Timeline of SARS-Cov2 Spread in Italy: Results from an Independent Serological Retesting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Environmental Suppliers Customer and Citizens Institutions and Communities Susainability Report - 2012 1 Index
Sustainability Report 2012 employees shareholders and investors environmental suppliers customer and citizens institutions and communities Susainability report - 2012 1 Index Index Letter to stakeholders 4 Introduction and note on methodology 6 The A2A Group’s Sustainability Report 6 Methodology 6 Scoping logic 7 Materiality 9 1 The A2A group 10 1.1 Size of the organisation and markets served 14 1.2 Companies outside the consolidation scope 15 2 Strategies and policies for sustainability 17 2.1 Mission and vision 18 2.2 Commitments and objectives for the future 18 2.3 The 2013-2015 Sustainability Plan and key indicators/results achieved in 2012 19 2.4 Partnerships and awards for sustainability 25 2.5 Corporate governance 27 Corporate governance bodies 27 Corporate governance tools 34 Regulatory framework 35 2.6 Stakeholder chart and engagement initiatives 37 3 Economic responsibility 41 3.1 The Group’s 2012 results 43 3.2 Formation of Value Added 43 3.3 Distribution of Net Global Value Added 45 3.4 Capital expenditure 46 3.5 Shareholders and Investors 47 Composition of share capital 47 A2A in the stock exchange indices 48 A2A in the sustainability ratings 49 2 Susainability report - 2012 Index Investing in A2A: sustainability as a valuation project 49 Relations with shareholders and investors 52 3.6 Tables: the numbers of the A2A Group 55 4 Environmental responsibility 57 4.1 Managing the environment 58 Environmental policy 59 Environmental management system 59 Environmental risk management 60 Environmental accounting 61 Research and -

New Milan Fair Complex
NEW MILAN FAIR COMPLEX Milan, Italy Development Team The New Milan Fair Complex (Nuovo Sistema Fiera Milano) has transformed a brownfield site along the Owner/Developer main road from downtown Milan to Malpensa Airport into a 200-hectare (494 ac) exhibition center, re- lieving traffic congestion around the historic fairground in the city center and allowing the original fair- Fondazione Fiera Milano Milan, Italy ground to continue to host smaller congresses and trade shows, even after part of the downtown site is www.fondazionefieramilano.com sold and redeveloped. The two separate yet complementary developments—the new complex at Rho- Pero (popularly known as Fieramilano) and the downtown complex (known as Fieramilanocity)—have Architect brought new life and prestige to Milan’s exhibition industry, enabling the Milan Fair Complex to con- Massimiliano Fuksas architetto tinue competing with other European exhibition centers and to maintain its position as an international Rome, Italy leader. Both projects are being promoted by Fondazione Fiera Milano, the private company that owns www.fuksas.it and operates the Milan Fair Complex, through its subsidiary Sviluppo Sistema Fiera SpA. Associate Architects The site of the new complex at Rho-Pero, two adjoining industrial suburbs northwest of Milan, was Schlaich Bergermann und Partner long occupied by an Agip oil refinery. After Fondazione Fiera Milano purchased the site, the refinery was Stuttgart, Germany dismantled and the land and groundwater cleaned up. In an approach considered highly unusual and www.sbp.de innovative in Italy, the foundation issued an international request for proposals (RFP) to select a general Studio Altieri contractor, an approach that lent continuity and consistency to the design and construction stages and Thiene (VI), Italy resulted in more accurate cost estimates and quicker completion. -

