2014 Contents Could This Be Child Abuse? ..............................................................................................1 Caretaker Assessment ......................................................................................................2 Injury Assessment ............................................................................................................4 Ruling Out a Natural Phenomenon or Medical Conditions -

Familial Hyperinsulinism Due to HNF4A Deficiency and Benign Premature Adrenarche: a Case Report
Case Report Familial Hyperinsulinism due to HNF4A Deficiency and Benign Premature Adrenarche: A Case Report Edward Compton,1 David H. Geller,2 Alaina P. Vidmar MD.3 Abstract Background: Familial Hyperinsulinism due to HNF4A deficiency (FHI-HNF4A) is a form of diazoxide-sensitive, diffuse hyperinsulinism, characterized by transient or persistent hyperinsulinemic hypoglycemia, and a propensity to develop Maturity-Onset Diabetes of the Young type 1 (MODY1). The association between FHI-HNF4A deficiency and benign premature adrenarche (BPA) is unknown. The Case: We report the case of a 5-year-old girl with FHI-HNF4A, controlled on diazoxide, who presented with BPA and Tanner stage 3 pubic hair associated with body odor and acne. Work-up revealed elevated dehydroepiandrosterone sulfate (DHEAS), elevated free testosterone, and advanced bone age. Insulin levels were elevated in the setting of normal fasting blood glucose. We discuss the possible hormonal underpinnings of hyperandrogenism. Conclusion: Though the underlying pathophysiology of this phenotype is unclear, a possible synergistic mechanism exists between insulin-induced hyperandrogenism and HNF4A deficiency leading to a transient decrease of SHBG and thus increased free testosterone levels. Further investigation is required to determine the association between HNF4A dysfunction and BPA. Key Words: Hyperinsulinism; Congenital Hyperinsulinism; Adrenarche; HNF4A; Hyperandrogenism (Source: MeSH-NLM). Introduction Congenital hyperinsulinism (CHI) is due to a variety of etiologies that Highlights: result in dysregulated insulin release from pancreatic β-cells. There are Familial Hyperinsulinism due to HNF4A deficiency (FHI-HNF4A) is a two histological variants of CHI, focal and diffuse, which differ in the form of diazoxide-sensitive; diffuse hyperinsulinism, characterized by extent of pancreatic involvement. -

A Misunderstood Teenager with Paediatric Inflammatory Multisystem Syndrome – Temporarily Associated with SARS-Cov-2 Admitted Under Adult Medicine
LESSONS OF THE MONTH Clinical Medicine 2021 Vol 21, No 1: e96–9 Lessons of the month: A misunderstood teenager with paediatric inflammatory multisystem syndrome – temporarily associated with SARS-CoV-2 admitted under adult medicine Authors: Sachin T PatelA and Harry WrightB The emergence of SARS-CoV-2 has proven to be a challenge low total protein (52 g/L), albumin (28 g/L), globulin (23 g/L) and to healthcare bodies globally. The virus has been associated alkaline phosphatase (49 U/L). A surgical review was sought, and with a spectrum of clinical features, from anosmia to they recommended radiological imaging. Contrast computed gastrointestinal upset to multiorgan dysfunction in the tomography (CT) of the chest, abdomen and pelvis showed most severe cases. Given the range of features observed, it is multiple enlarged mesenteric nodes, especially in the RIF, possibly ABSTRACT important to be aware that infectious diseases can present in keeping with mesenteric adenitis (Fig 1). The visualised appendix atypically. Furthermore, in many hospitals, including our own, was unremarkable and both lung fields were clear. All other teenagers aged 16 to 18 years old are admitted under the abdominal and pelvic viscera were unremarkable. care of adult medical services. Clinicians should be aware of As appendicitis was ruled out by the surgical team, he was patients presenting with the novel condition of paediatric started on intravenous (IV) aciclovir 600 mg, 3 times a day, and IV inflammatory multisystem disorder – temporarily associated ceftriaxone 2 g, 12 hourly, to cover for meningitis. He also received with SARS-CoV-2 (PIMS-TS). -

