Valvuloplasty Fact Sheet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Health Facilities and Services Review Board
STATE OF ILLINOIS HEALTH FACILITIES AND SERVICES REVIEW BOARD 525 WEST JEFFERSON ST. • SPRINGFIELD, ILLINOIS 62761 •(217) 782-3516 FAX: (217) 785-4111 DOCKET NO: BOARD MEETING: PROJECT NO: September 14, 2021 21-016 PROJECT COST: H-04 FACILITY NAME: CITY: Original: $170,520,604 NorthShore Glenbrook Hospital Glenview TYPE OF PROJECT: Substantive HSA: VII PROJECT DESCRIPTION: The Applicant [NorthShore University HealthSystem] is asking the State Board approve establishment of an open-heart surgery category of service, the addition of 8 cardiac cath labs, and the addition of 6 surgery rooms at Glenbrook Hospital in Glenview, Illinois. The cost of the project is $170,520,604. The expected completion date is December 31, 2024. The purpose of the Illinois Health Facilities Planning Act is to establish a procedure (1) which requires a person establishing, constructing or modifying a health care facility, as herein defined, to have the qualifications, background, character and financial resources to adequately provide a proper service for the community; (2) that promotes the orderly and economic development of health care facilities in the State of Illinois that avoids unnecessary duplication of such facilities; and (3) that promotes planning for and development of health care facilities needed for comprehensive health care especially in areas where the health planning process has identified unmet needs. Cost containment and support for safety net services must continue to be central tenets of the Certificate of Need process. (20 ILCS 3960/2) The Certificate of Need process required under this Act is designed to restrain rising health care costs by preventing unnecessary construction or modification of health care facilities. -

