The Lardaceous Ochre – Hibernoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Who, How and What of Pathology of Soft Tissue Sarcoma
Editorial Page 1 of 11 Who, how and what of pathology of soft tissue sarcoma Salvatore Lorenzo Renne Anatomic Pathology Unit, Humanitas Research Hospital, Humanitas University, Rozzano, MI 20089, Italy Correspondence to: Salvatore Lorenzo Renne. Adjunct Teaching Professor, Anatomic Pathology Unit, Humanitas Research Hospital, Humanitas University, Via Manzoni 56, Rozzano, MI 20089, Italy. Email: [email protected]. Submitted Aug 06, 2018. Accepted for publication Aug 23, 2018. doi: 10.21037/cco.2018.10.09 View this article at: http://dx.doi.org/10.21037/cco.2018.10.09 Introduction to soft tissue sarcoma (STS) adipocytes (lipoma, spindle cells lipoma, hibernoma, well- pathology differentiated liposarcoma (LPS), myxoid LPS, etc.). One chapter is dedicated to specific entities “of uncertain STS is a generic term that refers to a heterogeneous group differentiation” that are well-characterized entities that do of rare neoplastic diseases. The aim of this review is to not readily resemble any normal mesenchymal cells (as the discuss the role of pathology in the multidisciplinary Ewing sarcoma or the synovial sarcoma—a clear misnomer). management of STS patients. This will be done: (I) The last chapter is dedicated to those sarcomas that do illustrating the framework for the current classification; (II) not follow in any of the previously listed diagnosis and are examining the characteristics that allows an expert diagnosis; therefore called “undifferentiated/unclassified sarcomas” (III) describing the role of the sarcoma pathologist -

Complete Case of a Rare but Benign Soft Tissue Tumor
Hindawi Case Reports in Orthopedics Volume 2019, Article ID 6840693, 5 pages https://doi.org/10.1155/2019/6840693 Case Report Hibernoma of the Upper Extremity: Complete Case of a Rare but Benign Soft Tissue Tumor Thomas Reichel ,1 Kilian Rueckl,1 Annabel Fenwick,1,2 Niklas Vogt,3 Maximilian Rudert,1 and Piet Plumhoff1 1Department of Orthopedic Surgery, Koenig-Ludwig-Haus, University of Wuerzburg, Brettreichstraße 11, 97074 Wuerzburg, Germany 2Department of Trauma Surgery, Klinikum Augsburg, 86156 Augsburg, Germany 3Department of Pathology, University of Wuerzburg, 97080 Wuerzburg, Germany Correspondence should be addressed to Thomas Reichel; [email protected] Received 26 February 2019; Accepted 14 April 2019; Published 21 May 2019 Academic Editor: Elke R. Ahlmann Copyright © 2019 Thomas Reichel et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Hibernoma is a rare benign lipomatous tumor showing differentiation of brown fatty tissue. To the author’s best knowledge, there is no known case of malignant transformation or metastasis. Due to their slow, noninfiltrating growth hibernomas are often an incidental finding in the third or fourth decade of life. The vast majority are located in the thigh, neck, and periscapular region. A diagnostic workup includes ultrasound and contrast-enhanced MRI. Differential diagnosis is benign lipoma, well- differentiated liposarcoma, and rhabdomyoma. An incisional biopsy followed by marginal resection of the tumor is the standard of care, and recurrence after complete resection is not reported. The current paper presents diagnostic and intraoperative findings of a hibernoma of the upper arm and reviews similar reports in the current literature. -

The Use of High Tumescent Power Assisted Liposuction in the Treatment of Madelung’S Collar
Letter to the Editor The use of high tumescent power assisted liposuction in the treatment of Madelung’s collar Henryk Witmanowski1,2, Łukasz Banasiak1, Grzegorz Kierzynka1, Jarosław Markowicz1, Jerzy Kolasiński1, Katarzyna Błochowiak3, Paweł Szychta1,4 1Department of Plastic, Reconstructive and Aesthetic Surgery, Medical College in Bydgoszcz, Nicolaus Copernicus University in Torun, Poland 2Department of Physiology, Poznan University of Medical Sciences, Poznan, Poland 3Department of the Oral Surgery, Poznan University of Medical Sciences, Poznan, Poland 4Department of Oncological Surgery and Breast Diseases, Polish Mother’s Memorial Hospital-Research Institute, Lodz, Poland Adv Dermatol Allergol 2017; XXXIV (4): 366–371 DOI: https://doi.org/10.5114/ada.2017.69319 Mild symmetrical lipomatosis (plural symmetrical The disease most commonly takes a proximal form lipomatosis, multiple symmetric lipomatosis – MSL), which takes the following areas of the body with the fol- also