Clinically Established Biodegradable Long Acting Injectables: an Industry Perspective
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
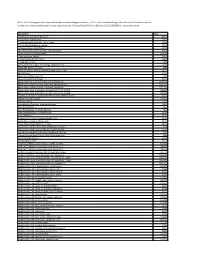
NOTE: the Following Are Shirley Ryan Abilitylab's Standard Charges As of Jan. 1, 2019. These Standard Charges Often Do Not
NOTE: The following are Shirley Ryan AbilityLab's standard charges as of Jan. 1, 2019. These standard charges often do not reflect what a patient or their insurance company/payer may be required to pay. Contact Patient Financial Services at 312-238-6039 for more information. Description Price 11-Deoxycortisol, Urine Random $531 12 Lead Ekg, Tracing Only $245 17 Hydroxycorticosteroids, Urine Timed $363 17 Hydroxyprogesterone, Serum $172 17 Ketosteroids, Urine Timed $273 17-Ketosteroids with Creatinine, Urine Random $273 2D Gait Analysis Charge(95999) $2,174 5' Nucleotidase, Serum $269 5.5 PDC PEDS CUFFED TRACH $226 5-HIAA-24 Hr Urine $99 A4566 Shoulder sling or vest design, abduction res $226 A4595 FES Electrode, each $38 A6545 Gradient Compression Wrap, Non-Elastic, Belo $171 ABO Rh Type $106 Above Knee Nylon Hose PR $83 Above Knee Suction Sheath $131 Above knee, for proximal femoral focal deficiency, $14,344 Above knee, molded socket, open end, SACH foot, en $10,751 Above knee, molded socket, single axis constant fr $10,935 Above knee, short prosthesis, no knee joint (""stu_L5210 $8,682 Above knee, short prosthesis, no knee joint (""stu_L5220 $7,429 ACAPELLA DH GREEN VIBRATORY PEP W/MOUTHPIECE DEVIC $181 Acetabuloplasty (27120) $4,493 Acetone, Serum $27 Acetylcholine Receptor Binding Antibody $405 Acid Phosphatase $66 Acid Phosphatase, Prostatic fraction $66 ACNE SURGERY MILIA CYSTS (10040) $530 Acorn Nebulizer $174 Activated PTT/Partial Thromboplastin Time $109 Active Wound Care > 20 cm Units $171 Active Wound Care/20 cm or < Units $171 Acupuncture with E-Stim. Each additional 15 minute $65 Acupuncture with E-Stim. -

Dexamethasone Sodium Phosphate Injection, USP)
HEXADROL® PHOSPHATE INJECTION (dexamethasone sodium phosphate injection, USP) DESCRIPTION — Hexadrol® Phosphate Injection (dexamethasone sodium phosphate injection, USP) is a water-soluble inorganic ester of dexamethasone which produces a rapid response even when injected intramuscularly. Dexamethasone Sodium Phosphate, C22H28FNa2O8P, has a molecular weight of 516.41 and chemically is Pregn-4-ene-3, 20-dione, 9-fluoro-11, 17-dihydroxy-16-methyl-21 (phosphonooxy)-, disodium salt, (11β, 16α). It occurs as a white to creamy white powder, is exceedingly hygroscopic, is soluble in water and its solutions have a pH between 7.5 and 10.5. It has the following structural formula: Hexadrol® Phosphate Injection is available in 4 mg/mL and 10 mg/mL concentrations. Each mL of Hexadrol® Phosphate Injection 4 mg/mL, contains dexamethasone sodium phosphate, USP equivalent to 4 mg dexamethasone phosphate; 1 mg sodium sulfite; 10 mg benzyl alcohol (preservative). Made isotonic with sodium citrate. pH adjusted with citric acid or sodium hydroxide. 1 Reference ID: 3593917 Each mL of Hexadrol® Phosphate Injection 10 mg/mL, contains dexamethasone sodium phosphate, USP equivalent to 10 mg dexamethasone phosphate; 1.5 mg sodium sulfite; 10 mg benzyl alcohol (preservative). Made isotonic with sodium citrate. pH adjusted with citric acid or sodium hydroxide. ACTIONS — Naturally occurring glucocorticoids (hydrocortisone), which also have salt- retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs are primarily used for their potent anti-inflammatory effects in disorders of many organ systems. Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body’s immune responses to diverse stimuli. -