ANXIETY DISORDERS Date of Publication: Jan
Disease/Medical Condition ANXIETY AND ANXIETY DISORDERS Date of Publication: Jan. 31, 2019 (Anxiety disorders include “generalized anxiety disorder”; “social anxiety disorder” [formerly known as “social phobia”]; “separation anxiety disorder”; “selective mutism”; “agoraphobia”; “substance abuse/medication-induced anxiety disorder”; “specific phobias” [also known as “simple phobias”, which include claustrophobia, blood phobia, needle phobia, and dental phobia1]; and “panic disorder”.) Is the initiation of non-invasive dental hygiene procedures* contra-indicated? No, unless the patient/ client displays signs/symptoms of anxiety or an anxiety disorder that pose a risk to himself/herself or the dental hygienist during procedures (e.g., markedly elevated heartrate with comorbid heart disease, inability to sit still, etc.). Is medical consult advised? — No, if anxiety disorder has been previously diagnosed and is well controlled. — Yes, if anxiety disorder is newly suspected or poor control of previously diagnosed anxiety disorder is suspected. — Yes, if severe xerostomia is suspected to be related to antidepressant or benzodiazepine use (which may improve if an alternative medication is a consideration). Is the initiation of invasive dental hygiene procedures contra-indicated?** No, unless the patient/ client displays signs/symptoms of anxiety or an anxiety disorder that pose a risk to himself/herself or the dental hygienist during procedures (e.g., markedly elevated heartrate with comorbid heart disease, inability to sit still, etc.). Is medical consult advised? ....................................... See above. Is medical clearance required? .................................. No, unless: — a panic attack has previously occurred in the dental/dental hygiene setting; or — severe leukopenia (i.e., reduced white blood cell count, and hence immunosuppression) is suspected with tricyclic antidepressant (TCA) or monoamine oxidase inhibitor2 (MAOI) medication use. -

Protocols for Injuries to the Eye Corneal Abrasion I
PROTOCOLS FOR INJURIES TO THE EYE CORNEAL ABRASION I. BACKGROUND A corneal abrasion is usually caused by a foreign body or other object striking the eye. This results in a disruption of the corneal epithelium. II. DIAGNOSTIC CRITERIA A. Pertinent History and Physical Findings Patients complain of pain and blurred vision. Photophobia may also be present. Symptoms may not occur for several hours following an injury. B. Appropriate Diagnostic Tests and Examinations Comprehensive examination by an ophthalmologist to rule out a foreign body under the lids, embedded in the cornea or sclera, or penetrating into the eye. The comprehensive examination should include a determination of visual acuity, a slit lamp examination and a dilated fundus examination when indicated. III. TREATMENT A. Outpatient Treatment Topical antibiotics, cycloplegics, and pressure patch at the discretion of the physician. Analgesics may be indicated for severe pain. B. Duration of Treatment May require daily visits until cornea sufficiently healed, usually within twenty-four to seventy-two hours but may be longer with more extensive injuries. In uncomplicated cases, return to work anticipated within one to two days. The duration of disability may be longer if significant iritis is present. IV. ANTICIPATED OUTCOME Full recovery. CORNEAL FOREIGN BODY I. BACKGROUND A corneal foreign body most often occurs when striking metal on metal or striking stone. Auto body workers and machinists are the greatest risk for a corneal foreign body. Hot metal may perforate the cornea and enter the eye. Foreign bodies may be contaminated and pose a risk for corneal ulcers. II. DIAGNOSTIC CRITERIA A. Pertinent History and Physical Findings The onset of pain occurs either immediately after the injury or within the first twenty-four hours. -

