Julie Mart C. Rubite, MD, FPAFP, MMHA Program Manager National Leprosy Control Program Department of Health Philippines OUTLINE I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Regional Prosecutors
REGIONAL PROSECUTORS LOCATION CHIEF PROSECUTOR CONTACT NUMBERS FAX EMAIL Region I ORP La Union (072) 242-7311 [email protected] NONNATUS CAESAR R. ROJAS (072) 242-7311 San Fernando City, La Union (072) 700-0770 [email protected] La Union Regional Prosecutor OPP Abra Nestor S. Tolentino (074) 752-8617 [email protected] Justice Hall,Bangued, Abra OPP Benguet Andres M. Gondayao (OIC) (074) 422-4680 (074) 422-2303 [email protected] Justice Hall, La Trinidad, Benguet OPP Ilocos Norte Rommel G. Calupig (OIC) (077) 772-1139 [email protected] Laoag City, Ilocos Norte OPP Ilocos Sur Robert V. Canosa (077) 722-2745 Vigan City, Ilocos Sur OPP La Union Sevilla Justice Hall, Sevilla Danilo C. Bumacod (072) 888-3072 San Fernando City, La Union OPP Mountain Province Golda C. Bagawi Bontoc, Mountain Province OPP Pangasinan Office of the Provincial Prosecutor, Abraham L. Ramos II (075) 542-4734 Hall of Justice, Lingayen, Pangasinan OCP Alaminos City (075) 551-3030 Cristobal G. Caalaman (OIC) (075) 552-7049 Alaminos City (075) 551-3039 OCP Baguio City Elmer M. Sagsago (074) 442-5832 (074) 442-5953 City Hall, Baguio City OCP Batac City Valentin L. Pascua, Jr. (077) 670-1828 [email protected] Batac City, Ilocos Norte OCP Candon City [email protected] Emmylou Rubang-Mangasar (077) 742-5402 Candon City, Ilocos Sur [email protected] OCP Dagupan City Elmer M. Surot (OIC) (075) 523-6728 [email protected] Dagupan City OCP Laoag City Lourdes M. Layugan (077) 772-1491 Laoag City, Ilocos Norte OCP San Carlos City Mitchel A. -
List of Licensed Covid-19 Testing Laboratory in the Philippines
LIST OF LICENSED COVID-19 TESTING LABORATORY IN THE PHILIPPINES ( as of November 26, 2020) OWNERSHIP MUNICIPALITY / NAME OF CONTACT LICENSE REGION PROVINCE (PUBLIC / TYPE OF TESTING # CITY FACILITY NUMBER VALIDITY PRIVATE) Amang Rodriguez 1 NCR Metro Manila Marikina City Memorial Medical PUBLIC Cartridge - Based PCR 8948-0595 / 8941-0342 07/18/2020 - 12/31/2020 Center Asian Hospital and 2 NCR Metro Manila Muntilupa City PRIVATE rRT PCR (02) 8771-9000 05/11/2020 - 12/31/2020 Medical Center Chinese General 3 NCR Metro Manila City of Manila PRIVATE rRT PCR (02) 8711-4141 04/15/2020 - 12/31/2020 Hospital Detoxicare Molecular 4 NCR Metro Manila Mandaluyong City PRIVATE rRT PCR (02) 8256-4681 04/11/2020 - 12/31/2020 Diagnostics Laboratory Dr. Jose N. Rodriguez Memorial Hospital and (02) 8294-2571; 8294- 5 NCR Metro Manila Caloocan City PUBLIC Cartridge - Based PCR 08/13/2020 - 12/31/2020 Sanitarium 2572 ; 8294-2573 (GeneXpert)) Lung Center of the 6 NCR Metro Manila Quezon City PUBLIC rRT PCR 8924-6101 03/27/2020 - 12/31/2020 Philippines (LCP) Lung Center of the 7 NCR Metro Manila Quezon City Philippines PUBLIC Cartridge - Based PCR 8924-6101 05/06/2020 - 12/31/2020 (GeneXpert) Makati Medical Center 8 NCR Metro Manila Makati City PRIVATE rRT PCR (02) 8888-8999 04/11/2020 - 