Milan, Italy Faculty Led Learning Abroad Program Fashion and Design Retailing: the Italian Way Led By: Dr
Milan, Italy Faculty Led Learning Abroad Program Fashion and Design Retailing: The Italian Way Led by: Dr. Chiara Colombi & Dr. Marcella Norwood What: 10-Day Study Tour: Milan, Italy (including Florence, Italy) When: Dates: May 22 – 31, 2016 (Between spring and summer terms 2016) Academic Plan: 1. Participate in preparation series during spring 2016 2. Travel & tour 3. Complete written assignments Enrollment: Enroll in HDCS 4398 or GRET 6398 (summer mini session) GPA Requirement: 2.5 (undergraduates); 3.0 (graduates) Scholarships: UH International Education Fee Scholarships 1. $750 (see http://www.uh.edu/learningabroad/scholarships/uh- scholarships/ for eligibility and application details. (graduate students already receiving GTF not eligible for scholarship) Deadline: IEF scholarship applications open January 4, close March 4. http://www.uh.edu/learningabroad/scholarships/uh-scholarships/) 2. $250 tuition rebate for HDCS 4398 (see http://www.uh.edu/learningabroad/scholarships/uh-scholarships/) (not available for GRET 6398 enrollment) To Apply: For Study Tour: To go into the registration, please click on this link (www.worldstridescapstone.org/register ) and you will be taken to the main registration web page. You will then be prompted to enter the University of Houston’s Trip ID: 129687 . Once you enter the Trip ID and requested security characters, click on the ‘Register Now’ box below and you will be taken directly to the site . Review the summary page and click ‘Register’ in the top right corner to enter your information 1 . Note: You are required to accept WorldStrides Capstone programs terms and conditions and click “check-out” before your registration is complete. -

Milan's New Exhibition System: a Driving Force Behind
COMUNICATO STAMPA MILAN’S NEW EXHIBITION SYSTEM: A DRIVING FORCE BEHIND THE ECONOMIC DEVELOPMENT OF LOMBARDY AND ITALY AS A WHOLE Monday, 17 November 2003 – Total revenues of more than €4.3 billion versus €2 billion in 2000, and 42,743 new jobs. This is the positive impact that Milan Fair will have on the regional economy when Milan’s new exhibition system, comprising the New Complex and the City Complex, will be operating at full capacity. Above, are some of the findings of a study conducted by Fondazione Fiera Milano – Ufficio Studi - in concert with CERTeT of Bocconi University, that will be presented on Friday, 14 November at the Milan conference of the “East-West Lombardy – the cardinal points of development” roadshow. The New Complex – the first stone of which was laid on 6 October 2002 – is a project that is being fully self-funded by Fondazione Fiera Milano and involves an investment of approx. €750 million, which includes the cost of purchasing the sites. The New Complex will have a gross floorspace of 530,000 square meters on a 2-million square meter site. A major project that is being developed by a private entity – Fondazione Fiera Milano – but with positive fallout for the public, the construction of which will generate €835 million in revenues and 7,900 new jobs. Noteworthy are also the figures related to the redevelopment project associated with the New Complex, with approx. 4.5 million cubic meters of reclaimed land. The study also shows that housing values in the municipalities around the New Complex rose - during 2000/2003 - by 25 percent versus 14.5 percent of comparable areas in the first city belt. -

Timeline / 1890 to 1900 / ITALY
Timeline / 1890 to 1900 / ITALY Date Country Theme 1890 - 1899 Italy Migrations Average annual Italian migration (temporary and permanent, to nearest 1,000): France 26,000, USA 51,000; Argentina 37,000; Brazil 58,000. 1890 Italy Music, Literature, Dance And Fashion The Cavalleria rusticana by Pietro Mascagni (1863–1945) has a great success, marking the beginning of verismo (Italian realism) in music, which intends to portray the world of peasants and the poor through strong and passionate drama. The singing style changes radically, leaving behind the aesthetics of bel canto and turning to reciting, even shouting, and spoken parts in the most exciting dramatic moments. 1890 Italy Reforms And Social Changes For the first time, trade unions organise celebrations for May Day as the International Worker’s Day. 1891 Italy Reforms And Social Changes First Chambers of Labour (territorial trade unions) founded in Milan. 1892 Italy Political Context Italian Socialist Party founded. 1892 - 1898 Italy Great Inventions Of The 19th Century Hydroelectric power plants are built in Tivoli (1892) and Paderno d’Adda (1898) and the power they generated is transported to, respectively, Rome and Milan. 1893 - 1895 Italy Cities And Urban Spaces Construction of Piazza Vittorio Emanuele (today Piazza della Repubblica) in Florence, after clearing the area of the Ancient Market. 1893 - 1894 Italy Economy And Trade A comprehensive law on banking establishes the Bank of Italy, which starts operating on 1 January 1894. 1893 Italy Music, Literature, Dance And Fashion Manon Lescaut by Giacomo Puccini (1858–1924) has a great success in Turin and Puccini becomes the most promising opera composer of the new generation. -