Surgical Management of Transcatheter Heart Valves
Corporate Medical Policy Surgical Management of Transcatheter Heart Valves File Name: surgica l_management_of_transcatheter_heart_valves Origination: 1/2011 Last CAP Review: 6/2021 Next CAP Review: 6/2022 Last Review: 6/2021 Description of Procedure or Service As the proportion of older adults increases in the U.S. population, the incidence of degenerative heart valve disease also increases. Aortic stenosis and mitra l regurgita tion are the most common valvular disorders in adults aged 70 years and older. For patients with severe valve disease, heart valve repair or replacement involving open heart surgery can improve functional status and qua lity of life. A variety of conventional mechanical and bioprosthetic heart valves are readily available. However, some individuals, due to advanced age or co-morbidities, are considered too high risk for open heart surgery. Alternatives to the open heart approach to heart valve replacement are currently being explored. Transcatheter heart valve replacement and repair are relatively new interventional procedures involving the insertion of an artificial heart valve or repair device using a catheter, rather than through open heart surgery, or surgical valve replacement (SAVR). The point of entry is typically either the femoral vein (antegrade) or femora l artery (retrograde), or directly through the myocardium via the apical region of the heart. For pulmonic and aortic valve replacement surgery, an expandable prosthetic heart valve is crimped onto a catheter and then delivered and deployed at the site of the diseased native valve. For valve repair, a small device is delivered by catheter to the mitral valve where the faulty leaflets are clipped together to reduce regurgitation. -
Severe Aortic Stenosis and the Valve Replacement Procedure
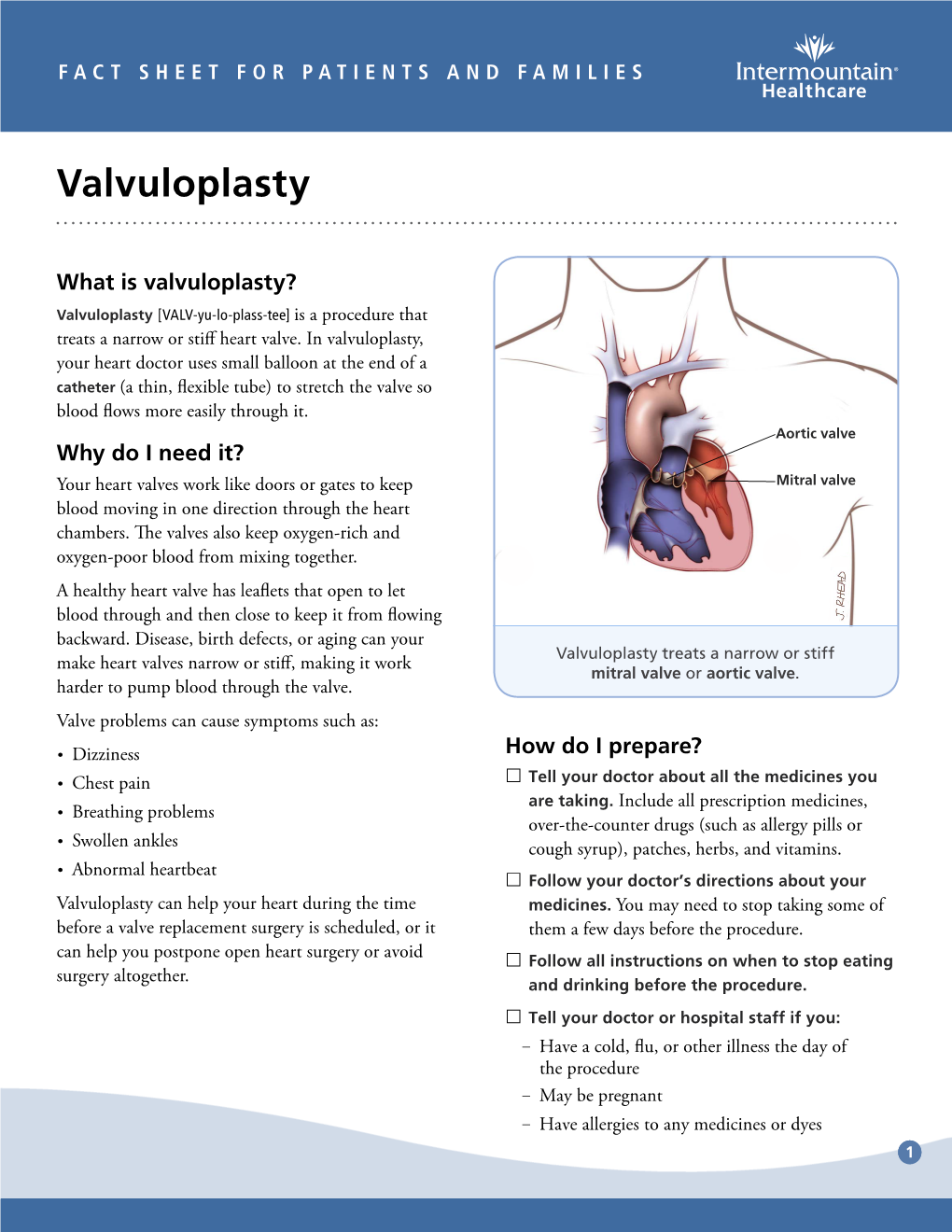
Severe Aortic Stenosis and the Valve Replacement Procedure A Guide for Patients and their Families If you’ve been diagnosed with severe aortic stenosis, you probably have a lot of questions and concerns. The information in this booklet will help you learn more about your heart, severe aortic stenosis, and treatment options. Your heart team will recommend which treatment option is best for you. Please talk with them about any questions you have. Table of Contents 4 About Your Heart 5 What Is Severe Aortic Stenosis? 5 What Causes Severe Aortic Stenosis? 7 What Are the Symptoms of Severe Aortic Stenosis? 8 Treatment Options for Severe Aortic Stenosis 10 Before a TAVR Procedure 12 What Are the Risks of TAVR? 2 3 About Your Heart What Is Severe See the difference between healthy and The heart is a muscle about the size of your fist. It is a pump that works nonstop to Aortic Stenosis? diseased valves send oxygen-rich blood throughout your entire body. The heart is made up of four The aortic valve is made up of two or three chambers and four valves. The contractions (heartbeats) of the four chambers push Healthy Valve the blood through the valves and out to your body. tissue flaps, called leaflets. Healthy valves open at every heart contraction, allowing blood to flow forward to the next chamber, and then close tightly to prevent blood from backing Pulmonic controls the flow of Aortic controls the flow of blood up. Blood flows in one direction only. This is Valve blood to the lungs Valve out of your heart to the important for a healthy heart. -

Transcatheter Mitral and Pulmonary Valve Therapy
Journal of the American College of Cardiology Vol. 53, No. 20, 2009 © 2009 by the American College of Cardiology Foundation ISSN 0735-1097/09/$36.00 Published by Elsevier Inc. doi:10.1016/j.jacc.2008.12.067 FOCUS ISSUE: VALVULAR HEART DISEASE Transcatheter Mitral and Pulmonary Valve Therapy Nicolo Piazza, MD,* Anita Asgar, MD,† Reda Ibrahim, MD,‡ Raoul Bonan, MD‡ Rotterdam, the Netherlands; London, United Kingdom; and Montreal, Quebec, Canada As the percentage of seniors continues to rise in many populations around the world, the already challenging burden of valvular heart disease will become even greater. Unfortunately, a significant proportion of patients with moderate-to-severe valve disease are refused or denied valve surgery based on age and/or accompanying comorbidities. Furthermore, because of advances in pediatric cardiology, the number of adult patients with con- genital heart disease is on the rise and over time, these patients will likely require repeat high-risk surgical pro- cedures. The aim of transcatheter valve therapies is to provide a minimally invasive treatment that is at least as effective as conventional valve surgery and is associated with less morbidity and mortality. The objective of this review was to provide an update on the clinical status, applicability, and limitations of transcatheter mitral and pulmonary valve therapies. (J Am Coll Cardiol 2009;53:1837–51) © 2009 by the American College of Cardiology Foundation The prevalence of moderate-to-severe valvular heart disease ing prevalence of adults with congenital heart disease. It is is highly age-dependent, ranging from an estimated 0.7% in safe to assume that some of these patients will require 18- to 44-year-olds in the U.S. -

