Nonsteroidal Antiinflammatory Drugs and Acute Renal Failure in Elderly Persons
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sulfinpyrazone 100Mg and 200Mg Tablets (Sulfinpyrazone)
Prescribing information sulfinpyrazone 100mg and 200mg tablets (sulfinpyrazone) Presentation: Coated tablets agents, sulphonamides, penicillin, theophylline, phenytoin, non- indication: Chronic, including tophaceous gout; recurrent gouty steroidal antirheumatic drugs. arthritis; hyperuricaemia Pregnancy and lactation: Used with caution in pregnant women, Dosage and administration: Route of administration: Oral. Adults: weighing the potential risk against the possible benefits. It is not known 100-200mg daily increasing gradually (over the first two or three whether the active substance or its metabolite(s) pass into breast milk. weeks) to 600mg daily (rarely 800mg), and maintained until the For safety reasons mothers should refrain from taking the drug. serum urate level has fallen within the normal range. Maintenance Undesirable effects: Mild transient gastro-intestinal upsets, such dose may be as low as 200mg daily. Children: Paediatric usage as nausea, vomiting, diarrhea, gastro-intestinal bleeding and not established. ulcers, acute renal failure, salt and water retention, allergic skin contraindications: Acute attacks of gout. Gastric and duodenal reactions, leucopenia, thrombocytopenia, agranulocytosis, aplastic ulcer. Known hypersensitivity to sulfinpyrazone and other pyrazolone anaemia, hepatic dysfunction, jaundice and hepatitis. derivatives. Contra-indicated in patients with asthma, urticaria, or (Please refer to the Summary of Product Characteristics for acute rhinitis, severe parenchymal lesions of the liver or kidneys, detailed information) porphyria, blood dyscrasias, haemorrhagic diatheses overdose: Nausea, vomiting, abdominal pains, diarrhoea, Precautions and warnings: Used with caution in patients with hypotension, cardiac arrhythmias, hyperventilation, respiratory hyperuricaemia or gout, episodes of urolithiasis or renal colic, disorders, impairment of consciousness, coma, epileptic seizures, ensure adequate fluid intake and alkalinisation of the urine during oliguria or anuria, acute renal failure, renal colic. -
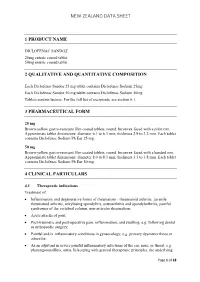
New Zealand Data Sheet
NEW ZEALAND DATA SHEET 1 PRODUCT NAME DICLOFENAC SANDOZ 25mg enteric coated tablet 50mg enteric coated tablet 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each Diclofenac Sandoz 25 mg tablet contains Diclofenac Sodium 25mg Each Diclofenac Sandoz 50 mg tablet contains Diclofenac Sodium 50mg Tablets contain lactose. For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM 25 mg Brown-yellow gastro-resistant film coated tablets, round, biconvex faced with a plain rim. Approximate tablet dimensions: diameter 6.1 to 6.3 mm; thickness 2.9 to 3.2 mm. Each tablet contains Diclofenac Sodium Ph Eur 25 mg. 50 mg Brown-yellow gastro-resistant film coated tablets, round, biconvex faced with a banded rim. Approximate tablet dimensions: diameter 8.0 to 8.3 mm; thickness 3.5 to 3.8 mm. Each tablet contains Diclofenac Sodium Ph Eur 50 mg. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of: • Inflammatory and degenerative forms of rheumatism - rheumatoid arthritis, juvenile rheumatoid arthritis, ankylosing spondylitis, osteoarthritis and spondylarthritis, painful syndromes of the vertebral column, non-articular rheumatism; • Acute attacks of gout; • Post-traumatic and post-operative pain, inflammation, and swelling, e.g. following dental or orthopaedic surgery; • Painful and/or inflammatory conditions in gynaecology, e.g. primary dysmenorrhoea or adnexitis; • As an adjuvant in severe painful inflammatory infections of the ear, nose, or throat, e.g. pharyngotonsillitis, otitis. In keeping with general therapeutic principles, the underlying Page 1 of 18 NEW ZEALAND DATA SHEET disease should be treated with basic therapy, as appropriate. Fever alone is not an indication. 4.2 Dose and method of administration Dosage Diclofenac Sandoz should only be prescribed when the benefits are considered to outweigh the potential risks. -