12/31/2020 (HB) Marikina Molecular 9 NCR Metro Manila Marikina City PUBLIC rRT PCR 04/30/2020 - 12/31/2020 Diagnostic laboratory Philippine Genome 10 NCR Metro Manila Quezon City Center UP-Diliman PUBLIC rRT PCR 8981-8500 Loc 4713 04/23/2020 - 12/31/2020 (NHB) Philippine Red Cross - (02) 8790-2300 local 11 NCR Metro Manila Mandaluyong City PRIVATE rRT PCR 04/23/2020 - 12/31/2020 National Blood Center 931/932/935 Philippine Red Cross - 12 NCR Metro Manila City of Manila PRIVATE rRT PCR (02) 8527-0861 04/14/2020 - 12/31/2020 Port Area Philippine Red Cross 13 NCR Metro Manila Mandaluyong City Logistics and PRIVATE rRT PCR (02) 8790-2300 31/12/2020 Multipurpose Center Research Institute for (02) 8807-2631; (02) 14 NCR Metro Manila Muntinlupa City Tropical Medicine, Inc. -

Sec Express Nationwide Submission (Sens)
North And Central Luzon Southern Luzon Region Visayas Name Address & Contact Info Name Address & Contact Info Name Address & Contact Info BSO Gound Operations Airfreight Ground Floor Manlapaz Bldg., Door #1 Arches Bldg., Arnaldo DAET ROXAS CITY 2100 Unit 6 De Leon Diaz Bldg., Gov. Panotes Ave., Daet BALANGA BATAAN Blvd, Roxas City, Capiz, 5800 Manahan St., Tinejero Balanga Air21 Bldg., LGB Compound Lower Ground Floor SM City Bataan LEGASPI CITY Lakandula Drive Brgy. 40 SM CITY, CEBU CITY North Reclamation Area, Cebu Washington St. Brgy. 2 Ablan, Cruzada Legaspi City City BATAC, ILOCOS NORTE Batac City, Ilocos Norte QVC Plaza Bldg., Tagbilaran Ground Floor CNM Building, Illus- TAGBILARAN CITY 2nd Floor McDo Bldg. Corner LEMERY, BATANGAS City, Bohol BAYOMBONG, NUEVA tre Avenue, Lemery, Batangas Mabini St. B. Aquino Ave., Solano, 2nd Floor, Gaisano Fiesta Mall, VIZCAYA TALISAY, CEBU CITY Nueva Vizcaya Neo-Francis Bldg., Paninsingin, Tabunok, Talisay City, Cebu LIPA CITY 467 Consejo St., Quezon District, Tambo, Lipa City Mindanao CABANATUAN CITY Cabanatuan City Chair Bldg., Stall 1, Lopez Ave., LOS BAÑOS, LAGUNA Batong Malake, Los Baños, Name Address & Contact Info Northeast Cabatuan Road, Baran- CAUAYAN, ISABELA Laguna gay San Fermin , Cauayan, Isabela Nepomuceno St. Barangay San Door 1 M. U. Bldg., J. C. Aquino MARINDUQUE BUTUAN CITY Gabayans Compound National Miguel Boac, Marinduque Ave., Tandang Sora, Butuan City CANDON, ILOCOS SUR Hi-way Candon City, Ilocos Sur Nepomuceno St. Barangay San MARINDUQUE Mc-Arthur Highway, San Miguel, Miguel Boac, Marinduque Airfreight 2100 Cagayan De Oro CALASIAO, PANGASINAN CAGAYAN DE ORO CITY Calasiao, Pangasinan Rodson Bldg., J. Hernandez Ave., City NAGA CITY Cargohaus Bldg., Clark, Naga City CLARK Purok 4, Gov. -

Table of Contents
TABLE OF CONTENTS Sangguniang Panlungsod Resolution Adopting the City of i Batac Citizen's Charter, 2017 Edition Messages City Mayor ii City Vice-Mayor iii Introduction / Foreword iv FACTS ABOUT THE CITY Vision and Mission of the City 1 Brief Historical Background of the City 2 Geo-Physical Characteristics 6 Population and Demographic Profile 11 Performance Pledge (City Government of Batac) 22 CITY FRONTLINE SERVICES I. EXECUTIVE SERVICES A. Office of the Mayor 1 