Skin Injuries – Can We Determine Timing and Mechanism?
Skin injuries – can we determine timing and mechanism? Jo Tully VFPMS Seminar 2016 What skin injuries do we need to consider? • Bruising • Commonest accidental and inflicted skin injury • Basic principles that can be applied when formulating opinion • Abrasions • Lacerations }we need to be able to tell the difference • Incisions • Stabs/chops • Bite marks – animal v human / inflicted v ‘accidental’ v self-inflicted Our role…. We are often/usually/always asked…………….. • “What type of injury is it?” • “When did this injury occur?” • “How did this injury occur?” • “Was this injury inflicted or accidental?” • IS THIS CHILD ABUSE? • To be able to answer these questions (if we can) we need knowledge of • Anatomy/physiology/healing - injury interpretation • Forces • Mechanisms in relation to development, plausibility • Current evidence Bruising – can we really tell which bruises are caused by abuse? Definitions – bruising • BLUNT FORCE TRAUMA • Bruise =bleeding beneath intact skin due to BFT • Contusion = bruise in deeper tissues • Haematoma - extravasated blood filling a cavity (or potential space). Usually associated with swelling • Petechiae =Pinpoint sized (0.1-2mm) hemorrhages into the skin due to acute rise in venous pressure • medical causes • direct forces • indirect forces Medical Direct Indirect causes mechanical mechanical forces forces Factors affecting development and appearance of a bruise • Properties of impacting object or surface • Force of impact • Duration of impact • Site - properties of body region impacted (blood supply, -

Synovial Fluidfluid 11
LWBK461-c11_p253-262.qxd 11/18/09 6:04 PM Page 253 Aptara Inc CHAPTER SynovialSynovial FluidFluid 11 Key Terms ANTINUCLEAR ANTIBODY ARTHROCENTESIS BULGE TEST CRYSTAL-INDUCED ARTHRITIS GROUND PEPPER HYALURONATE MUCIN OCHRONOTIC SHARDS RHEUMATOID ARTHRITIS (RA) RHEUMATOID FACTOR (RF) RICE BODIES ROPE’S TEST SEPTIC ARTHRITIS Learning Objectives SYNOVIAL SYSTEMIC LUPUS ERYTHEMATOSUS 1. Define synovial. VISCOSITY 2. Describe the formation and function of synovial fluid. 3. Explain the collection and handling of synovial fluid. 4. Describe the appearance of normal and abnormal synovial fluids. 5. Correlate the appearance of synovial fluid with possible cause. 6. Interpret laboratory tests on synovial fluid. 7. Suggest further testing for synovial fluid, based on preliminary results. 8. List the four classes or categories of joint disease. 9. Correlate synovial fluid analyses with their representative disease classification. 253 LWBK461-c11_p253-262.qxd 11/18/09 6:04 PM Page 254 Aptara Inc 254 Graff’s Textbook of Routine Urinalysis and Body Fluids oint fluid is called synovial fluid because of its resem- blance to egg white. It is a viscous, mucinous substance Jthat lubricates most joints. Analysis of synovial fluid is important in the diagnosis of joint disease. Aspiration of joint fluid is indicated for any patient with a joint effusion or inflamed joints. Aspiration of asymptomatic joints is beneficial for patients with gout and pseudogout as these fluids may still contain crystals.1 Evaluation of physical, chemical, and microscopic characteristics of synovial fluid comprise routine analysis. This chapter includes an overview of the composition and function of synovial fluid, and laboratory procedures and their interpretations. -