WO 2010/099522 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 2 September 2010 (02.09.2010) WO 2010/099522 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 45/06 (2006.01) A61K 31/4164 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/4045 (2006.01) A61K 31/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2010/025725 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 1 March 2010 (01 .03.2010) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, (26) Publication Language: English TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/156,129 27 February 2009 (27.02.2009) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (71) Applicant (for all designated States except US): ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, HELSINN THERAPEUTICS (U.S.), INC. -

S Salsalate Tablets
SALSALATE TABLETS CARDIOVASCULAR EFFECTS renal disease. If SALSALATE TABLETS therapy must be initiated, Rx Only Cardiovascular Thrombotic Events close monitoring of the patient’s renal function is advisable. Cardiovascular Risk Clinical trials of several COX-2 selective and nonselective NSAIDs Anaphylactoid Reactions • NSAIDs may cause an increased risk of serious cardiovascular of up to three years duration have shown an increased risk of As with other NSAIDs, anaphylactoid reactions may occur in thrombotic events, myocardial infarction, and stroke, which can serious cardiovascular (CV) thrombotic events, myocardial patients without known prior exposure to SALSALATE TABLETS. be fatal. This risk may increase with duration of use. Patients infarction, and stroke, which can be fatal. All NSAIDs, both COX-2 SALSALATE TABLETS should not be given to patients with the with cardiovascular disease or risk factors for cardiovascular selective and nonselective, may have a similar risk. Patients with aspirin triad. This symptom complex typically occurs in asthmatic disease may be at greater risk. (See WARNINGS and CLINICAL known CV disease or risk factors for CV disease may be at greater patients who experience rhinitis with or without nasal polyps, or TRIALS). risk. To minimize the potential risk for an adverse CV event in who exhibit severe, potentially fatal bronchospasm after taking • SALSALATE TABLETS is contraindicated for the treatment of patients treated with an NSAID, the lowest effective dose should be aspirin or other NSAIDs (see CONTRAINDICATIONS and perioperative pain in the setting of coronary artery bypass graft used for the shortest duration possible. Physicians and patients PRECAUTIONS - Preexisting Asthma). Emergency help should be (CABG) surgery (see WARNINGS Gastrointestinal Risk) should remain alert for the development of such events, even in sought in cases where an anaphylactoid reaction occurs. -

Highlights of Prescribing Information
HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------------CONTRAINDICATIONS------------------------------------- These highlights do not include all the information needed to use Patients with known hypersensitivity to natural or recombinant hirudins, IPRIVASK safely and effectively. See full prescribing information for and in patients with active bleeding and/or irreversible coagulation IPRIVASK. disorders (4). IPRIVASK® 15 mg (desirudin for injection), for subcutaneous injection -----------------------WARNINGS AND PRECAUTIONS----------------------------- Initial U.S. approval: 2003 • Hemorrhage: Bleeding can occur at any site during therapy with WARNING: SPINAL/EPIDURAL HEMATOMAS Iprivask. An unexplained fall in hematocrit or blood pressure should See Full Prescribing Information for complete boxed warning. lead to a search for a bleeding site. Avoid intramuscular injection as When neuraxial anesthesia (epidural/spinal anesthesia) or local bleeding and hematoma formation may result. (5.3). spinal puncture is employed, patients anticoagulated or • Increased Risk of bleeding with Renal Impairment: Dose reductions scheduled to be anticoagulated with selective inhibitors of by factors of three and nine are recommended for patients with thrombin such as Iprivask may be at risk of developing an moderate and severe renal impairment respectively (2.2). In addition, epidural or spinal hematoma which can result in long-term or daily aPTT and serum creatinine monitoring are recommended for permanent paralysis (5.1). patients with moderate -

