Subject Index
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lower Gastrointestinal Bleeding
Journal of Experimental and Clinical Medicine https://dergipark.org.tr/omuJecm Re view Article J Exp Clin Med 2021; 38(S1): 23-32 doi: 10.52142/omujecm.38.si.gastro.3 Lower gastrointestinal bleeding Serkan ÖCAL1,* , Mehmet Mutlu ÇATLI2 1 Department of Gastroenterology, University of Health Sciences Antalya Training and Research Hospital, Antalya, Turkey 2Departmant of Internal Medicine, Antalya Training and Research Hospital, Antalya, Turkey Received: 13.12.2020 • Accepted/Published Online: 09.01.2021 • Final Version: 18.03.2021 Abstract Bleeding from the lower part of the digestive system that appears as hematocheZia (fresh blood, clot or cherry-colored stool) or melena (dark- colored tarry stool) is called lower gastrointestinal tract bleeding (lower GI bleeding) (or colonic bleeding). In the traditional definition, lower GI bleeding was generally classified as bleeding distal to the TreitZ ligament (duodenojejunal junction) as the border. In the last decade, GI bleeding has adopted three categories in some recent publications: Upper, middle, and lower. According to this category, bleeding from a source between the TreitZ ligament and the ileocecal valve is classified as middle GI bleeding, bleeding from the distal of the ileocecal valve is classified lower GI bleeding. Lower GI bleeding and hospitalization rates increase with aging. Currently, physicians managing lower GI bleeding have many different diagnostic and therapeutic options ranging from colonoscopy and flexible sigmoidoscopy to radiographic interventions such as scintigraphy or angiography. Lower GI bleeding often stops spontaneously and less common than upper GI bleeding. Even though no modality has emerged as the gold standard in the treatment of lower GI bleeding, colonoscopy has several advantages and is generally considered as the preferred initial test in most of the cases. -

High B1a0d Pressure and Its Treatment in General
HIGH B1A0D PRESSURE AND ITS TREATMENT IN GENERAL PRACTICE WITH PARTICULAR REFERENCE TO A SERIES OF 100 CASES TREATED BY THE AUTHOR By HAROLD WILSON B01YBR IB.ffh.B. ProQuest Number: 13849841 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 13849841 Published by ProQuest LLC(2019). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 -CONTENTS SECTION 1. Introduction. SECTION 2. General Remarks. Definitions of General Interest. Present Views on Etiology. Pathology and Morbid Anatomy. Brief Historical Survey. SECTION 3. The Present Position. Prevalence. Clinical Manifestations. Prognosis. SECTION 4. Prevalence in Bolton. Summary of Cases. Symptomatology and Case Histories Prognosis. Treatment. SECTION 5. Conclusions. Bibliography. SECTION 1. INTRODUCTION. I think it can truthfully be said that the most interest ing problems in Medioine are those that are most baffling. Some years ago Ralph M a j o r ^ wrote these words, ”If our knowledge of the etiology of arterial hypertension is shrouded in a oertain haze, our knowledge of an effective therapy in this disease is enveloped in a dense fog.n A study of some of the vast literature on this subject does not greatly clarify the obscurity. -

Developmental Venous Anomaly: MR and Angiographic Features
JBR–BTR, 2014, 97: 17-20. DEVELOPMENTAL VENOUS ANOMALY: MR AND ANGIOGRAPHIC FEATURES M. Faure1, M. Voormolen1, T. Van der Zijden1, P.M. Parizel1 Developmental venous anomaly (DVA) is probably the most common anomaly of the intracranial vasculature. DVAs consist of multiple, radially oriented dilated medullary veins that converge into a transcerebral vein. We describe the imaging findings of this vascular anomaly in different patients and the role of different imaging modalities. Key-words: Cerebral blood vessels, abnormalities – Cerebral blood vessels, MR – Cerebral angiography. Developmental venous anomaly (DVA) was first considered a rare vascular malformation (1, 2). Nowa- days, with the advent of Computed Tomography (CT) and especially Magnetic Resonance Imaging (MRI), DVAs are seen every week to month by radiologists (3, 4). Most DVAs are solitary, asymptomatic lesions and are discovered incidentally. They have a relatively benign nature with a low incidence of hemorrhage. When they do bleed, this is thought to be due to associated vascular mal- formations, like cavernous angiomas. The typical angiographic appearance of a DVA is a caput medusae appear- ance in the venous phase. MRI com- bined with MR angiography (MRA) replaces angiography in most un- A B complicated cases as a non-invasive alternative (3, 5). Case reports Case 1 A 32-year-old woman presented with headache, with no particular location and no neurological deficit. MRI of the brain was made in another hospital that showed a flow void running transcerebral, suggestive for a vascular malformation (Fig. 1A,B). Initially, there was no gadolinium contrast given and an arterial feeder could thus not be excluded with MRI. -