(12) United States Patent (10) Patent No.: US 8,187,323 B2 Mortier Et Al
USOO8187323B2 (12) United States Patent (10) Patent No.: US 8,187,323 B2 Mortier et al. (45) Date of Patent: May 29, 2012 (54) VALVE TO MYOCARDIUM TENSION 4,372,293 A 2/1983 Vijil-Rosales MEMBERS DEVICE AND METHOD 4.409,974 A 10, 1983 Freedland 4,536,893 A 8, 1985 Parravicini 4,690,134 A 9/1987 Snyders (75) Inventors: Todd J. Mortier, Minneapolis, MN 4,705,040 A 1 1/1987 Mueller et al. (US); Cyril J. Schweich, Jr., St. Paul, 4,936,857 A 6, 1990 Kulik MN (US) 4,944,753. A 7/1990 Burgess et al. 4,960,424 A 10, 1990 Grooters (73) Assignee: Edwards Lifesciences, LLC, Irvine, CA 4,997.431 A 3, 1991 Isner et al. US 5,104,407 A 4, 1992 Lam et al. (US) 5,106,386 A 4, 1992 Isner et al. 5,131,905 A 7, 1992 Grooters (*) Notice: Subject to any disclaimer, the term of this RE34,021 E 8, 1992 Mueller et al. patent is extended or adjusted under 35 5,169,381 A 12/1992 Snyders U.S.C. 154(b) by 205 days. (Continued) (21) Appl. No.: 09/981,790 FOREIGN PATENT DOCUMENTS (22) Filed: Oct. 19, 2001 DE 36 14292 c 111987 (Continued) (65) Prior Publication Data OTHER PUBLICATIONS US 20O2/OO2908O A1 Mar. 7, 2002 Dickstein et al., “Heart Reduction Surgery: An Analysis of the Impact Related U.S. Application Data on Cardiac Function.” The Journal of Thoracic and Cardiovascular (63) Continuation of application No. 08/992.316, filed on Surgery, vol. -

Surgery for Acquired Heart Disease
View metadata, citation and similar papers at core.ac.uk brought to you byCORE provided by Elsevier - Publisher Connector SURGERY FOR ACQUIRED HEART DISEASE EARLY RESULTS WITH PARTIAL LEFT VENTRICULECTOMY Patrick M. McCarthy, MD a Objective: We sought to determine the role of partial left ventriculectomy in Randall C. Starling, MD b patients with dilated cardiomyopathy. Methods: Since May 1996 we have James Wong, MBBS, PhD b performed partial left ventriculectomy in 53 patients, primarily (94%) in Gregory M. Scalia, MBBS b heart transplant candidates. The mean age of the patients was 53 years Tiffany Buda, RN a Rita L. Vargo, MSN, RN a (range 17 to 72 years); 60% were in class IV and 40% in class III. Marlene Goormastic, MPH c Preoperatively, 51 patients were thought to have idiopathic dilated cardio- James D. Thomas, MD b myopathy, one familial cardiomyopathy, and one valvular cardiomyopathy. Nicholas G. Smedira, MD a As our experience accrued we increased the extent of left ventriculectomy James B. Young, MD b and more complex mitral valve repairs. For two patients mitral valve replacement was performed. For 51 patients the anterior and posterior mitral valve leaflets were approximated (Alfieri repair); 47 patients also had ring posterior annuloplasty. In 27 patients (5!%) one or both papillary muscles were divided, additional left ventricular wall was resected, and the papillary muscle heads were reimplanted. Results: Echocardiography showed a significant decrease in left ventricular dimensions after resection (8.3 cm to 5.8 cm), reduction in mitral regurgitation (2.8+ to 0), and increase in forward ejection fraction (15.7% to 32.7%). -