Chemmart Meloxicam
Chemmart Meloxicam Capsules Meloxicam Consumer Medicine Information For a copy of a large print leaflet, Ph: 1800 195 055 What is in this leaflet Ask your doctor if you have any swelling of the feet or lips due to questions about why this medicine fluid build-up Read this leaflet carefully before has been prescribed for you. · You experience bleeding from the taking your medicine. Your doctor may have prescribed this stomach, gut or any other This leaflet answers some common medicine for another reason. bleeding questions about meloxicam. It does This medicine is available only with · You have had a stroke resulting not contain all the available a doctor©s prescription. from a bleed in the brain or have information. It does not take the a bleeding disorder place of talking to your doctor or How it works · You currently have a peptic pharmacist. Meloxicam belongs to a family of (stomach) ulcer All medicines have risks and medicines called Non-Steroidal Anti- · You are lactose intolerant (this benefits. Your doctor has weighed inflammatory Drugs (NSAIDs). medicine contains lactose) the risks of you using this medicine These medicines work by relieving · You have Crohn©s Disease or against the benefits they expect it pain and inflammation. Ulcerative Colitis will have for you. There is no evidence that this · You have severe liver or kidney Keep this leaflet with your medicine is addictive. problems medicine. · You are currently taking other You may want to read it again. medicines known as: sulfinpyrazone (used to treat Before you take this gout), fluconazole (used to treat medicine fungal infections) or certain What this medicine is sulfur antibiotics (e.g. -

Information for the User Diclofenac / Omeprazole Modified-Release
Package Leaflet: Information for the User Diclofenac / Omeprazole modified-release capsules, hard, 75 mg / 20 mg diclofenac sodium/omeprazole Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Keep this leaflet. You may need to read it again. If you have any further questions, please ask your doctor or pharmacist. This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Diclofenac / Omeprazole modified-release capsules, hard, 75 mg / 20 mg is and what it is used for 2. What you need to know before you take Diclofenac / Omeprazole modified-release capsules, hard, 75 mg / 20 mg 3. How to take Diclofenac / Omeprazole modified-release capsules, hard, 75 mg / 20 mg 4. Possible side effects 5. How to store Diclofenac / Omeprazole modified-release capsules, hard, 75 mg / 20 mg 6. Contents of the pack and other information 1. What Diclofenac / Omeprazole modified-release capsules, hard, 75 mg / 20 mg is and what it is used for Diclofenac / Omeprazole modified-release capsules, hard, 75 mg / 20 mg contains two active ingredients in a single capsule. These active ingredients are diclofenac sodium (75 mg) and omeprazole (20 mg). Diclofenac is one of a group of medicines called non-steroidal anti-inflammatory drugs (NSAIDs) and is used to reduce pain and inflammation of joint disorders. -

Gastro-Duodenal Ulcers Associated with the Use of Non-Steroidal Anti-Inflammatory Drugs: a Systematic Review of Preventive Pharmacological Interventions
Gastro-duodenal Ulcers Associated with the Use of Technology Non-steroidal Anti- inflammatory Drugs: A Systematic Review Report of Preventive Issue 38 September 2003 Pharmacological Interventions Publications can be requested from: CCOHTA 600-865 Carling Avenue Ottawa, Ontario, Canada K1S 5S8 Tel. (613) 226-2553 Fax. (613) 226-5392 Email: [email protected] or download from CCOHTA’s web site: http://www.ccohta.ca Cite as: Rostom A, Dubé C, Jolicoeur E, Boucher M, Joyce J. Gastro-duodenal ulcers associated with the use of non-steroidal anti-inflammatory drugs: a systematic review of preventive pharmacological interventions. Ottawa: Canadian Coordinating Office for Health Technology Assessment; 2003. Technology report no 38. Reproduction of this document for non-commercial purposes is permitted provided appropriate credit is given to CCOHTA. CCOHTA is a non-profit organization funded by the federal, provincial and territorial governments. Legal Deposit - 2003 National Library of Canada ISBN: 1-894620-92-5 (print) ISBN: 1-894620-93-3 (electronic version) Publications Mail Agreement Number: 40026386 Canadian Coordinating Office for Health Technology Assessment Gastro-duodenal Ulcers Associated with the Use of Non-steroidal Anti-inflammatory Drugs: A Systematic Review of Preventive Pharmacological Interventions Alaa Rostom MD MSc FRCPC1 1 Catherine Dubé MD MSc FRCPC 1 Emilie Jolicoeur MD 2 Michel Boucher BPharm MSc 2 Janet Joyce MLS September 2003 ________________________ 1 University of Ottawa, Ottawa, Ontario 2 Canadian Coordinating Office for Health Technology Assessment, Ottawa, Ontario Reviewers These individuals kindly provided comments on this report. External Reviewers Isabelle Chabot, PhD Betsy Miller, BScPharm MSc Manager, Health Economics and Executive Director Outcomes Research Patient Access and Outcomes Research Merck Frosst Canada & Co. -