Outpatient Services
Outpatient Services Coverage of Certain Services in the OUTPATIENT setting only* EFFECTIVE MARCH 9, 2015 bmchp.org | 888-566-0008 TO FIND A CODE OR WORD - While holding down the CTRL key, press the F key, type in Code, then press ENTER key Procedure Code Description 0213T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, cervical or thoracic; single level 0214T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, cervical or thoracic; second level (List separately in addition to code for primary procedure) 0215T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, cervical or thoracic; third and any additional level(s) (List separately in addition to code for primary procedure) 0216T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, lumbar or sacral; single level 0217T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, lumbar or sacral; second level (List separately in addition to code for primary procedure) 0218T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound -

DISEASES of ARTERIES ARTERIOSCLEROSIS (“Hardening of the Arteries”): General Term Reflecting Arterial Wall Thickening and Loss of Elasticity
DISEASES OF ARTERIES ARTERIOSCLEROSIS (“hardening of the arteries”): general term reflecting arterial wall thickening and loss of elasticity 3 patterns •Atherosclerosis: involves the the aorta and the large arteries •Mönckeberg sclerosis: calcific deposits in the media of middle-sized arteries in persons >age 50 •Arteriolosclerosis: involves the small arteries and arterioles in association with hypertension or diabetes ATHEROSCLEROSIS Multifactorial, slowly progressive chronic degenerative-inflammatory disease of the aorta and the large arteries, such as • coronary arteries • circle of Willis • popliteal and tibial arteries Significance: > 50% of all death is attributed to atherosclerosis in well-developed countries Morphology Gross • Atheromatous plaque (pathognomic) - raised white-yellow lesion in the intima, protruding into the lumen • Large plaques in the aorta (> 2 cm) contain a yellow, grumous debris (”atheroma” - Greek word for gruel) Atheromatous plaque in the middle cerebral artery: raised white-yellow lesion in the intima, protruding into the lumen (formol-fixed brain) Aorta: the plaques contain a yellow, grumous debris (arrow) Structure of atheroma on LM • Intimal lesion • Central lipid core • Fibrous ”cap” subendothelially Central lipid core composed of lipids, cholesterol clefts, necrotic debris + calcium-salts, surrounded by foamy macrophages, T-lymphocytes, fibroblasts, small capillaries, and collagens and proteoglycans Types of plaques • Vulnerable plaques have large atheromatous cores, increased inflammatory cell content and thin fibrous caps high risk of rupture thrombosis • Stable plaques have minimal atheromatous cores and inflammation and thick fibrous caps 70% stenosis (critical stenosis) chronic ischemia distally Vulnerable plaque in the coronary artery Inflammatory infiltrates and capillaries around the lipid core. Lumen Intima Media Pathogenesis Response to chronic endocardial injury hypothesis • Cholesterol can’t dissolve in the blood. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -
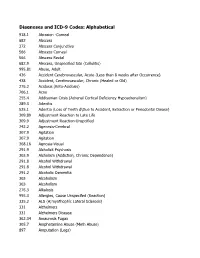
DSM III and ICD 9 Codes 11-2004
Diagnoses and ICD-9 Codes: Alphabetical 918.1 Abrasion -Corneal 682 Abscess 372 Abscess Conjunctiva 566 Abscess Corneal 566 Abscess Rectal 682.9 Abscess, Unspecified Site (Cellulitis) 995.81 Abuse, Adult 436 Accident Cerebrovascular, Acute (Less than 8 weeks after Occurrence) 438 Accident, Cerebrovascular, Chronic (Healed or Old) 276.2 Acidosis (Keto-Acidosis) 706.1 Acne 255.4 Addisonian Crisis (Adrenal Cortical Deficiency Hypoadrenalism) 289.3 Adenitis 525.1 Adentia (Loss of Teeth d\Due to Accident, Extraction or Periodontal Diease) 309.89 Adjustment Reaction to Late Life 309.9 Adjustment Reaction-Unspcified 742.2 Agenesis-Cerebral 307.9 Agitation 307.9 Agitation 368.16 Agnosia-Visual 291.9 Alcholick Psychosis 303.9 Alcholism (Addiction, Chronic Dependence) 291.8 Alcohol Withdrawal 291.8 Alcohol Withdrawal 291.2 Alcoholic Dementia 303 Alcoholism 303 Alcoholism 276.3 Alkalosis 995.3 Allergies, Cause Unspecifed (Reaction) 335.2 ALS (A;myothophic Lateral Sclerosis) 331 Alzheimers 331 Alzheimers Disease 362.34 Amaurosis Fugax 305.7 Amphetamine Abuse (Meth Abuse) 897 Amputation (Legs) 736.89 Amputation, Leg, Status Post (Above Knee, Below Knee) 736.9 Amputee, Site Unspecified (Acquired Deformity) 285.9 Anemia 284.9 Anemia Aplastic (Hypoplastic Bone Morrow) 280 Anemia Due to loss of Blood 281 Anemia Pernicious 280.9 Anemia, Iron Deficiency, Unspecified 285.9 Anemia, Unspecified (Normocytic, Not due to blood loss) 281.9 Anemia, Unspecified Deficiency (Macrocytic, Nutritional 441.5 Aneurysm Aortic, Ruptured 441.1 Aneurysm, Abdominal 441.3 Aneurysm, -

Flexible Video-Endsocopic Injection Sclerotherapy for Second and Third Degree Internal Hemorrhoids
Published online: 2019-09-26 ORIGINAL ARTICLE Flexible Video-Endsocopic Injection Sclerotherapy for Second and Third Degree Internal Hemorrhoids Sandeep Nijhawan, Udawat H, Gaurav Gupta, Anil Sharma, Amit Mathur, Bharat Sapra, Subhash Nepalia Department of Gastroenterology, SMS Medical College, Jaipur, Rajasthan, India ABSTRACT Background and objectives: Bleeding from hemorrhoids is the commonest cause of rectal bleeding in adults. Injection sclerotherapy of internal hemorrhoids is one of the non-surgical treatments, and is simple, safe and feasible. Conventionally sclerotherapy is performed with rigid proctoscope which has limitations of maneuverability, narrower field of vision and documentation compared to flexible videoendoscope. Therefore, we assessed the efficacy and safety of video-colonoscopic sclerotherapy for bleeding internal hemorrhides. Methods: Seventy-nine patients of bleeding internal hemorrhoids were subjected to colonoscopic sclerotherapy using 1.5% polidocanol in retroflexed or forward viewing positions. Success of treatment was defined as cessation of bleeding for six weeks. Patients were observed for complications and were followed up regularly for 3 months. Results: A total of 79 evaluable patients, 61 had grade II and 18 had grade III hemorrhoids. There was no statistically significant differences in achieving excellent or good results for control of bleeding between patients with grade II and grade III hemorrhoids (100% vs 94,5%; p>0.05). The number of sessions of sclerotherapy required were significantly more in grade II than grade III hemorrhoids (1.1 ± 0.3 vs 1.3 ± 0.7; p = 0.04). No significant complications were noted except for bloating in ten patients (12.6 %) and rectal pain in 6 (7.6%) patients. -

Venous Angiomas of the Brain A
- REVIEW ARTICLE systems," Venous angiomas may be Venous angiomas of quite small, draining a limited region of the brain, or may be very large, the brain a sometimes draining an entire hemi- • sphere. They can be single or multi- ple, and even bilateral.P" The com- review monest sites of occurrence are in the frontal and parietal lobes of the cere- venous anomaly' or DVA, pointing bral hemispheres and in the cerebel- Ian C Duncan out that these abnormalities actual- Ium.':" They can also be found in the ly represented an extreme anatomi- FFRad(D)SA occipital and temporal lobes, basal cal variant of the normal venous ganglia and pons." Unitas Interventional Unit POBox 14031 drainage of the brain. Lytlelton Imaging 0140 Pathology The classical radiographic appear- The theory of the development of ance of these abnormalities accurately venous angiomas is that there is fail- reflects the anatomical picture with Introduction ure of regression of normal embryon- multiple enlarged transmedullary Venous angiomas of the brain, also ic transmedullary venous channels. veins radiating in a wedge or radial termed venous malformations or These persistent transmedullary veins pattern toward the larger collecting developmental venous anomalies run axially through the white matter vein producing the pathognomic (DVA) are commonest of the to drain into a single larger calibre col- 'caput medusae' or 'spoke wheel' intracranial vascular malformations lecting venous trunk. The dilated ter- appearance during the venous phase comprising between 50% and 63% of minal collecting vein then penetrates of a cerebral angiogram (Figs 1,2).14,15 all intracranial vascular malforma- the cortex to drain either superficially A similar appearance is often seen on tions. -