Familial Mediterranean Fever and Periodic Fever, Aphthous Stomatitis, Pharyngitis, and Adenitis (PFAPA) Syndrome: Shared Features and Main Differences
Rheumatology International (2019) 39:29–36 Rheumatology https://doi.org/10.1007/s00296-018-4105-2 INTERNATIONAL REVIEW Familial Mediterranean fever and periodic fever, aphthous stomatitis, pharyngitis, and adenitis (PFAPA) syndrome: shared features and main differences Amra Adrovic1 · Sezgin Sahin1 · Kenan Barut1 · Ozgur Kasapcopur1 Received: 10 June 2018 / Accepted: 13 July 2018 / Published online: 17 July 2018 © Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract Autoinflammatory diseases are characterized by fever attacks of varying durations, associated with variety of symptoms including abdominal pain, lymphadenopathy, polyserositis, arthritis, etc. Despite the diversity of the clinical presentation, there are some common features that make the differential diagnosis of the autoinflammatory diseases challenging. Familial Mediterranean fever (FMF) is the most commonly seen autoinflammatory conditions, followed by syndrome associated with periodic fever, aphthous stomatitis, pharyngitis, and adenitis (PFAPA). In this review, we aim to evaluate disease charac- teristics that make a diagnosis of FMF and PFAPA challenging, especially in a regions endemic for FMF. The ethnicity of patient, the regularity of the disease attacks, and the involvement of the upper respiratory systems and symphonies could be helpful in differential diagnosis. Current data from the literature suggest the use of biological agents as an alternative for patients with FMF and PFAPA who are non-responder classic treatment options. More controlled studies -
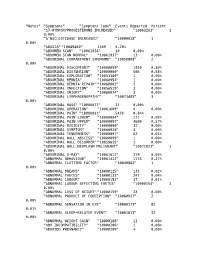
The Vaccine Adverse Event Reporting System (VAERS)
"Notes" "Symptoms" "Symptoms Code" Events Reported Percent "17-HYDROXYPROGESTERONE INCREASED" "10063263" 1 0.00% "5'NUCLEOTIDASE INCREASED" "10000028" 1 0.00% "ABASIA" "10049460" 1309 0.20% "ABDOMEN SCAN" "10061936" 10 0.00% "ABDOMEN SCAN NORMAL" "10061937" 13 0.00% "ABDOMINAL COMPARTMENT SYNDROME" "10058808" 2 0.00% "ABDOMINAL DISCOMFORT" "10000059" 1930 0.30% "ABDOMINAL DISTENSION" "10000060" 505 0.08% "ABDOMINAL EXPLORATION" "10053309" 1 0.00% "ABDOMINAL HERNIA" "10060954" 1 0.00% "ABDOMINAL HERNIA REPAIR" "10060802" 2 0.00% "ABDOMINAL INFECTION" "10056519" 3 0.00% "ABDOMINAL INJURY" "10060924" 3 0.00% "ABDOMINAL LYMPHADENOPATHY" "10073485" 3 0.00% "ABDOMINAL MASS" "10000077" 21 0.00% "ABDOMINAL OPERATION" "10061609" 6 0.00% "ABDOMINAL PAIN" "10000081" 5426 0.84% "ABDOMINAL PAIN LOWER" "10000084" 171 0.03% "ABDOMINAL PAIN UPPER" "10000087" 3699 0.57% "ABDOMINAL RIGIDITY" "10000090" 32 0.00% "ABDOMINAL SYMPTOM" "10060926" 3 0.00% "ABDOMINAL TENDERNESS" "10000097" 62 0.01% "ABDOMINAL WALL ABSCESS" "10000099" 1 0.00% "ABDOMINAL WALL DISORDER" "10059625" 1 0.00% "ABDOMINAL WALL NEOPLASM MALIGNANT" "10071023" 1 0.00% "ABDOMINAL X-RAY" "10061612" 279 0.04% "ABNORMAL BEHAVIOUR" "10061422" 1775 0.27% "ABNORMAL CLOTTING FACTOR" "10049862" 1 0.00% "ABNORMAL DREAMS" "10000125" 133 0.02% "ABNORMAL FAECES" "10000133" 247 0.04% "ABNORMAL LABOUR" "10000153" 37 0.01% "ABNORMAL LABOUR AFFECTING FOETUS" "10000154" 1 0.00% "ABNORMAL LOSS OF WEIGHT" "10000159" 23 0.00% "ABNORMAL PRODUCT OF CONCEPTION" "10060927" 2 0.00% "ABNORMAL SENSATION IN EYE" "10000173" -