New Zealand Data Sheet IBUPROFEN LIQUID CAPSULES
New Zealand Data Sheet IBUPROFEN LIQUID CAPSULES Neo Health Ibuprofen liquid capsules 400mg 1 PRODUCT NAME Ibuprofen 400mg Liquid capsules 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each capsule contains Ibuprofen 400 mg. For full list of excipients, see section 6.1 3.PHARMACEUTICAL FORM Capsule, soft Natural transparent, oval shaped, soft gelatin capsule containing clear colourless liquid. imprinted with L 160 in Black edible ink. 4.CLINICAL PARTICULARS 4.1 Therapeutic indications This medical product is indicated in adults and children & adolescents 12 years of age and over for the symptomatic treatment of mild to moderate pain and/or inflammation associated with headache, migraine, tension headache, muscular pain, dental pain, period pain, sinus pain, back pain, arthritis pain, cold and flu symptoms. 4.2 Dosage and administration For oral use and short-term use only. Capsules should not be chewed. Undesirable effects may be minimized by using the lowest effective dose for the shortest possible duration necessary to control symptoms (see section 4.4) Adults and children & adolescents 12 years of age and over. Initial dose, one capsule with water. Then, if necessary, one capsule every six hours. Do not exceed six capsules (2400 mg) in any 24-hour period. If in children and adolescents between 12 and 18 years this medicinal product is required for 3 days, or if symptoms worsen a doctor should be consulted. If in adults the product is required for more than 3 days in the case of fever and 4 days for treatment of pain, or if the symptoms worsen the patient is advised to consult a doctor. -