National Clinical Coding Standards OPCS-4 (2018)
OPCS Classification of Interventions and Procedures Version 4.8 OPCS Classification of Interventions and Procedures Volume I - Tabular List I - Tabular Volume National Clinical Coding Standards OPCS-4 (2018) For more information please visit: Accurate data for quality information systems.digital.nhs.uk/data/clinicalcoding ISBN 978-0-11-323048-8 Terminology and Classifications Delivery Service www.tso.co.uk 9 780113 230488 9923 OPCS 4.8 Vol I Cover v0_2.indd 1-3 31/10/2016 10:00 National Clinical Coding Standards OPCS-4 Accurate data for quality information Produced by: Terminology and Classifications Delivery Service NHS Digital Vantage House 40 Aire Street Leeds LS1 4HT [email protected] http://systems.digital.nhs.uk/data/clinicalcoding Date of issue: April 2018 Copyright © 2018 Health and Social Care Information Centre The Health and Social Care Information Centre is a non-departmental body created by statute, also known as NHS Digital. OPCS-4 CONTENTS Introduction ............................................................................................................................ 3 Data Quality ........................................................................................................................... 7 National Clinical Coding Standards OPCS-4 reference book .............................................. 11 Rules of OPCS-4 ................................................................................................................. 16 Conventions of OPCS-4 ..................................................................................................... -

Presented: February 2, 2017 Thru February 4, 2017
2017 ACP Colorado Chapter Meeting February 2, 2017 thru February 4,2017 Broadmoor Hotel, Colorado Springs, Colorado Resident Abstracts Presented: February 2, 2017 thru February 4, 2017 2017 ACP Colorado Chapter Meeting – February 2, 2017 thru February 4, 2017 – Broadmoor Hotel – Colorado Springs, Colorado Name: Angela Burgin, MD Presentation Type: Oral Presentation Residency Program: University of Colorado School of Medicine Additional Authors: Winthrop Lockwood MS3, Katarzyna Mastalerz, MD Abstract Title: Use Clean Needles, Boil you Cotton: Advice for the Modern Drug User Abstract Information: Introduction: Fever in an intravenous drug abuser results in a wide differential diagnosis for the physician to consider, ranging from simple soft tissue infections to endocarditis or epidural abscess. This large breadth of possibilities often leads to dilemmas on which studies to order first, usually resulting in an expensive evaluation. We present one more option to add to the differential diagnosis in an IV drug user who presents with fever, with the hopes of increasing awareness of this condition to the medical community. Case Description: A 31 year old female with a history significant for IV drug abuse presented with dyspnea, chest pain, severe abdominal pain, right arm swelling, and generalized weakness for several days. She worked for a home health company and admitted to recently injecting hydromorphone and other opiates into her veins. Physical exam on admission was notable for a high fever, tachycardia, and right forearm edema, erythema, and induration, with a benign chest and abdominal exam. Ancillary studies revealed a urine toxicology positive for opiates, methadone, and cocaine, as well as a white blood cell count of 13. -

Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation
Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation. ФЕДЕРАЛЬНОЕ ГОСУДАРСТВЕННОЕ БЮДЖЕТНОЕ ОБРАЗОВАТЕЛЬНОЕ УЧРЕЖДЕНИЕ ВЫСШЕГО ОБРАЗОВАНИЯ «КУБАНСКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ» МИНИСТЕРСТВА ЗДРАВООХРАНЕНИЯ РОССИЙСКОЙ ФЕДЕРАЦИИ (ФГБОУ ВО КубГМУ Минздрава России) Кафедра пропедевтики внутренних болезней Department of Propaedeutics of Internal Diseases BASIC CLINICAL SYNDROMES Guidelines for students of foreign (English) students of the 3rd year of medical university Krasnodar 2020 2 УДК 616-07:616-072 ББК 53.4 Compiled by the staff of the department of propaedeutics of internal diseases Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation: assistant, candidate of medical sciences M.I. Bocharnikova; docent, c.m.s. I.V. Kryuchkova; assistent E.A. Kuznetsova; assistent, c.m.s. A.T. Nepso; assistent YU.A. Solodova; assistent D.I. Panchenko; docent, c.m.s. O.A. Shevchenko. Edited by the head of the department of propaedeutics of internal diseases FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation docent A.Yu. Ionov. Guidelines "The main clinical syndromes." - Krasnodar, FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation, 2019. – 120 p. Reviewers: Head of the Department of Faculty Therapy, FSBEI HE KubSMU of the Ministry of Health of Russia Professor L.N. Eliseeva Head of the Department