Performance Pledges 23 2 Securing Mayor’s Clearance 25 3 Request for Mayor’s Approval to Hang 26 Streamer(s) 4 Request for Mayor’s Approval to Conduct 28 Advertising and Promotional Activities 5 Request for Solemnization of Marriage 29 6 Request for the Use of the Imelda Cultural Center/City Basketball Court, City Tourist 30 Buses, Kalipi Training Center, and City Equipment 7 Request for the Use of the City Ambulance 32 8 Securing Mayor's Endorsement to Cut Tree(s) 35 9 Request for Mayor's Permit for a Not-for-Hire 37 (Private) Tricycle 10 Securing Mayor's Permit for Fund Raising Activities/Silicitation 39 11 Securing Mayor's Permit to Conduct Motorcade or Procession 41 12 Seeking Mayor's Approval on Barangay 43 Request(s) 13 Request for a Discounted Rate of Burial Plot at 45 the City Cemetery 14 Securing Mayor's Endorsement to Borrow Blood 47 15 Application for the Junior City Scholarship 48 Program B. Human Resource Management Office 1 Vision 50 2 Mission 50 3 Performance Pledges 50 4 Answering Inquiries on Application for 51 Employment 5 Issuance of Service Record/Certificate of 52 Employment and Other HR Records 6 Initial Processing of Terminal Leave Pay 53 C. -
PHILRICE-BATAC Branch-Based Highlights
Branch-Based Highlights PHILRICE-BATAC Branch-Based Highlights TABLE OF CONTENTS Page Executive Summary 1 A. Development I. Clean, Green, Practical and Smart On-Farm Learning 2 Center (BIN-032-000) II. One-Stop Shop for Technology Information and 8 Promotion of Rice and Rice-based Knowledge Products (BIN-033-000) III. Agromet-Batac (BIN-035-000) 17 IV. PhilRice Batac Intensified Rice-Based Agri-Bio Systems 18 (BIN-036-000) V. PalaYamaNayon the Rural Transformation Movement 23 (BIN-037-000) VI. Be Riceponsible Campaign (BIN-038-000) 27 VII. Agribusiness Analysis of IRBAS Enterprises (IRB-016- 29 000) VIII. Accelerating Development, Demonstration and 30 Adoption of Palayamanan Plus in Lowland Farms (171A-RTF-022) IX. Accelerating the Development and Dissemination 32 of Associated Rice Production Technologies that are Resource-Use Efficient (172A-Y3-RTF-002) X. Knowledge Sharing and Learning (174D-RTF-022) 34 XI. Philippine Rice Information System (PRiSM) An 35 Operational System for Rice Monitoring to Support Decision Making towards Increased Rice Production in the Philippines (175A-RTF-022) XII. Purification, Multiplication and Commercialization of 37 Selected Aromatic Upland Rice Varieties in Support to the DA’s Initiative on Rice Exportation (176D-Y2-RTF-002) XIII. Field Demonstration of New Rainfed Varieties (Sahod 39 Ulan) in Rainfed Lowland Rice (590-RTF-003) Branch-Based Highlights Branch-Based Highlights TABLE OF CONTENTS TABLE OF CONTENTS Page Page XIV. Agricultural Support Component-National Irrigation 40 XI. Pre-harvest and post-harvest management for aromatic 69 Sector Rehabilitation and Improvement Project (633-RTF- and organic rice (HVP-002-005) 194) XII. -

International Journal of Education and Research Vol. 9 No. 2 February 2021