Rome Milan Sokol Ft
April 2021 Quarterly Publication AMERICAN SOKOL TYRS Honor Award Presented to Rome Milan Sokol Ft. Worth For Leadership in the Sport of Gymnastics And Selfless Dedication to Sokol In the True Spirit of its Founder Miroslav Tyrs The Falcon is the fastest bird of flight at 200 miles per hour and vision 2.5 times greater than humans. Fly you Sokol, fly on high! 1 Board of Governors The Sokol Eye – Sokolským Okem President Jean Hruby March/April 2021 Districts: Jean Hruby – President Central Rich Vachata A true legacy of Sokol, gymnastic pioneer, champion, innovator, mentor, Eastern Irene Wynnyczuk trendsetter…these are the qualities of the American Sokol Hall of Fame Dr. Northeastern Meg Novacek Miroslav Tyrš Honor Award. Pacific Yvonne Masopust This month the Southern District honored Brother Rome Milan with this notable Southern Robert Podhrasky award. When Rome Milan established the American Sokol Hall of Fame Awards, Western Allison Gerber he had a vision to remember those who have made a mark and changed the history of Sokol in a positive way. Unaware, Rome was actually writing his own history. Executive Board Members Together on “Zoom” many Sokols from around the USA joined the Southern President Jean Hruby District to witness Rome receiving this prestigious award. Listening to all of Rome’s accomplishments, memories and the words of gratitude shared by many 1st VP Robert Podhrasky who joined, reminded this “Sokol Eye” that we have remarkable people in our 2nd VP Maryann Fiordelis family and that if we strive to be like Rome Milan, Sokol will carry on. -

For an Urban History of Milan, Italy: the Role Of
FOR AN URBAN HISTORY OF MILAN, ITALY: THE ROLE OF GISCIENCE DISSERTATION Presented to the Graduate Council of Texas State University‐San Marcos in Partial Fulfillment of the Requirements for the Degree Doctor of PHILOSOPHY by Michele Tucci, B.S., M.S. San Marcos, Texas May 2011 FOR AN URBAN HISTORY OF MILAN, ITALY: THE ROLE OF GISCIENCE Committee Members Approved: ________________________________ Alberto Giordano ________________________________ Sven Fuhrmann ________________________________ Yongmei Lu ________________________________ Rocco W. Ronza Approved: ______________________________________ J. Micheal Willoughby Dean of the Gradute Collage COPYRIGHT by Michele Tucci 2011 ACKNOWLEDGEMENTS My sincere thanks go to all those people who spent their time and effort to help me complete my studies. My dissertation committee at Texas State University‐San Marcos: Dr. Yongmei Lu who, as a professor first and as a researcher in a project we worked together then, improved and stimulated my knowledge and understanding of quantitative analysis; Dr. Sven Fuhrmann who, in many occasions, transmitted me his passion about cartography, computer cartography and geovisualization; Dr. Rocco W. Ronza who provided keen insight into my topic and valuable suggestions about historical literature; and especially Dr. Alberto Giordano, my dissertation advisor, who, with patience and determination, walked me through this process and taught me the real essence of conducting scientific research. Additional thanks are extended to several members of the stuff at the Geography Department at Texas State University‐San Marcos: Allison Glass‐Smith, Angelika Wahl and Pat Hell‐Jones whose precious suggestions and help in solving bureaucratic issues was fundamental to complete the program. My office mates Matthew Connolly and Christi Townsend for their cathartic function in listening and sharing both good thought and sometimes frustrations of being a doctoral student. -