Leapfrog Hospital Survey Hard Copy
Leapfrog Hospital Survey Hard Copy QUESTIONS & REPORTING PERIODS ENDNOTES MEASURE SPECIFICATIONS FAQS Table of Contents Welcome to the 2016 Leapfrog Hospital Survey........................................................................................... 6 Important Notes about the 2016 Survey ............................................................................................ 6 Overview of the 2016 Leapfrog Hospital Survey ................................................................................ 7 Pre-Submission Checklist .................................................................................................................. 9 Instructions for Submitting a Leapfrog Hospital Survey ................................................................... 10 Helpful Tips for Verifying Submission ......................................................................................... 11 Tips for updating or correcting a previously submitted Leapfrog Hospital Survey ...................... 11 Deadlines ......................................................................................................................................... 13 Deadlines for the 2016 Leapfrog Hospital Survey ...................................................................... 13 Deadlines Related to the Hospital Safety Score ......................................................................... 13 Technical Assistance....................................................................................................................... -

Heart Valve Surgery Factsheet
Heart information Heart valve surgery Contents Page 1 What are heart valves? Page 3 What is heart valve surgery? Page 3 Valve repair Page 4 Valve replacement Page 4 What happens during heart valve surgery? Page 5 Why do I need heart valve surgery? Page 6 What will happen after heart valve surgery? Page 6 Will I feel pain after the operation? Page 6 How long will I have to stay in hospital? Page 7 How long will it take to recover from heart valve surgery? Page 7 When can I start eating again? Page 8 What should I be eating? Page 8 What if I am constipated? Page 8 How active can I be? Page 9 When can I be more physically active? Page 9 When can I have sex? Page 10 Why am I so tired? Page 10 Why do I feel great one day, but dreadful the next? Page 10 When can I return to work? Page 10 Palpitations Page 11 Heart attack Page 12 Endocarditis Page 12 Will I need to take medicine? Page 13 Important things to remember about anti-coagulant medicine Page 14 Warfarin and food Page 15 What should I talk to my doctor about? Page 16 Glossary What are heart valves? For more Heart valves are like one-way doors that control the direction of blood flow between the four chambers of the heart. There are information two upper chambers (the atria) and two lower chambers (the on this topic ventricles) (see the diagram on page 2). The atria receive blood please call from the body and pump it into the ventricles. -

Medicare National Coverage Determinations Manual, Part 1
Medicare National Coverage Determinations Manual Chapter 1, Part 1 (Sections 10 – 80.12) Coverage Determinations Table of Contents (Rev. 10838, 06-08-21) Transmittals for Chapter 1, Part 1 Foreword - Purpose for National Coverage Determinations (NCD) Manual 10 - Anesthesia and Pain Management 10.1 - Use of Visual Tests Prior to and General Anesthesia During Cataract Surgery 10.2 - Transcutaneous Electrical Nerve Stimulation (TENS) for Acute Post- Operative Pain 10.3 - Inpatient Hospital Pain Rehabilitation Programs 10.4 - Outpatient Hospital Pain Rehabilitation Programs 10.5 - Autogenous Epidural Blood Graft 10.6 - Anesthesia in Cardiac Pacemaker Surgery 20 - Cardiovascular System 20.1 - Vertebral Artery Surgery 20.2 - Extracranial - Intracranial (EC-IC) Arterial Bypass Surgery 20.3 - Thoracic Duct Drainage (TDD) in Renal Transplants 20.4 – Implantable Cardioverter Defibrillators (ICDs) 20.5 - Extracorporeal Immunoadsorption (ECI) Using Protein A Columns 20.6 - Transmyocardial Revascularization (TMR) 20.7 - Percutaneous Transluminal Angioplasty (PTA) (Various Effective Dates Below) 20.8 - Cardiac Pacemakers (Various Effective Dates Below) 20.8.1 - Cardiac Pacemaker Evaluation Services 20.8.1.1 - Transtelephonic Monitoring of Cardiac Pacemakers 20.8.2 - Self-Contained Pacemaker Monitors 20.8.3 – Single Chamber and Dual Chamber Permanent Cardiac Pacemakers 20.8.4 Leadless Pacemakers 20.9 - Artificial Hearts And Related Devices – (Various Effective Dates Below) 20.9.1 - Ventricular Assist Devices (Various Effective Dates Below) 20.10 - Cardiac -