Vinblastine and Sulfinpyrazone Export by the Multidrug Resistance Protein MRP2 Is Associated with Glutathione Export
British Journal of Cancer (2000) 83(3), 375–383 © 2000 Cancer Research Campaign doi: 10.1054/ bjoc.2000.1262, available online at http://www.idealibrary.com on Vinblastine and sulfinpyrazone export by the multidrug resistance protein MRP2 is associated with glutathione export R Evers1,4, M de Haas1, R Sparidans2, J Beijnen2, PR Wielinga3, J Lankelma3 and P Borst1 1Division of Molecular Biology and Center of Biomedical Genetics, The Netherlands Cancer Institute, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Pharmacy, Slotervaart Hospital, Louwesweg 6, 1066 EC Amsterdam, The Netherlands; 3Academic Hospital Vrije Universiteit, Department of Medical Oncology, Room BR232, PO Box 7057, 1007 MB Amsterdam, The Netherlands; 4Present address Georg-Speyer-Haus, Paul Ehrlich straße 42–44, 60596 Frankfurt am, Germany Summary The multidrug resistance proteins MRP1 and MRP2 are members of the same subfamily of ATP-binding cassette transporters. Besides organic molecules conjugated to negatively charged ligands, these proteins also transport cytotoxic drugs for which no negatively charged conjugates are known to exist. In polarized MDCKII cells, MRP1 routes to the lateral plasma membrane, and MRP2 to the apical plasma membrane. In these cells MRP1 transports daunorubicin, and MRP2 vinblastine; both transporters export reduced glutathione (GSH) into the medium. We demonstrate that glutathione transport in MDCKII-MRP1 cells is inhibited by the inhibitors of organic anion transporters sulfinpyrazone, indomethacin, probenecid and benzbromarone. In MDCKII-MRP2 cells, GSH export is stimulated by low concentrations of sulfinpyrazone or indomethacin, whereas export is inhibited down to control levels at high concentrations. We find that unmodified sulfinpyrazone is a substrate for MRP2, also at concentrations where GSH export is inhibited. -
Ibuprofen 600 Mg Film- Coated Tablets
Package leaflet: Information for the user You should discuss your treatment with your doctor or pharmacist before taking Ibuprofen if Ibuprofen 600 mg film- you: • have heart problems including heart failure, coated tablets angina (chest pain), or if you have had a heart attack, bypass surgery, peripheral Read all of this leaflet carefully before artery disease (poor circulation in the legs you start taking this medicine because it or feet due to narrow or blocked arteries), or contains important information for you. any kind of stroke (including ‘mini-stroke’ or - Keep this leaflet. You may need to read it transient ischaemic attack “TIA”). again. • have high blood pressure, diabetes, high - If you have any further questions, ask your cholesterol, or have a family history of heart doctor or pharmacist. disease or stroke, or if you are a smoker. - This medicine has been prescribed for you Effects on the kidneys only. Do not pass it on to others. It may Ibuprofen may cause problems with kidney harm them, even if their signs of illness are function even in patients who have not had the same as yours. kidney problems before. This may result in - If you get any side effects, talk to your swelling of the legs and may even lead to heart doctor or pharmacist. This includes any failure or high blood pressure in predisposed possible side effects not listed in this leaflet. individuals. See section 4. Ibuprofen may cause kidney damage especially What is in this leaflet in patients who already have kidney, heart or 1. What Ibuprofen is and what it is used for liver problems, or are taking diuretics or ACE 2. -

Salicylic Acid 6% Foam
Salicylic Acid 6% Foam (salicylic acid in a water and lipid based foam, 6%) Rx Only DESCRIPTION Salicylic Acid 6% Foam is applied topically and used in the removal of excessive keratin in hyperkeratotic skin disorders. Active Ingredient: Salicylic Acid 6% Inactive Ingredients: Butane, Carthamus Tinctorius (Safflower) Seed Oil, Cocamidopropyl Dimethylamine, Diazolidinyl Urea, Ethylhexylglycerin, Glycerin, Methylparaben, Olea Europaea (Olive) Fruit Oil, Phenoxyethanol, Polysorbate 20, Polysorbate 80, Propane, Propylene Glycol, Propylparaben, Sodium C14-16 Olefin Sulfonate, Sodium Hydroxide, Water. CHEMICAL STRUCTURE Salicylic acid is a 2-hydroxy derivative of benzoic acid having the following chemical structure: CO2H OH CLINICAL PHARMACOLOGY Salicylic acid has been shown to produce desquamation of the horny layer of skin while not affecting qualitative or quantitative changes in structure of the viable epidermis. The mechanism of action has been attributed to dissolution of intercellular cement substance. In a study of the percutaneous absorption of salicylic acid from Salicylic Acid 6% Foam in four patients with extensive active psoriasis, Taylor and Halprin showed that peak serum levels never exceeded 5 mg/100 mL even though more than 60% of the applied salicylic acid was absorbed. Systemic toxic reactions are usually associated with much higher serum levels (30 to 40 mg/100mL). Peak serum levels occurred within 5 hours of the topical application under occlusion. The sites were occluded for 10 hours over the entire body surface below the neck. Since salicylates are distributed in the extracellular space, patients with a contracted extracellular space due to dehydration or diuretics have higher salicylate levels than those with a normal extracellular space.