How SARS-Cov-2 Pandemic Changed Traumatology and Hospital Setting: an Analysis of 498 Fractured Patients
Journal of Clinical Medicine Article How SARS-CoV-2 Pandemic Changed Traumatology and Hospital Setting: An Analysis of 498 Fractured Patients Marco Brayda-Bruno 1, Riccardo Giorgino 2,* , Enrico Gallazzi 3, Ilaria Morelli 4 , Francesca Manfroni 1 , Matteo Briguglio 1 , Riccardo Accetta 1, Laura Mangiavini 1,5 and Giuseppe Maria Peretti 1,5 1 IRCCS Orthopedic Institute Galeazzi, 20144 Milan, Italy; [email protected] (M.B.-B.); [email protected] (F.M.); [email protected] (M.B.); [email protected] (R.A.); [email protected] (L.M.); [email protected] (G.M.P.) 2 Residency Program in Orthopedics and Traumatology, University of Milan, 20122 Milan, Italy 3 Ortopedia e Traumatologia 3, ASST Centro Specialistico Ortopedico Traumatologico G. Pini–CTO, 20122 Milan, Italy; [email protected] 4 U.O.C. Ortopedia e Traumatologia Nuovo Ospedale di Legnano ASST Ovest Milanese, 20025 Legnano, Italy; [email protected] 5 Department of Biomedical Sciences for Health, University of Milan, 20122 Milan, Italy * Correspondence: [email protected] Abstract: Background: SARS-CoV-2 pandemic is one of the biggest challenges for many health systems in the world, making lots of them overwhelmed by the enormous pressure to manage patients. We reported our Institutional Experience, with specific aims to describe the distribution and type of treated injuries, and the organizational setup of our hospital. Methods: Data of fractured patients admitted for surgical treatment in the time frames 9 March 2020–4 May 2020 and 1 March Citation: Brayda-Bruno, M.; 2019–31 May 2019 were collected and compared. Furthermore, surgery duration and some parameters Giorgino, R.; Gallazzi, E.; Morelli, I.; of effectiveness in health management were compared. -

Usa Pavilion Final Report
USA PAVILION FINAL REPORT THIS REPORT IS DEDICATED to the entire team at the U.S. Consulate Milan, Consul General, Ambassador Philip T. Reeker, and Deputy Commissioner General’s Commissioner General Elia Tello. The entire staff at the consulate in Milan was a critical element in the success of our efforts at the Milan Expo. They demonstrated the best of what the Department of State has to offer. USA PAVILION In addition to the team in Milan, we could not have done what we did and how we did it without Department support in Washington, D.C. We were blessed to have Ambassador David Thorne, Beatrice Camp, and Kelsey Bacon, examples of the world-class professionals who FINAL REPORT serve our country. …Welcome to the future we are working to create. June 8, 2016 were welcomed to our pavilion by President Obama, who outlined the One of the most beautiful elements of the pavilion was the vertical farm. Every day, I can meet people coming from all over the world and talk Dear Secretary Kerry, importance of food security and encouraged us each to play a role in While it was visually stunning, the vertical farm also represented what about sustainability on topics which are affecting all of us.” helping to solve these challenges. innovation can result when we combine the miracle of nature and the s the process of transforming the Expo site into an innovation The remarkable success and impact of the USA Pavilion could not have power of technology. The vertical farm was larger than an American hub for Milan gets underway, I wanted to take this opportunity President Obama noted, “By the year 2050 the world’s population is been possible without the direct efforts of you, Mr. -
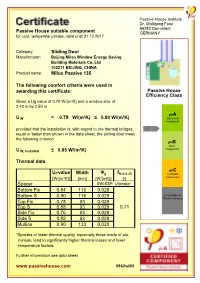
Passive House Suitable Component Sliding Door Milux Passive 135 The
Passive House Institute Dr. Wolfgang Feist 64283 Darmstadt Passive House suitable component GERMANY for cool, temperate climate, valid until 31.12.2017 Category: Sliding Door Manufacturer: Beijing Milan Window Energy Saving Building Materials Co.,Ltd 102211 BEIJING, CHINA Product name: Milux Passive 135 The following comfort criteria were used in awarding this certificate: Passive House Efficiency Class Given a Ug value of 0.70 W/(m²K) and a window size of 2.40 m by 2.50 m phA U W = 0.79 W/(m²K) ≤ 0.80 W/(m²K) advanced component provided that the installation is, with regard to the thermal bridges, equal or better than shown in the data sheet, the sliding door meets the following criterion. phB basic component U W, installed ≤ 0.85 W/(m²K) Thermal data phC Uf-value Width Ψg fRsi=0.25 certifiable [W/(m²K)] [mm] [W/(mK)] [-] component Spacer SWISSP. Ultimate* Bottom Fix 0.84 116 0.028 Bottom S 0.90 116 0.028 not suitable for Passive Houses Top Fix 0.78 93 0.029 Top S 0.88 93 0.029 0.71 Side Fix 0.76 93 0.028 Side S 0.82 93 0.028 Mullion 0.90 133 0.028 *Spacers of lower thermal quality, especially those made of alu- minium, lead to significantly higher thermal losses and lower temperature factors. Further information see data sheet www.passivehouse.com 0962sd03 Data Sheet Beijing Milan Window Energy Saving , Milux Passive 135 Manufacturer Beijing Milan Window Energy Saving Building Materials Co.,Ltd baishan lndustrial Park Changping Distrct, 102211 BEIJING, CHINA Tel.: +861080726999 E-Mail: [email protected], www.milanwindows.com o 20 C o 18 C o 16 C o 14 C o 12 C o 10 C o 8 C o 6 C o 4 C o 2 C o 0 C o -2 C o -4 C o -6 C o -8 C o -10 C Bottom section Isothermal Description Timber frame ( 0.13W/(mK)) with external aluminium shall and insulation PU (0.036W/(mK)). -