Symptom Management in the Last Days of Life This Is About Managing Symptoms in the Last Days of Life Where the Dying Process Has Set In
Symptom management in the last days of life This is about managing symptoms in the last days of life where the dying process has set in. It assumes that the therapeutic aims are therefore: To allow the patient to die comfortably To support the family/carers and to start to prepare them for bereavement To discontinue any burdensome or irrelevant clinical procedures Key Prescribing Questions in the last days of life 1. Ahead of time Page a. Pre-emptive prescribing 1 b. Differences in specific circumstances 1 2. Once the oral route is lost a. What can be stopped? – managing co-morbidities at the end of life 2 (insulin; anti-epileptics; steroids; cardiac medicines) b. How to prescribe a syringe pump 3 i. Opioid conversion 4 ii. Combining drugs in a syringe – what can and can’t be mixed? 5 iii. Dosing other drugs 6 c. What can and can’t be given subcutaneously 7 3. Problems a. Uncontrolled symptoms (pain; restlessness; secretions; breathlessness; nausea; thirst) 8 b. Obtaining medicines out of hours 11 c. References and contact phone numbers 12 Pre-emptive prescribing The pre-emptive prescribing of p.r.n. medication for anticipated symptoms can avoid great distress. The cost is negligible and it saves time on the part of both families and out-of-hours health professionals. Typical maximum doses are described on page 22, but the doses needed by individuals vary widely: it is more important to assess the effectiveness of each p.r.n. before repeating or increasing doses – if a p.r.n. is ineffective, try a different approach or seek advice (see flow diagrams) A typical “pre-emptive p.r.n.” regimen for patients approaching the end of life might include: Morphine sulphate 2.5-5mg 1-4 hourly p.r.n. -

Vertebroplasty (Repair of Vertebrae with Bone Cement)
Patient information – Radiology Unit Tel 0118 322 7991 Vertebroplasty (repair of vertebrae with bone cement) Introduction This leaflet tells you about the procedure known as “vertebroplasty”, explains what is involved, the benefits and possible risks. It is not meant to replace informed discussion between you and your doctor but can act as a starting point for such a discussion. You should have plenty of time to discuss this procedure with the doctor who will be performing the procedure. What is vertebroplasty? Vertebroplasty is a procedure used to strengthen a collapsed spinal vertebra that has fractured and usually lost height due to osteoporosis or, less commonly, tumour infiltration or trauma. Vertebroplasty is primarily aimed at relieving the patient’s pain, to allow a rapid return to the previous level of activity, and secondarily to prevent further vertebral collapse. It is minimally invasive which means that patients suffer less disruption, face less risk and recover more quickly than with conventional open surgery. It is most effective when the fracture is relatively recent and particularly in patients who are very debilitated by the pain of the fracture or who cannot tolerate adequate quantities of painkilling medication. In some circumstances, vertebroplasty can be very effective even if the fracture is many months or even years old. Vertebroplasty is accomplished by injecting orthopaedic cement through a needle into the fractured bone; essentially forming an internal cast to stabilise the fracture similar to the principle of using plaster cast on an arm fracture. Typically, vertebroplasty is recommended if simpler treatments, such as bed rest, back bracing or pain medication have been ineffective, or if the side effects of analgesia have become problematic, such as causing stomach ulcers or drowsiness. -

Centre for Reviews and Dissemination
Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta- analysis Leucht S, Corves C, D Arbter, Engel R R, Li C, Davis J M CRD summary The authors concluded that amisulpride, clozapine, olanzapine and risperidone can be effective in treating schizophrenia patients. Second-generation antipsychotic drugs can also result in fewer extrapyramidal side effects, but can induce weight gain. The authors' conclusions reflected the evidence presented, but some potential methodological flaws in the review process meant that the extent to which those conclusions were reliable was unclear. Authors' objectives To compare the effects of first and second-generation antipsychotic drugs in schizophrenia patients. Searching The search for eligible studies was started in 2005, including MEDLINE to October 2006, Cochrane Schizophrenia Group's Specialised Register and the US Food and Drugs Administration website. Search terms were reported and there were no language restrictions. Previous reviews were searched for additional relevant studies. Study selection Randomised controlled trials (RCTs) of oral second-generation antipsychotic drugs (amisulpride, aripiprazole, clozapine, olanzapine, quetiapine, risperidone, sertindole, ziprasidone and zotepine) compared with first-generation drugs in patients with schizophrenia or related disorders (schizoaffective, schizophreniform or delusional disorders) irrespective of diagnostic criteria were eligible for inclusion in the review. The optimum doses of second-generation drugs were selected -