Transcatheter Aortic Valve Replacement
What is TAVR? Cardiac Catheterization: Important things to know that will help you get ready Transcatheter Aortic Valve Replacement (TAVR) is a procedure Your doctor will tell if you need to stop eating or drinking to fix the aortic valve without taking out the old valve. A TAVR before your procedure. Your doctor also will tell you if you does not need open heart surgery and the heart does not need must stop taking any medications before the procedure. to be stopped. Catheterization Lab In the Pre-Operative (Pre-Op) Room before your The surgeon puts a catheter (thin tube) into an artery in your Cardiac Catheterization upper leg or through a small cut in your chest. The catheter will • You will wear a hospital gown. We will ask you to take off all Transcatheter Aortic Valve carry a new valve to your heart. your clothing (even underwear), jewelry, dentures, glasses, Replacement (TAVR) hearing aids, etc. • An intravenous line (IV) may be put into a vein in your arm • We will prepare and clean the catheter site (where the catheter goes into your body). We will clean your skin with a special wash that kills germs. We may need to trim body hair. • We will ask you to empty your bladder (pee) before your procedure After Your Cardiac Catheterization • You may be on bed rest (lying flat) for 2 to 6 hours. To lower the risk of bleeding, we do not want you to bend your body at the catheter site (where the catheter went into your body) • Your nurse will often check your vital signs (blood pressure, heart rate, temperature) and catheter site • You must use a urinal or bed pan until you can safely stand and walk to the bathroom • While you are healing, do not do strenuous exercise (such as running or lifting weights). -

A Focus on Valve-Sparing Ascending Aortic Aneurysm Repair Newyork
ADVANCES IN CARDIOLOGY, INTERVENTIONAL CARDIOLOGY, AND CARDIOVASCULAR SURGERY Affiliated with Columbia University College of Physicians and Surgeons and Weill Cornell Medical College A Focus on Valve-Sparing NOVEMBER/DECEMBER 2014 Ascending Aortic Aneurysm Repair Emile A. Bacha, MD The most frequent location for aneurysms in the Chief, Division of Cardiac, chest occurs in the ascending aorta – and these Thoracic and Vascular Surgery aneurysms are often associated with either aortic NewYork-Presbyterian/Columbia stenosis or aortic insufficiency, especially when the University Medical Center aneurysm involves a bicuspid aortic valve. Director, Congenital and Pediatric Cardiac Surgery “We know that patients who have enlarged NewYork-Presbyterian Hospital aortas or aneurysms of the ascending aorta are at [email protected] great risk for one of two major life-threatening events: an aortic rupture or an aortic dissection,” Allan Schwartz, MD says Leonard N. Girardi, MD, Director of Chief, Division of Cardiology Thoracic Aortic Surgery in the Department of NewYork-Presbyterian/Columbia Cardiothoracic Surgery, NewYork-Presbyterian/ University Medical Center Weill Cornell Medical Center. “Dissection of the Valve-sparing ascending aortic aneurysm repair [email protected] inner lining of the wall of the blood vessel can also lead to rupture or other complications down last 15 years, the Aortic Surgery Program at Weill O. Wayne Isom, MD the line. For example, as the tear extends it may Cornell has been aggressively pursuing the devel- Cardiothoracic Surgeon-in-Chief NewYork-Presbyterian/ affect the vessels that supply the brain or the opment of a procedure that would enable surgeons Weill Cornell Medical Center coronary arteries or cause tremendous damage to to spare the patient’s native valve. -

About Mitral Valve Repair
About Mitral Valve Repair What It Is What To Expect Definition Prior to Procedure The mitral valve is on the left side of the heart. It allows Your doctor will likely do the following: blood to flow from the left upper chamber into the left • Physical exam lower chamber. When the valve is not working well, it • Chest X-ray may need to be repaired. • Lab work • Echocardiogram Reasons for Procedure • Electrocardiogram (ECG, EKG) Mitral valve repair is the best option for many patients • Cardiac catheterization with degenerative mitral valve disease leading to regurgitation (leakage). Compared to valve replacement, Talk to your doctor about your medicines, herbs, or mitral valve repair provides better outcomes leaving supplements. You may be asked to stop taking some normally functioning tissue, which resists infection more medicines up to one week before the procedure, such as: effectively and usually eliminates the need for long-term • Blood-thinning drugs, such as warfarin (Coumadin) use of blood thinners. • Anti-platelet drugs, such as clopidogrel (Plavix) • Diabetes medications, such as metformin Possible Complications (Glucophage) If you are planning to have a mitral valve repair, your doctor will review a list of possible complications, which Your doctor may also ask you to: may include: • Eat a light meal the night before. Do not eat or drink • Infections anything after midnight. • Bleeding • Arrange for a ride to and from the hospital. • Stroke • Arrange for help at home after the procedure. • Damage to other organs, such as the kidneys Anesthesia • Irregular heart rhythm You will have a general anesthetic. You will be asleep • Death during the procedure.