6-Day Rome, Florence, Maranello & Milan Ferrari Tour
ITALIA IN FERRARI powered by 6-Day Rome, Florence, Maranello & Milan Ferrari Tour A New Travel Concept Red Travel offers a new travel concept; an innovative approach to the self-drive tour offering absolute luxury combined with the ultimate Gran Turismo experience. Red Travel Tours are unique journeys, individually created for you to fully experience the Italian Way of Life. Each journey is a sublime blend of art, fashion, architecture, gastronomy and spectacular scenery. Our guests will feel part of a real Ferrari team, enjoying the opportunity to personally drive the very latest models. Travelling for kilometres, accelerating through the steep, winding roads of Lazio, Tuscany, Emilia-Romagna and Lombardia, putting their driving skills to the ultimate test. Behind the scenes, Red Travel staff take complete care of the Ferraris. Every morning, our guests will find their car at the entrance of the hotel, clean and polished, refuelled and fully checked, ready to begin another day of exciting driving through further dazzling landscapes. 6-Day Rome, Florence, Maranello & Milan Ferrari Tour 6-Day Rome, Florence, Maranello & Milan Ferrari Tour DAY 1: WELCOME TO ROME, THE ETERNAL CITY You will be met at Rome Fiumicino International Airport and transferred by Mercedes E-Class to· the splendid Hotel de la Ville, a modern-day icon atop the Spanish Steps. A lively 18th-century palazzo in a peerless position, Hotel de la Ville both embodies and overlooks life in the Eternal City’. The confluence of classical Roman romance and contemporary cool, sweeping city views, buzzing drinking and dining spots and fresh, zestful design make for Rome’s most exciting new arrival. -

EXPO2015. We Are There! Sustainable Farm Pavilion
THE WORLD OF NEW HOLLAND AGRICULTURE We are fi nally there. Until October 31st EXPO2015. the New Holland Sustainable Farm Pavilion We are there! at Expo 2015 displays our sustainable farming technologies. Sustainable Farm Pavilion EXPO2015. We are there! We are fi nally there. The New Holland Sustainable Farm Pavilion, at Expo 2015, will display our sustainable farming technologies until October 31st he New Holland Sustainable Farm Pavilion opened hours to which all farmers are accustomed. on May 1st ready to welcome over 20 million New Holland Agriculture is the only The Seeds of Life series is an important part of the Tvisitors who are expected to visit Milan for Expo experience within the Pavilion, as many visitors have little 2015, the Universal Exhibition. New Holland is a Global agricultural equipment manufacturer knowledge and awareness of agriculture. New Holland Partner of Expo Milano 2015and the only agricultural with its own pavilion participating in has made the visit to the Sustainable Farm Pavilion an equipment brand present at Expo 2015 as part of CNH the universal exhibition, whose theme enlightening experience. Industrial and Fiat Chrysler. The choice could not be The Pavilion itself is totally sustainable. Built without better given the Expo 2015 theme: Feeding the Planet, Feeding the Planet, Energy for Life concrete foundations, it is assembled on a steel framework Energy for Life. New Holland has actively pursued a perfectly represents the vision, the designed to be easily dismantled: no demolition work strategy for sustainable agriculture since 2006, when its mission and the values of our Clean will be needed nor any construction waste produced.