Oxford® Policy Update Bulletin: December 2015 Oxford
Oxford December 2015 policy update bulletin Medical & Administrative Policy Updates UnitedHealthcare respects the expertise of the physicians, health care professionals, and their staff who participate in our network. Our goal is to support you and your patients in making the most informed decisions regarding the choice of quality and cost-effective care, and to support practice staff with a simple and predictable administrative experience. The Policy Update Bulletin was developed to share important information regarding Oxford® Medical and Administrative Policy updates.* *Where information in this bulletin conflicts with applicable state and/or federal law, Oxford® follows such applicable federal and/or state law Oxford Oxford® Medical and Administrative Policy Updates Overview This bulletin provides complete details on Oxford® Medical and Policy Update Classifications Administrative Policy updates. The appearance of a service or New procedure in this bulletin indicates only that Oxford® has recently New clinical coverage criteria and/or documentation review requirements adopted a new policy and/or updated, revised, replaced or have been adopted for a service, procedure, test, or device retired an existing policy; it does not imply that Oxford® provides Updated coverage for the service or procedure. In the event of an An existing policy has been reviewed and changes have not been made inconsistency or conflict between the information provided in this to the clinical coverage criteria or documentation review requirements; bulletin and the posted policy, the provisions of the posted policy however, items such as the clinical evidence, FDA information, and/or will prevail. Note that most benefit plan documents exclude from list(s) of applicable codes may have been updated benefit coverage health services identified as investigational or unproven/not medically necessary. -

Future Directions for Intrathecal Pain Management 93
NEUROMODULATION: TECHNOLOGY AT THE NEURAL INTERFACE Volume 11 • Number 2 • 2008 http://www.blackwell-synergy.com/loi/ner ORIGINAL ARTICLE FBlackwell uturePublishing Inc Directions for Intrathecal Pain Management: A Review and Update From the Interdisciplinary Polyanalgesic Consensus Conference 2007 Timothy Deer, MD* • Elliot S. Krames, MD† • Samuel Hassenbusch, MD, PhD‡ • Allen Burton, MD§ • David Caraway, MD¶ • Stuart Dupen, MD** • James Eisenach, MD†† • Michael Erdek, MD‡‡ • Eric Grigsby, MD§§ • Phillip Kim, MD¶¶ • Robert Levy, MD, PhD*** • Gladstone McDowell, MD††† • Nagy Mekhail, MD‡‡‡ • Sunil Panchal, MD§§§ • Joshua Prager, MD¶¶¶ • Richard Rauck, MD**** • Michael Saulino, MD†††† •Todd Sitzman, MD‡‡‡‡ • Peter Staats, MD§§§§ • Michael Stanton-Hicks, MD¶¶¶¶ • Lisa Stearns, MD***** • K. Dean Willis, MD††††† • William Witt, MD‡‡‡‡‡ • Kenneth Follett, MD, PhD§§§§§ • Mark Huntoon, MD¶¶¶¶¶ • Leong Liem, MD****** • James Rathmell, MD†††††† • Mark Wallace, MD‡‡‡‡‡‡ • Eric Buchser, MD§§§§§§ • Michael Cousins, MD¶¶¶¶¶¶ • Ann Ver Donck, MD******* *Charleston, WV; †San Francisco, CA; ‡Houston, TX; §Houston, TX; ¶Huntington, WV; **Bellevue, WA; ††Winston Salem, NC; ‡‡Baltimore, MD; §§Napa, CA; ¶¶Wilmington, DE; ***Chicago, IL; †††Columbus, OH; ‡‡‡Cleveland, OH; §§§Tampa, FL; ¶¶¶Los Angeles, CA; ****Winston Salem, NC; ††††Elkings Park, PA; ‡‡‡‡Hattiesburg, MS; §§§§Colts Neck, NJ; ¶¶¶¶Cleveland, OH; *****Scottsdale, AZ; †††††Huntsville, AL; ‡‡‡‡‡Lexington, KY; §§§§§Iowa City, IA; ¶¶¶¶¶Rochester, NY; ******Nieuwegein, The Netherlands; ††††††Boston, MA; ‡‡‡‡‡‡La Jolla, CA; §§§§§§Switzerland; ¶¶¶¶¶¶Australia; and *******Brugge, Belgium ABSTRACT Background. Expert panels of physicians and nonphysicians, all expert in intrathecal (IT) therapies, convened in the years 2000 and 2003 to make recommendations for the rational use of IT analgesics, based on the preclinical and clinical literature known up to those times, presentations of the expert panels, discussions on current practice and standards, and the result of surveys of physicians using IT agents. -