ICD-9 Diagnosis Codes Effective 10/1/2011 (V29.0) Source: Centers for Medicare and Medicaid Services
ICD-9 Diagnosis Codes effective 10/1/2011 (v29.0) Source: Centers for Medicare and Medicaid Services 0010 Cholera d/t vib cholerae 00801 Int inf e coli entrpath 01086 Prim prg TB NEC-oth test 0011 Cholera d/t vib el tor 00802 Int inf e coli entrtoxgn 01090 Primary TB NOS-unspec 0019 Cholera NOS 00803 Int inf e coli entrnvsv 01091 Primary TB NOS-no exam 0020 Typhoid fever 00804 Int inf e coli entrhmrg 01092 Primary TB NOS-exam unkn 0021 Paratyphoid fever a 00809 Int inf e coli spcf NEC 01093 Primary TB NOS-micro dx 0022 Paratyphoid fever b 0081 Arizona enteritis 01094 Primary TB NOS-cult dx 0023 Paratyphoid fever c 0082 Aerobacter enteritis 01095 Primary TB NOS-histo dx 0029 Paratyphoid fever NOS 0083 Proteus enteritis 01096 Primary TB NOS-oth test 0030 Salmonella enteritis 00841 Staphylococc enteritis 01100 TB lung infiltr-unspec 0031 Salmonella septicemia 00842 Pseudomonas enteritis 01101 TB lung infiltr-no exam 00320 Local salmonella inf NOS 00843 Int infec campylobacter 01102 TB lung infiltr-exm unkn 00321 Salmonella meningitis 00844 Int inf yrsnia entrcltca 01103 TB lung infiltr-micro dx 00322 Salmonella pneumonia 00845 Int inf clstrdium dfcile 01104 TB lung infiltr-cult dx 00323 Salmonella arthritis 00846 Intes infec oth anerobes 01105 TB lung infiltr-histo dx 00324 Salmonella osteomyelitis 00847 Int inf oth grm neg bctr 01106 TB lung infiltr-oth test 00329 Local salmonella inf NEC 00849 Bacterial enteritis NEC 01110 TB lung nodular-unspec 0038 Salmonella infection NEC 0085 Bacterial enteritis NOS 01111 TB lung nodular-no exam 0039 -

Taste and Smell Disorders in Clinical Neurology
TASTE AND SMELL DISORDERS IN CLINICAL NEUROLOGY OUTLINE A. Anatomy and Physiology of the Taste and Smell System B. Quantifying Chemosensory Disturbances C. Common Neurological and Medical Disorders causing Primary Smell Impairment with Secondary Loss of Food Flavors a. Post Traumatic Anosmia b. Medications (prescribed & over the counter) c. Alcohol Abuse d. Neurodegenerative Disorders e. Multiple Sclerosis f. Migraine g. Chronic Medical Disorders (liver and kidney disease, thyroid deficiency, Diabetes). D. Common Neurological and Medical Disorders Causing a Primary Taste disorder with usually Normal Olfactory Function. a. Medications (prescribed and over the counter), b. Toxins (smoking and Radiation Treatments) c. Chronic medical Disorders ( Liver and Kidney Disease, Hypothyroidism, GERD, Diabetes,) d. Neurological Disorders( Bell’s Palsy, Stroke, MS,) e. Intubation during an emergency or for general anesthesia. E. Abnormal Smells and Tastes (Dysosmia and Dysgeusia): Diagnosis and Treatment F. Morbidity of Smell and Taste Impairment. G. Treatment of Smell and Taste Impairment (Education, Counseling ,Changes in Food Preparation) H. Role of Smell Testing in the Diagnosis of Neurodegenerative Disorders 1 BACKGROUND Disorders of taste and smell play a very important role in many neurological conditions such as; head trauma, facial and trigeminal nerve impairment, and many neurodegenerative disorders such as Alzheimer’s, Parkinson Disorders, Lewy Body Disease and Frontal Temporal Dementia. Impaired smell and taste impairs quality of life such as loss of food enjoyment, weight loss or weight gain, decreased appetite and safety concerns such as inability to smell smoke, gas, spoiled food and one’s body odor. Dysosmia and Dysgeusia are very unpleasant disorders that often accompany smell and taste impairments.