International Journal of Education and Research Vol. 9 No. 2 February 2021 FESTIVALS OF ILOCOS NORTE: A CONTEXTUAL REVIEW OF VALUES AND CULTURE IN NORTHERN PHILIPPINES JASPER KIM M. RABAGO Author Assistant Professor Mariano Marcos State University Laoag City, Ilocos Norte, Philippines email: [email protected] 55 ISSN: 2411-5681 www.ijern.com ABSTRACT The study was conducted to develop and validate a series of pamphlets on selected festivals of Ilocos Norte. The descriptive approach was used and adapted the research and development (R and D) methodology. The social studies curriculum in the elementary and secondary schools in the Philippine K to 12 is designed to teach and strengthen the learners’ knowledge and understanding of local history. Part of teaching the concepts is integrating cultural values that are manifested in the various localities’ ways of life. Research and studies on cultural festivals were surveyed and first hand interview with key informants in the various local government units were done to determine the historical origin and values that are manifested in the festivals. The results of the survey were used as bases in the development of pamphlets on selected festivals of Ilocos Norte that could be used in teaching local history and values. The pamphlet comes in a series (1-6) form and has the following parts namely: A Cultural Celebration, The Town and Its People, Social Organization, A Reflection of the People’s Culture, and The Cultural Values and Highlights. Festivals were chosen based on their geographical place of origin. Hence, all the festivals were equally represented. Two festivals, Currimao’s Dinaklisan and Pasuquin’s Dumadara were chosen from the coastal area, from the upland area are Carasi’s Magdadaran Talip and Dumalneg’s Panagwawagi, and from the lowland area are Batac City’s Empanada and Dingras’ Ani. -

Region Name of Laboratory I A.G.S. Diagnostic and Drug
REGION NAME OF LABORATORY I A.G.S. DIAGNOSTIC AND DRUG TESTING LABORATORY I ACCU HEALTH DIAGNOSTICS I ADH-LENZ DIAGNOSTIC LABORATORY I AGOO FAMILY HOSPITAL I AGOO LA UNION MEDICAL DIAGNOSTIC CENTER, INC. I AGOO MEDICAL CLINICAL LABORATORY I AGOO MUNICIPAL HEALTH OFFICE CLINICAL LABORATORY I ALAMINOS CITY HEALTH OFFICE LABORATORY I ALAMINOS DOCTORS HOSPITAL, INC. I ALCALA MUNICIPAL HEALTH OFFICE LABORATORY I ALLIANCE DIAGNOSTIC CENTER I APELLANES ADULT AND PEDIATRIC CLINIC & LABORATORY I ARINGAY MEDICAL DIAGNOSTIC CENTER I ASINGAN DIAGNOSTIC CLINIC I ATIGA MATERNITY AND DIAGNOSTIC CENTER I BACNOTAN DISTRICT HOSPITAL I BALAOAN DISTRICT HOSPITAL I BANGUI DISTRICT HOSPITAL I BANI - RHU CLINICAL LABORATORY I BASISTA RURAL HEALTH UNIT LABORATORY I BAUANG MEDICAL AND DIAGNOSTIC CENTER I BAYAMBANG DISTRICT HOSPITAL I BETHANY HOSPITAL, INC. I BETTER LIFE MEDICAL CLINIC I BIO-RAD DIAGNOSTIC CENTER I BIOTECHNICA DIAGNOSTIC LABORATORY I BLESSED FAMILY DOCTORS GENERAL HOSPITAL I BLOODCARE CLINICAL LABORATORY I BOLINAO COMMUNITY HOSPITAL I BUMANGLAG SPECIALTY HOSPITAL (with Additional Analyte) I BURGOS MEDICAL DIAGNOSTIC CENTER CO. I C & H MEDICAL AND SURGICAL CLINIC, INC. I CABA DISTRICT HOSPITAL I CALASIAO DIAGNOSTIC CENTER I CALASIAO MUNICIPAL CLINICAL LABORATORY I CANDON - ST. MARTIN DE PORRES HOSPITAL (REGIONAL) I CANDON GENERAL HOSPITAL (ILOCOS SUR MEDICAL CENTER, INC.) REGION NAME OF LABORATORY I CANDON ST. MARTIN DE PORRES HOSPITAL I CARDIO WELLNESS LABORATORY AND DIAGNOSTIC CENTER I CHRIST-BEARER CLINICAL LABORATORY I CICOSAT HOSPITAL I CIPRIANA COQUIA MEMORIAL DIALYSIS AND KIDNEY CENTER, INC. I CITY GOVERNMENT OF BATAC CLINICAL LABORATORY I CITY OF CANDON HOSPITAL I CLINICA DE ARCHANGEL RAFAEL DEL ESPIRITU SANTO AND LABORATORY I CLINIPATH MEDICAL LABORATORY I CORDERO - DE ASIS CLINIC X-RAY & LABORATORY I CORPUZ CLINIC AND HOSPITAL I CUISON HOSPITAL, INC. -

Pdf | 270.43 Kb
2. Casualties 5 Two (2) persons were reported missing: one (1) in Silangan, San Mateo Rizal identified as Arnold Julian (9 yrs old), fell down in a manhole and the other one in Imus, Cavite identified as Jonathan Hormeneta (22 years old) slipped while crossing a bridge in Shelter Town, Imus, Cavite. Allegedly, he fell in “Buhay na Tubig” and believed to be swept by strong current of water 5 One (1) person identified as Joemar Ligara, 13 years old was reported dead in Caloocan City North Brgy160 due to drowning in Tullahan River 5 One (1) person identified as Lomer Fernando, 32 years old of Brgy 12, Palpalicong, Batac, Ilocos Norte was reported dead due to electrocution 3. Damages Region IV-A 5 Based on the initial assessment of DPWH IV-A, damage to roads in Laguna is PhP380,000.00 5 A landslide in Buntong Palay, San Mateo, Rizal has caused the damage of 8 houses (5 totally and 3 partially) 4. Flood Monitoring NCR - At the height of the storm there were 30 barangays flooded in nine (9) cities of Metro Manila namely: Pasig, San Juan, Caloocan, Marikina, Manila, Valenzuela, Malabon, Muntinlupa and Makati with flood waters ranging from 8 inches to knee-deep. Flood waters in these areas have already subsided Region I 5 Cumulative total number of houses affected by flooding in Ilocos Norte were 6,752: and 545 were isolated due to flooding: Location Cumulative Total Affected Isolated due to Flooing Dingras 2,560 Nueva Era 95 Paoay 1,213 Batac 921 Adams 405 Pinili 243 Piddig 60 San Nicolas 678 Banna 40 Marcos 57 Solsona 142 Sarrat 105 Pasuquin 733 45 5. -

Preventive Maintenance
BIDS AND AWARDS COMMITTEE – SECURITY PLANT COMPLEX CHECKLIST OF REQUIREMENTS FOR BIDDERS (Procurement of Goods/Services) Title of : One (1) lot Preventive Maintenance Services of Requirement Electronic Security Systems in Various BSP Branches, as per BSP Terms of Reference: Item 1 - Luzon Area [Five (5) BSP Branches in Batac, Dagupan, Cabanatuan, San Fernando Pampanga, and Tuguegarao] Item 2 - South Luzon Area [Three (3) BSP Branches in Lucena, Naga and Legazpi] Item 3 - Visayas Area [Five (5) BSP Branches in Bacolod, Dumaguete, Iloilo, Roxas, and Tacloban] Item 4 - Mindanao Area [Six (6) BSP Branches in Butuan, Cotabato, Cagayan De Oro, General Santos, Ozamis, and Zamboanga] PIN : BAC-SPC GS No. 2021-0233 dated 16 June 2021 Approved Budget : Php7,800,00.00, VAT inclusive for the Contract Bidder : ______________________________________________ BIDDERS SHALL SUBMIT ONE (1) SET OF DOCUMENTS UNDER ENVELOPE NOS. 1 TO 3. ENVELOPE No. 1 - ELIGIBILITY AND TECHNICAL REQUIREMENTS ENVELOPE The preliminary examination of bids shall use a non-discretionary “pass/fail” criterion. If a bidder submits the required document, it shall be rated “passed” for that particular requirement. In this regard, bids that fail to include any requirement or are incomplete or patently insufficient shall be considered as “failed”. Otherwise, the BAC shall rate Envelope No. 1 as “passed”. (Rule IX, Section 30.1) (To be filled-up by the BSP Evaluator during the Preliminary Examination of Bids) P F CONTENTS OF A A REMARKS DOCUMENT S I S L I. ELIGIBILITY DOCUMENTS1 Class “A” Documents 1. Philippine Government Electronic Procurement System (PhilGEPS) Platinum Reg./Cert. No.: ______ 1 Photocopies unless indicated as original copy. -

REPORT on GOVERNMENT PROGRAM/PROJECTS/ACTIVITIES Bureau of Jail Management and Penology for the Year 2015
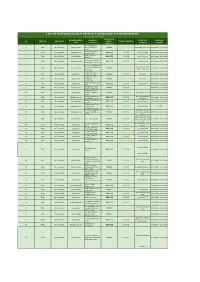
REPORT ON GOVERNMENT PROGRAM/PROJECTS/ACTIVITIES Bureau of Jail Management and Penology For the Year 2015 CONTRACT SOURCE OF DATE TARGET ITEM PROJECTS NAME OF JAIL / LOCATION ABC AMOUNT FUND CONTRACTOR DATE STARTED COMPLETED COMPLETION REMARKS REPAIR AND MAINTENANCE FIRST QUARTER ROOF REPAIR OF THE WARDEN'S BALAOAN DISTRICT JAIL/ SHINE MAE 1 OFFICE AND JAIL KITCHEN BALAOAN,LA UNION P 26,000.00 P 25,180.00 MOOE CONSTRUCTION 11-Feb-15 19-Feb-15 25-Feb-15 COMPLETED/PAID BALUNGAO DISTRICT JAIL/ SHINE MAE 2 INSTALLATION OF COMBAT WIRE BALUNGAO,PANGASINAN P 94,500.00 P 93,060.00 MOOE CONSTRUCTION 10-Mar-15 23-Mar-15 25-Mar-15 COMPLETED/PAID BATAC DISTRICT JAIL/ SHINE MAE 3 INSTALLATION OF COMBAT WIRE BATAC, ILOCOS NORTE P 23,000.00 P 22,300.00 MOOE CONSTRUCTION 13-Feb-15 20-Feb-15 23-Feb-15 COMPLETED/PAID BAUANG DISTRICT JAIL/ COMPASS ROSE 4 INSTALLATION OF COMBAT WIRE BAUANG,LA UNION P 81,500.00 P 80,420.00 MOOE BUILDERS 9-Mar-15 24-Mar-15 24-Mar-15 COMPLETED/PAID BURGOS DISTRICT JAIL/ DWELLSIGNERS 5 CONSTRUCTION OF SALLY PORT BURGOS,PANGASINAN P 300,000.00 P 297,740.00 MOOE BUILDERS 16-Feb-15 26-Mar-15 26-Mar-15 COMPLETED/PAID CANDON CITY JAIL/ CANDON SHINE MAE 6 PLASTERING OF PERIMETER FENCE CITY,ILOCOS SUR P 139,590.00 P 138,760.00 MOOE CONSTRUCTION 26-Feb-15 12-Mar-15 11-Apr-15 COMPLETED/PAID DAGUPAN CITY JAIL/ SHINE MAE 7 INSTALLATION OF COMBAT WIRE DAGUPAN,PANGASINAN P 145,000.00 P 143,820.00 MOOE CONSTRUCTION 5-Mar-15 20-Mar-15 20-Mar-15 COMPLETED/PAID DAGUPAN CITY JAIL-FD/ SHINE MAE 8 CONSTRUCTION OF NEW KITCHEN DAGUPAN,PANGASINAN -

Hoval Final Ronnel.P65