2.0 Synopsis
Hydrocodone/Acetaminophen Extended Release Tablets M12-807 Abbreviated Clinical Study Report R&D/11/661 2.0 Synopsis Abbott Laboratories Individual Study Table Referring (For National Authority to Part of Dossier: Use Only) Name of Study Drug: Volume: Hydrocodone/Acetaminophen Extended Release Page: Name of Active Ingredient: Hydrocodone 10 mg/ Acetaminophen 650 mg Extended Release Title of Study: A Phase 2, Randomized Withdrawal Study of the Analgesic Efficacy and Safety of Hydrocodone/Acetaminophen Extended Release Compared to Placebo in Subjects with Chronic Low Back Pain Coordinating Investigator: Study Sites: Seventeen investigative sites in the United States Publications: None Studied Period (Years): Phase of Development: 2 First Subject First Visit: 22 June 2011 Last Subject Last Visit: 28 October 2011 Objectives: The primary objective of this study was to compare the analgesic efficacy and safety of 1 tablet of hydrocodone/acetaminophen extended release 10 mg/650 mg administered twice daily over 2 weeks to placebo in subjects with moderate to moderately severe chronic low back pain (CLBP). A secondary objective of this study was to explore the population pharmacokinetics of hydrocodone and acetaminophen resulting from administration of hydrocodone/acetaminophen extended release 10 mg/650 mg tablets. Methodology: This Phase 2, multicenter, double-blind (DB), placebo-controlled, randomized withdrawal study compared the analgesic efficacy and safety of 1 tablet hydrocodone/acetaminophen extended release 10 mg/650 mg to placebo in subjects with moderate to moderately severe CLBP. Subjects met pre-defined criteria at the conclusion of the Open-Label (OL) Titration Period to proceed to randomization into the DB Maintenance Period of the study. -

Hyoscine Butylbromide, Levomepromazine, Metoclopramide, Midazolam, Ondansetron
TRUST WIDE/DIVISIONAL DOCUMENT Delete as appropriate Policy/Standard Operating Procedure/ Clinical Guideline Policy and Procedure for the T34 Ambulatory Syringe Pump DOCUMENT TITLE: in adults (Palliative Care) DOCUMENT ELHT/CP22 Version 5.3 NUMBER: DOCUMENT REPLACES Which ELHT/CP22 Version 5.2 Version LEAD EXECUTIVE DIRECTOR DGM AUTHOR(S): Note Syringe pump policy task and finish group chaired by should not include Palliative Medicine Consultant names TARGET AUDIENCE: Medical and Nursing Staff 1 To provide a clear governance framework to ensure a safe and consistent approach to the use of the T34 Ambulatory Syringe Pump DOCUMENT 2 To provide details of how to set up and administer PURPOSE: medication by a T34 Ambulatory Syringe Pump 3 To provide easily accessible information about the common medicines used in a Syringe Pump Clinical Practice Summary. Guidance on consensus approaches To be read in to managing palliative care symptoms. Lancashire and South conjunction with Cumbria consensus guidance – August 2017 (identify which internal C064 V5 Medicines Management Policy documents) IC24 V4 Aseptic non touch technique (ANTT) policy East Lancashire Hospital NHS Trust – Policies & Procedures, Protocols, Guidelines ELHT/CP22 v5.2 May 2020 Page 1 of 77 Nursing and Midwifery Council - Standards for Medicines Management 2015 Dickman et al (2016) The Syringe Driver, 4th edition, Oxford Press T. Mitten, (2000) Subcutaneous drug infusions, a review of problems and solutions. International Journal of Palliative Nursing Vol 7, No 2. Twycross et al (2017) 6th Edition Palliative Care SUPPORTING Formulary and Palliative Care Formulary online, REFERENCES accessed June 2018 Twycross R., Wilcock A., (2001) Symptom Management in Advanced Cancer 3rd edition Radcliffe medical press Oxon. -