known as Madelung’s disease or Launois-Bensaude lowing frequency: the genial area 92.3%, cervical region syndrome is a rare disease of unknown etiology, first de- 67.7%, shoulder region 54.8%, abdominal 45.2%, chest scribed by Brodie in 1846, Madelung in 1888, and Launois 41.9%, thigh and pelvic rim 32.3% [11, 12]. The periph- with Bensaude in 1898 [1–3]. eral type mainly locates on both sides at the level of the Madelung’s disease incidence is 1 : 250000 [4]. Mul- hands, feet and knees, this is definitely a rarer form of tiple symmetric lipomatosis occurs mainly in the inhabit- the disease. The mixed form is described very rarely. The ants of the Mediterranean area and Eastern Europe, in specified central type is also engaged primarily around males (male to female ratio is 20 : 1), aged 30–70 years, the lower torso, and intermediate parts of the legs. -
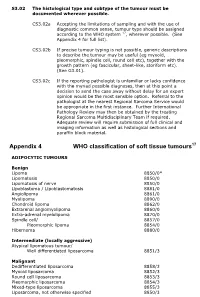
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -
The Role of Cytogenetics and Molecular Diagnostics in the Diagnosis of Soft-Tissue Tumors Julia a Bridge
Modern Pathology (2014) 27, S80–S97 S80 & 2014 USCAP, Inc All rights reserved 0893-3952/14 $32.00 The role of cytogenetics and molecular diagnostics in the diagnosis of soft-tissue tumors Julia A Bridge Department of Pathology and Microbiology, University of Nebraska Medical Center, Omaha, NE, USA Soft-tissue sarcomas are rare, comprising o1% of all cancer diagnoses. Yet the diversity of histological subtypes is impressive with 4100 benign and malignant soft-tissue tumor entities defined. Not infrequently, these neoplasms exhibit overlapping clinicopathologic features posing significant challenges in rendering a definitive diagnosis and optimal therapy. Advances in cytogenetic and molecular science have led to the discovery of genetic events in soft- tissue tumors that have not only enriched our understanding of the underlying biology of these neoplasms but have also proven to be powerful diagnostic adjuncts and/or indicators of molecular targeted therapy. In particular, many soft-tissue tumors are characterized by recurrent chromosomal rearrangements that produce specific gene fusions. For pathologists, identification of these fusions as well as other characteristic mutational alterations aids in precise subclassification. This review will address known recurrent or tumor-specific genetic events in soft-tissue tumors and discuss the molecular approaches commonly used in clinical practice to identify them. Emphasis is placed on the role of molecular pathology in the management of soft-tissue tumors. Familiarity with these genetic events -

The 2020 WHO Classification of Soft Tissue Tumours: News and Perspectives
PATHOLOGICA 2021;113:70-84; DOI: 10.32074/1591-951X-213 Review The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives Marta Sbaraglia1, Elena Bellan1, Angelo P. Dei Tos1,2 1 Department of Pathology, Azienda Ospedale Università Padova, Padova, Italy; 2 Department of Medicine, University of Padua School of Medicine, Padua, Italy Summary Mesenchymal tumours represent one of the most challenging field of diagnostic pathol- ogy and refinement of classification schemes plays a key role in improving the quality of pathologic diagnosis and, as a consequence, of therapeutic options. The recent publica- tion of the new WHO classification of Soft Tissue Tumours and Bone represents a major step toward improved standardization of diagnosis. Importantly, the 2020 WHO classi- fication has been opened to expert clinicians that have further contributed to underline the key value of pathologic diagnosis as a rationale for proper treatment. Several rel- evant advances have been introduced. In the attempt to improve the prediction of clinical behaviour of solitary fibrous tumour, a risk assessment scheme has been implemented. NTRK-rearranged soft tissue tumours are now listed as an “emerging entity” also in con- sideration of the recent therapeutic developments in terms of NTRK inhibition. This deci- sion has been source of a passionate debate regarding the definition of “tumour entity” as well as the consequences of a “pathology agnostic” approach to precision oncology. In consideration of their distinct clinicopathologic features, undifferentiated round cell sarcomas are now kept separate from Ewing sarcoma and subclassified, according to the underlying gene rearrangements, into three main subgroups (CIC, BCLR and not Received: October 14, 2020 ETS fused sarcomas) Importantly, In order to avoid potential confusion, tumour entities Accepted: October 19, 2020 such as gastrointestinal stroma tumours are addressed homogenously across the dif- Published online: November 3, 2020 ferent WHO fascicles. -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -

Case Report Perineal Lipoblastoma: a Case Report and Review of Literature
Int J Clin Exp Pathol 2014;7(6):3370-3374 www.ijcep.com /ISSN:1936-2625/IJCEP0000325 Case Report Perineal lipoblastoma: a case report and review of literature Qiang Liu1*, Zheng Xu1*, Shunbao Mao1, Rongyao Zeng1, Wenyou Chen1, Qiang Lu1, Yihe Guo2, Jing Liu1* 1Department of General Surgery, 175 Hospital of PLA (Affiliated Dongnan Hospital of Xiamen University), 269 Zhanghua Middle Road, Zhangzhou 363000, Fujian Province, China; 2Department of Pathology, 175 Hospital of PLA, 269 Zhanghua Middle Road, Zhangzhou 363000, Fujian Province, China. *Equal contributors. Received March 25, 2014; Accepted May 23, 2014; Epub May 15, 2014; Published June 1, 2014 Abstract: Lipoblastoma is a rare benign mesenchymal tumor that composes of embryonal white fat tissue and typi- cally occurs in infants or young children under 3 years of age. It usually affects the extremities, trunk, head, and neck. The perineum is a rare location with only 7 cases reported in the literature. We describe a case of 3-year-old girl with a lipoblastoma arising from perineum. An approximately 4.5 cm × 3.5 cm × 2.5 cm nodule was resected in left perineum with satisfied results. Pathological examination showed that it was composed of small lobules of mature and immature fat cells, separated by fibrous septa containing small dilated blood vessels. The left perineal lipoblastoma, although rare, should be differentiated from some other mesenchymal tumors with similar histologic and cytological features. Keywords: Perineum, lipoblastoma, myxoid liposarcoma, childhood, pathology Introduction Case report Lipoblastoma was first described by Jaffe in A 3-year-old girl was admitted to the Department 1926 [1]. -

Cellular Angiofibroma: Analysis of 25 Cases Emphasizing Its Relationship to Spindle Cell Lipoma and Mammary-Type Myofibroblastoma
Modern Pathology (2011) 24, 82–89 82 & 2011 USCAP, Inc. All rights reserved 0893-3952/11 $32.00 Cellular angiofibroma: analysis of 25 cases emphasizing its relationship to spindle cell lipoma and mammary-type myofibroblastoma Uta Flucke1, J Han JM van Krieken1 and Thomas Mentzel2 1Department of Pathology, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands and 2Dermatopathologie Bodensee, Friedrichshafen, Germany Cellular angiofibroma represents a rare benign mesenchymal tumor, occurring mainly in the superficial soft tissue of the genital region. The involvement of 13q14 in some cases confirmed the morphological suggested link with spindle cell lipoma and mammary-type myofibroblastoma. We analyzed the clinicopathological and immunohistochemical features of 25 cases, and performed in a number of cases additional molecular studies. There were 17 female and 8 male patients (age ranged from 27 to 83 years); females tended to be younger. A marked predilection for the vulva (n ¼ 13) was observed, and neoplasms in males were predominantly located in the inguinal region (n ¼ 4), and one case each in the scrotum, perianal, the knee, and the upper eyelid. The tumors arose most commonly in the superficial soft tissue and were well circumscribed in all but two cases. The tumor size ranged from 1 to 9 cm. All lesions were composed of spindle-shaped cells associated with numerous small- to medium-sized blood vessels; however, a broad morphological variation with foci of lipogenic differentiation in nine cases and sarcomatous transformation in one case was found. By immunohistochemistry, 11 out of 22 cases expressed CD34. A focal reaction for a-smooth muscle actin was observed in 9 out of 22 cases, and two cases each stained weak and focally positive for epithelial membrane antigen and CD99. -

Cd34positive Superficial Myxofibrosarcoma
J Cutan Pathol 2013: 40: 639–645 © 2013 John Wiley & Sons A/S. doi: 10.1111/cup.12158 Published by John Wiley & Sons Ltd John Wiley & Sons. Printed in Singapore Journal of Cutaneous Pathology CD34-positive superficial myxofibrosarcoma: a potential diagnostic pitfall§ Background: Myxofibrosarcoma (MFS) arises most commonly in the Steven C. Smith1,†,AnnA. proximal extremities of the elderly, where it may involve subcutaneous Poznanski1,†,§, Douglas R. and dermal tissues and masquerade as benign entities in limited biopsy Fullen1,2, Linglei Ma3, samples. We encountered such a case, in which positivity for CD34 and Jonathan B. McHugh1,DavidR. morphologic features were initially wrongly interpreted as a Lucas1 and Rajiv M. Patel1,2 ‘low-fat/fat-free’ spindle cell/pleomorphic lipoma. Case series have not 1 assessed prevalence of CD34 reactivity among cutaneous examples of Department of Pathology, University of Michigan, Ann Arbor, MI, USA, MFS. 2Department of Dermatology, University of Methods: We performed a systematic review of our institution’s Michigan, Ann Arbor, MI, USA, and experience, selecting from among unequivocal MFS resection 3Miraca Life Sciences, Glen Burnie, MD, USA specimens those superficial cases in which a limited biopsy sample §This project was presented orally as a proffered might prove difficult to interpret. These cases were immunostained for paper at the United States and Canadian Academy CD34 and tabulated for clinicopathologic characteristics. of Pathology Annual Meeting in Baltimore, MD, = March 2013. Results: After review of all MFS diagnoses over 5 years (n 56), we †Both the authors contributed equally to this work. identified a study group of superficial MFS for comparison to the index ‡Present address: Department of Biomedical case (total n = 8). -
Molecular Diagnosis of Soft Tissue Tumors: Avoid Pitfalls
Molecular Diagnosis of Soft Tissue Tumors: Avoid Pitfalls Cristina Antonescu, MD Department of Pathology Memorial Sloan-Kettering Cancer Center, New York Overview I. When should we rely on the help of molecular testing? II. Specificity, Prevalence, and Prognostic Implications of Molecular Abnormalities. III. ‘Gold Standard’ in surgical pathology of soft tissue tumors I. When should we rely on the help of molecular testing? – difficult distinctions between a benign and malignant diagnosis – unusual morphologic features – unusual clinical presentations or unexpected immunohistochemical results – refined classification may directly impact on clinical management of the patient – confirm diagnosis in conflicting second opinions Benign vs Malignant STT – Perineurioma versus Low Grade Fibromyxoid Sarcoma – SFT/HPC versus Synovial Sarcoma (SS) – Angiomatoid Fibrous Histiocytoma vs sarcoma – Lipoblastoma vs myxoid liposarcoma in children Sarcomas with unusual morphologic appearance – Desmoplastic Round Cell Tumor (DRCT) with predominantly rosettes or tubular structure formation – Small cell GIST in children STT with typical morphology but unusual clinical presentation – Ewing Sarcoma in superficial location – Ewing Sarcoma in older individuals (>40 years) – Ewing Sarcoma in visceral location STT associated with an unusual immunoprofile – Ewing Sarcoma (ES) with strong Keratin expression – Synovial sarcoma with S100 protein positivity Refined classification may directly impact on clinical management – GIST versus sarcoma, NOS – Ewing Sarcoma vs -
Pattern-Based Approach to Mesenchymal Neoplasms and Their Mimics in the Head and Neck
PATTERN-BASED APPROACH TO MESENCHYMAL NEOPLASMS AND THEIR MIMICS IN THE HEAD AND NECK. Bibianna Purgina, MD FRCPC The Ottawa Hospital/EORLA, University of Ottawa, Ottawa, Canada Outline Important histologic patterns in H&N soft tissue lesions Hypercellular Spindle Cell Lesions Hemangiopericytoma-Like Vascular Pattern Lipomatous Tumors Myxoid Lesions Clues when dealing with overlapping features Chondroid tumors in bone Hemangiopericytoma- Hypercellular Spindle Like Vascular Pattern Cell Lesions Myxoid Lesions Lipomatous Tumors Hypercellular Spindle Hemangiopericytoma- Cell Lesions Like Vascular Pattern Spindle Cell SCC Angiofibroma Spindle Cell Melanoma Glomangiopericytoma Spindle Myoepithelioma/carcinoma Solitary Fibrous Tumor MPNST Myofibroma Cellular Schwannoma LM/LMS Biphenotypic Sinonasal Sarcoma Synovial Sarcoma Monophasic Synovial Sarcoma Spindle Cell/Sclerosing RMS Myxoid Lesions Lipomatous Tumors Nodular Fasciitis Low grade fibromyxoid sarcoma Typical Lipoma and lipoma Sinonasal Polyp variants Myxoma Spindle cell/pleomorphic lipoma Chondromyxoid Fibroma Liposarcoma Myxoid Odontogenic Tumors Nerve Sheath Tumours HPC-Like Vascular Pattern Hypercellular Spindle Cell LesionsGPC Spindle Cell SCC Myofibroma Angiofibroma Spindle Cell Melanoma LM/LMS Myofibroma Spindle Myoepithelioma/ BSNS Carcinoma Monophasic SS Spindle Cell/Sclerosing RMS Cellular Schwannoma MPNST SFT Fibromatosis Lipomatous Tumors Nodular Fasciitis Low grade fibromyxoid sarcoma Spindle cell/pleomorphic lipoma Neurofibroma, schwannoma Myxoid Lesions Typical Lipoma