Toxic Debt The Onerous Austrian Legacy of Medical Waste Incineration in the Philippines EEEcccological WWWaste Coalition of the Philippines,,, Inc... The Eco logical Waste Coalition of the Philippines, Inc. is a public interest network of community, church, school, environmental and public health groups that are committed to the pursuit of ecologically sustainable and socially just solutions to managing waste. The Coalition works to achieve a zero-waste society in the Philippines by 2020, and is guided by 5 key principles: (1) SIMPLE SOLUTIONS on the (2) LOCAL level, using an (3) INTEGRATED APPROACH to harness local talents and energies to ensure that the local community enjoys (4) ECONOMIC BENEFITS in a (5) SUSTAINABLE MANNER. The Coalition has initiated or supported citizens’ campaigns on the closure of dumps, landfills, and incinerators. Its advocacies also include extended producers’ responsibility and the regulation of the use of plastic materials. Eco Waste Coalition of the Philippines Unit 320 Eagle Court Condominium 26 Matalino Street, Diliman Quezon City, Philippines 1101 Tel (632) 929-0376 Fax (632) 436-4733 www.ecowastecoalition.blogspot.com TOXIC DEBT 5 Background THE PROPER DISPOSAL of waste generated by health care facilities is of special public health concern. Although a large part of the waste collected from health care facilities is comparable to the waste generated by regular households, a small but significant portion of that waste is considered hazardous and thus requiring special treatment and disposal procedures. Most of the hazardous waste produced by hospitals are infectious medical waste, the type of waste that is suspected to contain pathogens (bacteria, viruses, parasites or fungi). -

January 2020 Death Statistics in Ilocos Region.Pdf
Death Statistics Ilocos Region: January 2020 Date of Release: 14 October 2020 Reference No.: 2020-47 Data on deaths presented in this release were obtained from the Certificate of Death (Municipal Form 103) that were registered at the Office of the City/Municipal Civil Registrars and forwarded to the Philippine Statistics Authority - Provincial Statistical Offices in Ilocos Region. Information included deaths registered in January 2019 and in January 2020. Table 1. Number and Percent Distribution of Registered Deaths by Province, Ilocos Region: January 2020 and January 2019 Number of Registered Percentage Region/ Deaths Province January January January January 2020 2019 2020 2019 Ilocos Region 3,796 3,752 100 100 Ilocos Norte 499 474 13 13 Ilocos Sur 498 441 13 12 La Union 665 627 18 17 Pangasinan 2,134 2,210 56 59 Source: Preliminary results from the Decentralized Vital Statistics System Registered deaths in the region surpassed three thousand in January 2020 • Ilocos Region registered a total of 3,796 deaths in January 2020. • Pangasinan topped the highest number of deaths in January 2020. Its share was more than half (56 percent) of the total registered deaths in the region at 2,134 deaths. • La Union ranked second with 665 deaths (18 percent). • Ilocos Norte and Ilocos Sur followed with 499 deaths (13 percent) and 498 (13 percent), respectively. Parammata Bldg. C, Diversion Road, Sitio 5, Brgy. Biday, City of San Fernando, La Union Telefax: (072) 888-4804 / 607-0247/ 888-2582 www.rsso01.psa.gov.ph Dagupan City tops with the most registered number of deaths • Among cities/municipalities in the region, Dagupan City, Pangasinan registered the highest number of deaths with 443 deaths in January 2020.