Approach to the Poisoned Patient
PED-1407 Chocolate to Crystal Methamphetamine to the Cinnamon Challenge - Emergency Approach to the Intoxicated Child BLS 08 / ALS 75 / 1.5 CEU Target Audience: All Pediatric and adolescent ingestions are common reasons for 911 dispatches and emergency department visits. With greater availability of medications and drugs, healthcare professionals need to stay sharp on current trends in medical toxicology. This lecture examines mind altering substances, initial prehospital approach to toxicology and stabilization for transport, poison control center resources, and ultimate emergency department and intensive care management. Pediatric Toxicology Dr. James Burhop Pediatric Emergency Medicine Children’s Hospital of the Kings Daughters Objectives • Epidemiology • History of Poisoning • Review initial assessment of the child with a possible ingestion • General management principles for toxic exposures • Case Based (12 common pediatric cases) • Emerging drugs of abuse • Cathinones, Synthetics, Salvia, Maxy/MCAT, 25I, Kratom Epidemiology • 55 Poison Centers serving 295 million people • 2.3 million exposures in 2011 – 39% are children younger than 3 years – 52% in children younger than 6 years • 1-800-222-1222 2011 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System Introduction • 95% decline in the number of pediatric poisoning deaths since 1960 – child resistant packaging – heightened parental awareness – more sophisticated interventions – poison control centers Epidemiology • Unintentional (1-2 -

Information to Users
The direct and modulatory antinociceptive actions of endogenous and exogenous opioid delta agonists Item Type text; Dissertation-Reproduction (electronic) Authors Vanderah, Todd William. Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 04/10/2021 00:14:57 Link to Item http://hdl.handle.net/10150/187190 INFORMATION TO USERS This ~uscript }las been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely. event that the author did not send UMI a complete mannscript and there are missing pages, these will be noted Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginnjng at the upper left-hand comer and contimJing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. -

Pharmacotherapy, Drug-Drug Interactions and Potentially
medRxiv preprint doi: https://doi.org/10.1101/2021.03.31.21254518; this version posted April 6, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Pharmacotherapy, drug-drug interactions and potentially inappropriate medication in depressive disorders Jan Wolff1,2,3, Pamela Reißner4, Gudrun Hefner5, Claus Normann2, Klaus Kaier6, Harald Binder6, Christoph Hiemke7, Sermin Toto8, Katharina Domschke2, Michael Marschollek1, Ansgar Klimke4,9 1 Peter L. Reichertz Institute for Medical Informatics of TU Braunschweig and Hannover Medical School, Germany. 2 Department of Psychiatry and Psychotherapy, Medical Center - University of Freiburg, Faculty of Medicine, University of Freiburg, Freiburg, Germany. 3 Evangelical Foundation NeuerKerode, Germany. 4 Vitos Hochtaunus, Friedrichsdorf, Germany. 5 Vitos Clinic for Forensic Psychiatry, Eltville, Germany 6 Institute of Medical Biometry and Statistics, Medical Center - University of Freiburg, Faculty of Medicine, University of Freiburg, Germany. 7 Department of Psychiatry and Psychotherapy, University Medical Center Mainz, Germany. 8 Department of Psychiatry, Social Psychiatry and Psychotherapy, Hannover Medical School, Germany. 9 Heinrich-Heine-University Düsseldorf, Germany. ___ Correspondence Dr. Jan Wolff, Peter L. Reichertz Institute for Medical Informatics of TU Braunschweig and Hannover Medical School, Hannover, Germany. Address: Karl- Wiechert-Allee 3, 30625 Hannover. Email: [email protected], wolff.jan@mh- hannover.de, ORCID: https://orcid.org/0000-0003-2750-0606 Key words (MeSH) Depression, Polypharmacy, Antidepressants, Hospitals, Drug Interactions, Psychiatry NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice.